Understanding the distinctions between insulin resistance and prediabetes is critical for healthcare providers as well as individuals at risk of metabolic disorders. While these terms are frequently used interchangeably, they actually represent distinct stages in glucose dysregulation.
Insulin resistance occurs when cells don’t respond effectively to insulin production resulting in an increase in its production prediabetes is when blood sugar levels remain elevated but don’t qualify as a diabetes diagnosis.
This article seeks to outline these distinctions through definitions, symptoms, causes, and diagnostic criteria so as to more effectively inform diagnosis and treatment strategies.
Definition of Insulin Resistance
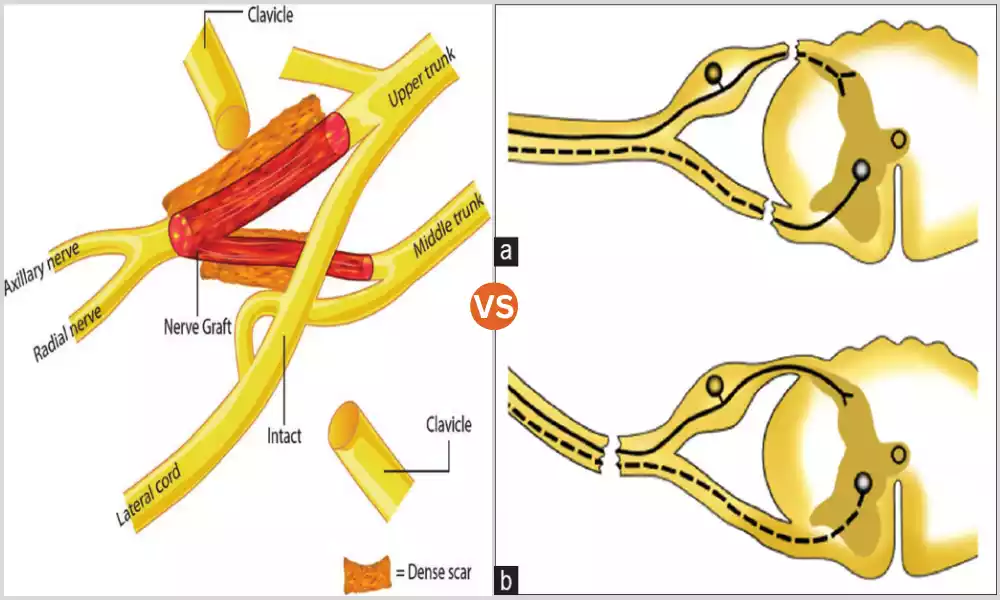
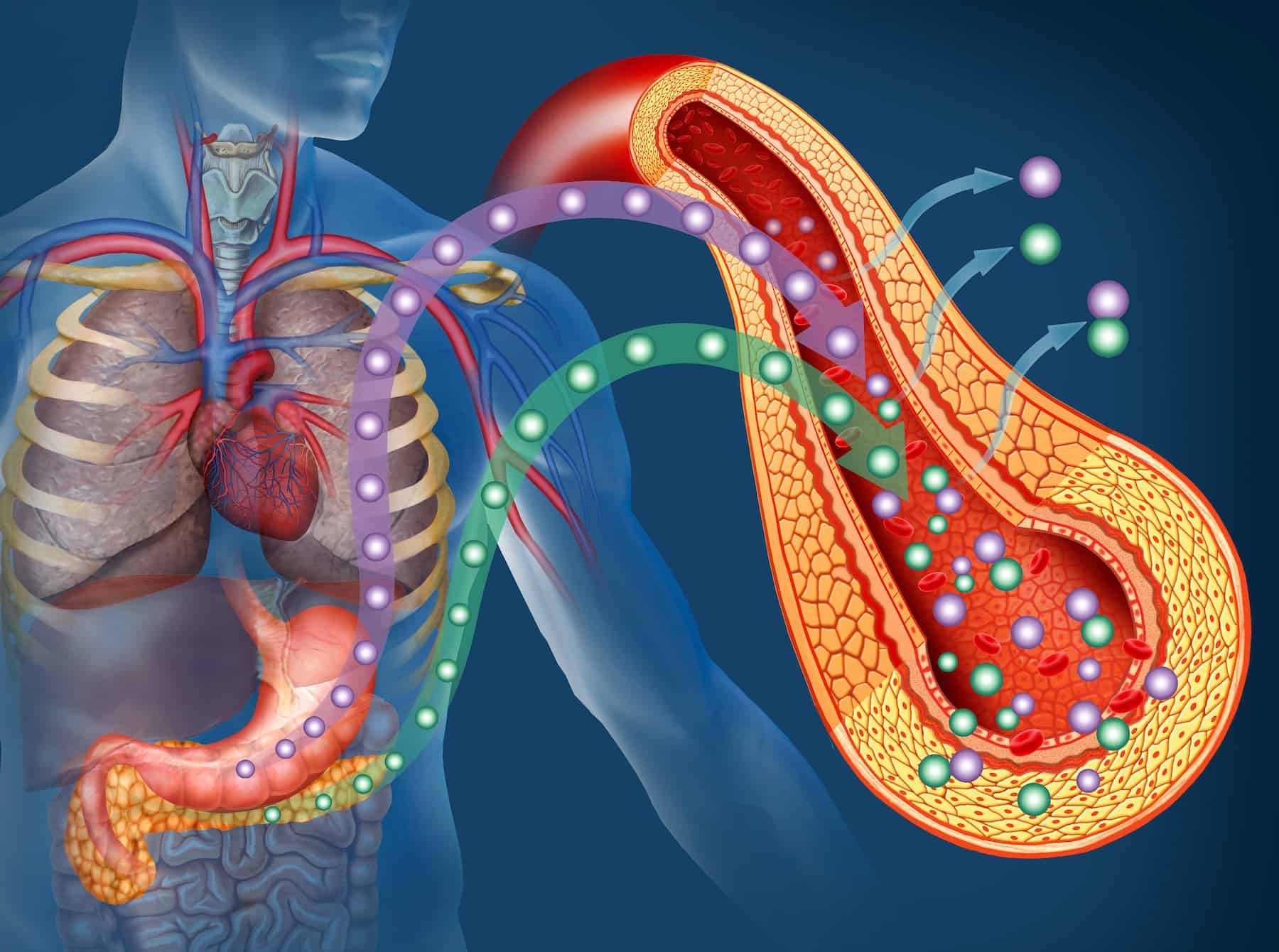
Insulin resistance is a metabolic condition characterized by reduced responsiveness of cells such as muscle, fat, and liver cells to insulin hormone. When functioning normally, this system helps cells take in glucose from the bloodstream, thus controlling blood sugar levels, but with resistance, the system becomes ineffective Cells do not respond as expected when sensing insulin signals resulting in reduced glucose uptake and regulation.
As a result, the pancreas may produce more insulin to compensate for reduced effectiveness, leading to hyperinsulinemia – elevated blood insulin levels. Unfortunately, even though more insulin may be produced than before, blood sugar levels may still gradually rise due to inefficient utilization by cells of available glucose – creating an endless cycle of metabolic dysfunction and creating further issues with your health.
Insulin resistance can often serve as a precursor to more serious conditions, including prediabetes and type 2 diabetes, often coexisting with obesity, high blood pressure, and elevated triglyceride levels.
As part of metabolic syndrome – an umbrella of conditions that increases your risk for heart disease, stroke, and type 2 diabetes – insulin resistance may become increasingly problematic over time.
Definition of Prediabetes
Prediabetes is a metabolic condition in which blood sugar levels exceed normal but do not meet the criteria to be classified as type 2 diabetes. It serves as an early warning sign or intermediate stage on the journey toward full diabetes with prediabetes still producing some amount of insulin but possibly not enough to maintain healthy levels due to decreased sensitivity, and serves as an intermediate step toward full diabetes.
Prediabetes often has no identifiable symptoms, making it easy for it to go undetected and increase an individual’s risk for type 2 diabetes as well as cardiovascular conditions like heart attack and stroke.
People living with prediabetes face increased risks both of type 2 diabetes development as well as cardiovascular illnesses like heart attack and stroke.
Diabetes can be identified through several tests, including the Fasting Plasma Glucose Test, Oral Glucose Tolerance Test, and Hemoglobin A1C Test. These assessments measure glucose concentration in various conditions of blood circulation to help healthcare providers assess how well their body is managing blood sugar.
Early diagnosis and management of prediabetes can halt or even reverse its progression, decreasing your risk for more serious conditions like type 2 diabetes, cardiovascular diseases, and other complications.
Lifestyle modifications including diet modification, exercise regimen, and possibly medication may be suggested for managing prediabetes successfully.

Comparison Table of Insulin Resistance and Prediabetes
| Feature | Insulin Resistance | Prediabetes |
|---|---|---|
| Definition | Reduced cellular responsiveness to insulin, leading to elevated insulin levels (hyperinsulinemia). | Elevated blood sugar levels that are not high enough for a type 2 diabetes diagnosis. |
| Symptoms | Often asymptomatic, may include fatigue, weight gain, and high blood pressure. | Usually asymptomatic, but may include increased thirst and urination if it progresses. |
| Causes | Lifestyle factors, genetics, obesity, lack of physical activity. | Similar to insulin resistance, but also age, family history, and hormonal changes. |
| Diagnostic Tests | Insulin level tests, Homeostatic Model Assessment for Insulin Resistance (HOMA-IR), are often discovered during other tests. | Fasting Plasma Glucose, Oral Glucose Tolerance Test, Hemoglobin A1C. |
| Treatment | Lifestyle changes, Metformin may be prescribed. | Lifestyle changes, Sometimes metformin is prescribed to prevent progression to diabetes. |
| Associated Risks | Increased risk of developing prediabetes and type 2 diabetes, as well as cardiovascular diseases. | Higher risk of progressing to type 2 diabetes and associated complications like heart disease. |
| Long-term Outlook | Can lead to prediabetes or type 2 diabetes if not managed. | High likelihood of progressing to type 2 diabetes if not managed. |
| Management Strategy | Lifestyle changes such as diet and exercise, medication may be considered. | Intensive lifestyle modification and medication may be prescribed if high risk of diabetes. |
Importance of understanding the difference between effective diagnosis and management
Below are several key reasons why it is crucial to recognize these differences for effective diagnosis and management of chronic illnesses.
Insulin Resistance Leads to Prediabetes
Insulin resistance often precedes prediabetes, and then type 2 diabetes. Recognizing these subtle differences allows for earlier interventions that could stop its progress into more serious states.
Targeted Treatment
Treatment for insulin resistance typically centers on lifestyle modifications to increase its sensitivity, prediabetes often requires more aggressive action involving medications like metformin to stave off diabetes from emerging.
Risk Stratification
Healthcare providers who can accurately differentiate between insulin resistance and prediabetes can use it as a basis to more precisely stratify patient risk for conditions like cardiovascular disease, providing more targeted preventative measures and measures of protection.
Resource Allocation
Gaining an in-depth knowledge of various conditions allows healthcare systems to more efficiently allocate their resources. For instance, someone suffering from insulin resistance might benefit more from lifestyle coaching while those diagnosed with prediabetes might require more intensive medical monitoring.
Customized Care
Diagnosing and managing insulin resistance differs significantly from prediabetes, acknowledging these variations allows for more personalized care that may prove more effective than adopting a one-size-fits-all approach.
Monitoring and Follow-Up
Insulin resistance and prediabetes each have unique diagnostic criteria, so knowing which condition you are treating helps in selecting appropriate follow-up tests and monitoring plans.
Early Diagnosis and Treatment Can Improve Quality of Life
Early diagnosis and tailored treatment of either condition can drastically enhance the quality of life, helping avoid complications such as fatigue, weight gain, and the emotional impact of living with chronic illnesses.
Public Health Implications
Greater awareness of metabolic conditions paves the way for more targeted public health policies, educational programs, awareness campaigns, and preventive measures that are more tailored toward each person.
Who is more likely to develop insulin resistance or prediabetes?
Common Risk Factors for Both Conditions
Age is often more of a factor. Obesity – particularly abdominal obesity is often considered a strong risk factor.
Physical Inactivity: Leading an inactive lifestyle increases the risks involved.
Family History and Ethnicity are major risk factors. Ethnic groups such as African American, Hispanic, Native American, and Asian American populations are at greater risk. Additional Factors that Increase Insulin Resistance
Insulin resistance is often evident among people living with hypertension. Elevated levels of Triglycerides may signal increased risk.
Low HDL Cholesterol: Lower levels of good “LDL” cholesterol could indicate risk.
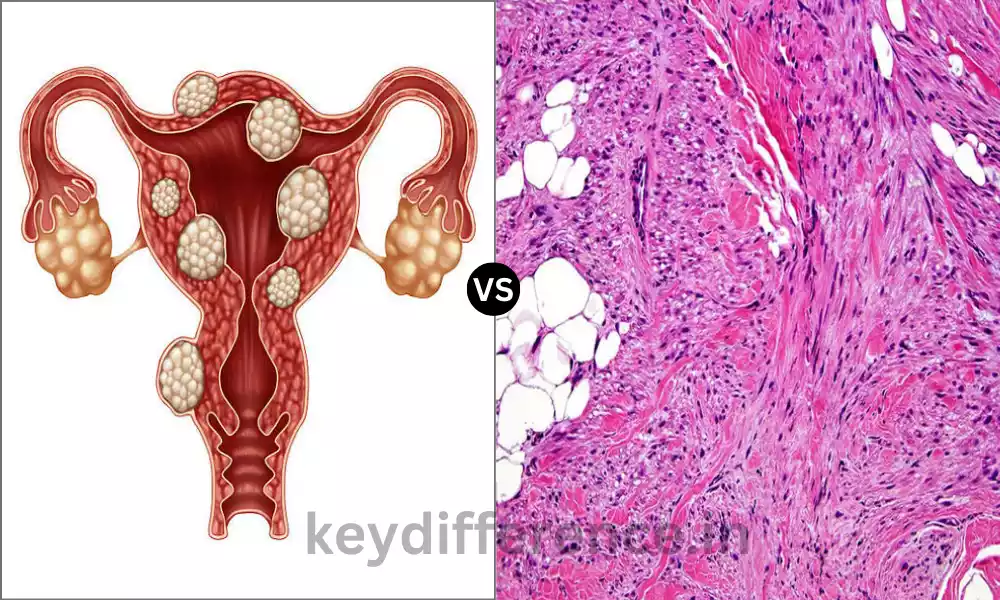
Polycystic Ovary Syndrome (PCOS): Women diagnosed with PCOS tend to be insulin resistant.
Smoking: Cigarette smoking has been shown to increase insulin resistance and put individuals at greater risk of prediabetes.
Other Factors Contributing to Prediabetes
Gestational Diabetes: Women who experience gestational diabetes have an increased risk for prediabetes.
Hormonal Changes: Conditions like hypothyroidism can contribute significantly to prediabetes development.
Sleep Disorders: Studies have linked conditions like Sleep Apnea with an increased risk of prediabetes.
Special Cases Children and Adolescents: Insulin resistance and prediabetes have long been considered adult conditions, however, due to an increase in childhood obesity cases they are now increasingly being diagnosed in younger individuals.
Pregnant Women: Gestational diabetes or insulin resistance during gestation increases their risk for both conditions post-pregnancy.
Medical Conditions with an Increased Risk:
Metabolic Syndrome: This condition refers to a collection of factors that significantly increase the risk for insulin resistance and prediabetes, as well as heart disease.
People living with cardiovascular issues are especially at risk.
Fatty Liver Disease: Fatty liver disease can increase your risk of insulin resistance and lead to prediabetes.
Overall, those at greater risk for these conditions tend to have lifestyle habits like poor diet and lack of exercise that put them at a greater risk.
Genetic predispositions or other medical conditions may also increase risks, but it’s important to remember that anyone can develop insulin resistance or prediabetes even without these risk factors.
As such, screenings and adopting healthy practices are recommended. Therefore, regular screenings as well as leading a healthy life are highly recommended.
What causes insulin resistance and prediabetes?
Although prediabetes and insulin resistance are closely linked diseases that are often co-existing and have distinct, but interconnected sets of factors. Understanding the causative factors that cause these conditions will help guide prevention and treatment strategies.
Common Causes for Both Conditions
Lifestyle Factors
- Bad Diet Consumption of high amounts of refined carbs, sugars, and unhealthy fats may cause an increase in weight and metabolic imbalance.
- A lack of physical activity Sedentary behavior is strongly linked with insulin resistance. It can also increase the levels of blood sugar.
Genetic Predisposition
- A family background of metabolic disorders or type 2 diabetes could increase the risk of both conditions.
Obesity
- Weight gain, especially in the abdominal region is a major risk aspect. The fat cells that line the abdomen are active metabolically and may cause insulin resistance.
Age
- The older population is generally more susceptible, but these ailments are being recognized in younger people also.
Ethnicity
- People with particular ethnic backgrounds, including African American, Hispanic, Native American, and Asian American are more at risk.
Additional Causes Specific to Insulin Resistance
Hormonal Imbalance
- Conditions such as Polycystic Ovary Syndrome (PCOS) for women can cause insulin resistance.
High Blood Pressure
- Hypertension is linked to an increased likelihood in developing diabetes resistance.
High Triglycerides and Low HDL
- A deficiency in blood lipid levels could make insulin less efficient.
Smoking
- Tobacco use can exacerbate insulin resistance.
Additional Causes Specific to Prediabetes
Hormonal Changes
- Hormonal imbalances, like hypothyroidism, may contribute to prediabetes.
Pregnancy
- Women who suffer from gestational diabetes are more likely to develop prediabetes and later, type 2 diabetes.
Sleep Disorders
- Sleep apnea and other sleep disorders have been associated with prediabetes likely due to hormone imbalances and stress due to poor sleep.
Underlying Medical Conditions
- Certain illnesses and medications may result in or worsen prediabetes and insulin resistance. For example, glucocorticoid medications and antipsychotic medications can alter the sensitivity of insulin.
Environmental Factors
- Chemicals that cause endocrine disruption and even chronic stress could be a factor in the onset of these diseases even though research is continuing on these topics.
Reference Books
- “The Blood Sugar Solution: The UltraHealthy Program for Losing Weight, Preventing Disease, and Feeling Great Now!”
- By Mark Hyman
- This book offers a comprehensive program for tackling blood sugar-related health issues like insulin resistance and prediabetes.
- “The Diabetes Code: Prevent and Reverse Type 2 Diabetes Naturally”
- By Jason Fung
- This book discusses lifestyle changes and medical treatments for managing blood sugar disorders.
- “Why We Get Sick: The Hidden Epidemic at the Root of Most Chronic Disease—and How to Fight It”
- By Benjamin Bikman
- The author explores insulin resistance as a key factor in many chronic diseases, offering advice on how to counter it.
Summary
Insulin resistance and prediabetes are two crucial metabolic conditions, often serving as precursors to more serious conditions like type 2 diabetes or cardiovascular issues.
While they share many similarities, understanding their unique traits is critical for effective diagnosis and management. Lifestyle factors, including diet, exercise, and stress management can play an instrumental role in preventing and treating these conditions.
Medical intervention may sometimes be required. Regular screenings and healthcare consultations are vitally important, particularly for individuals at higher risk due to age, genetic predisposition, or coexisting medical conditions.
By taking proactive steps it’s entirely possible to manage these conditions and live healthier lives.