The condition is a widespread chronic medical disease that affects millions of people across the globe. One of the main components of treating diabetes is the choice of the appropriate oral antidiabetic medications.
Of the many kinds of these medicines, Sulfonylureas and Meglitinides are two of the most frequently used choices. We will examine the key distinctions between Meglitinides and Sulfonylureas in relation to their mechanisms of action through to their clinical applications, assisting medical doctors and patients in making informed choices regarding diabetes management.
What are Sulfonylureas?
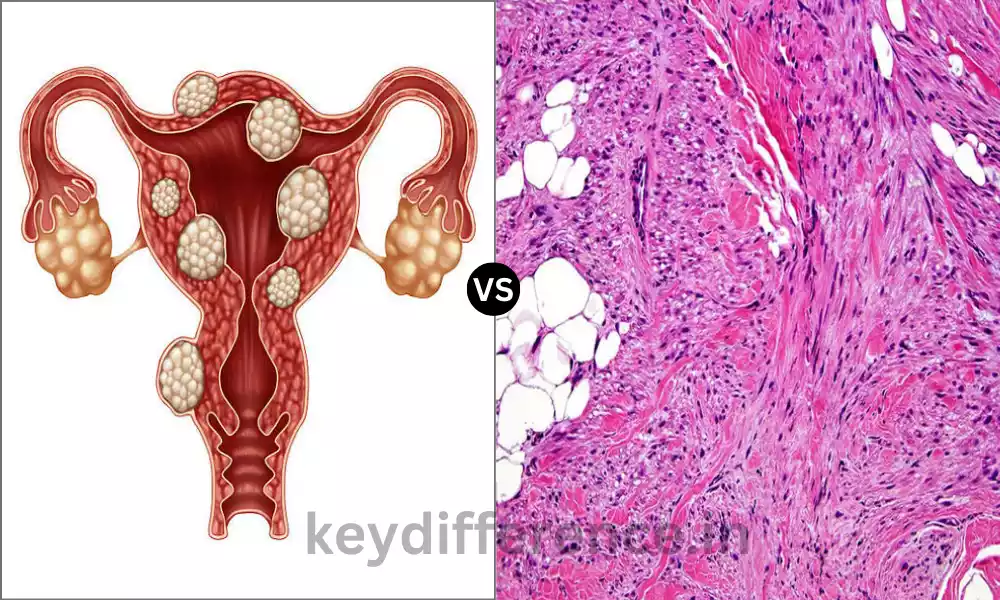
Sulfonylureas are a type of oral antidiabetic medicine which are prescribed in treating diabetes type 2. They work by causing the pancreas ‘ ability to produce more insulin which aids in lowering blood sugar levels of people suffering from diabetes.

They are typically recommended when lifestyle changes or other medications aren’t enough to control blood glucose levels. Examples of sulfonylureas that are commonly used include glyburide, glipizide, as well as glimepiride.
What are Meglitinides?
Meglitinides is a type of oral antidiabetic medication employed in the treatment of Type 2 Diabetes. These medications are effective by stimulating the pancreas’s insulin release, which aids in regulating glucose levels in the blood.

Meglitinides are especially effective in decreasing blood glucose levels following meals. They have an accelerated time to action and are usually taken prior to meals. Meglitinides are the most common examples.
Repaglinide and Nateglinide. They are typically prescribed to people with diabetes who require rapid and rapid insulin release to manage blood sugar spikes after meals.
Comparison Table of Sulfonylureas and Meglitinides
Here’s a simplified comparison table of Sulfonylureas and Meglitinides:
| Aspect | Sulfonylureas | Meglitinides |
|---|---|---|
| Mechanism of Action | Stimulate insulin release from the pancreas | Stimulate insulin release from the pancreas |
| Medications in the Class | Glyburide, Glipizide, Glimepiride, etc. | Repaglinide, Nateglinide |
| Onset and Duration of Action | Generally longer duration of action may cause prolonged hypoglycemia | Shorter duration of action, taken before meals to control post-meal glucose |
| Efficacy in Glycemic Control | Effective at lowering blood glucose levels | Effective at controlling postprandial glucose spikes |
| Common Side Effects | Hypoglycemia, weight gain, GI disturbances | Hypoglycemia, weight gain, GI disturbances |
| Drug Interactions and Cautions | Interact with various medications, caution with other hypoglycemic agents | Fewer drug interactions, less risk of prolonged hypoglycemia |
| Advantages | Established history, low cost, once-daily dosing | Quick action, reduced risk of prolonged hypoglycemia |
| Disadvantages | Risk of hypoglycemia, weight gain, potential for beta-cell exhaustion | Meal timing requirements, less effective for fasting glucose |
| Patient Selection | Considered for individuals with specific needs or when other options fail | Suitable for those with post-meal glucose spikes or irregular meal schedules |
Please note that this is a simplified comparison, and individual patient factors and preferences play a significant role in determining the choice between these two classes of antidiabetic medications. Healthcare providers should make treatment decisions based on a patient’s specific needs and circumstances.
Effectiveness of Sulfonylureas in glycemic control
Sulfonylureas have been used extensively for a long time and are believed to be beneficial in the control of glycemic for people suffering from Type 2 Diabetes. They stimulate the pancreas to release insulin which assists in lowering glucose levels in the blood.
Here are some important points concerning the effectiveness of Sulfonylureas in the control of glycemic levels:
- Blood glucose reduction: Sulfonylureas can effectively reduce blood glucose levels both at rest as well as after-prandial (after mealtimes). This may result in an improvement in HbA1c levels that are a reflection of long-term control over glucose.
- Quick Onset of Action: These drugs usually exhibit a rapid start of action, usually within an hour after having taken an amount. This fast action will help to reduce the rise in blood sugar following meals.
- HbA1c Reduction: The treatment with Sulfonylureas typically results in a significant decrease in HbA1c level. The amount of reduction could differ based on the particular dosage, medication, and the specific patient’s response.
- Long-Term Efficacy: Sulfonylureas are able to help with long-term glycemic control if employed in conjunction with a complete diabetes management program. They are typically considered second-line drugs following lifestyle changes or metformin.
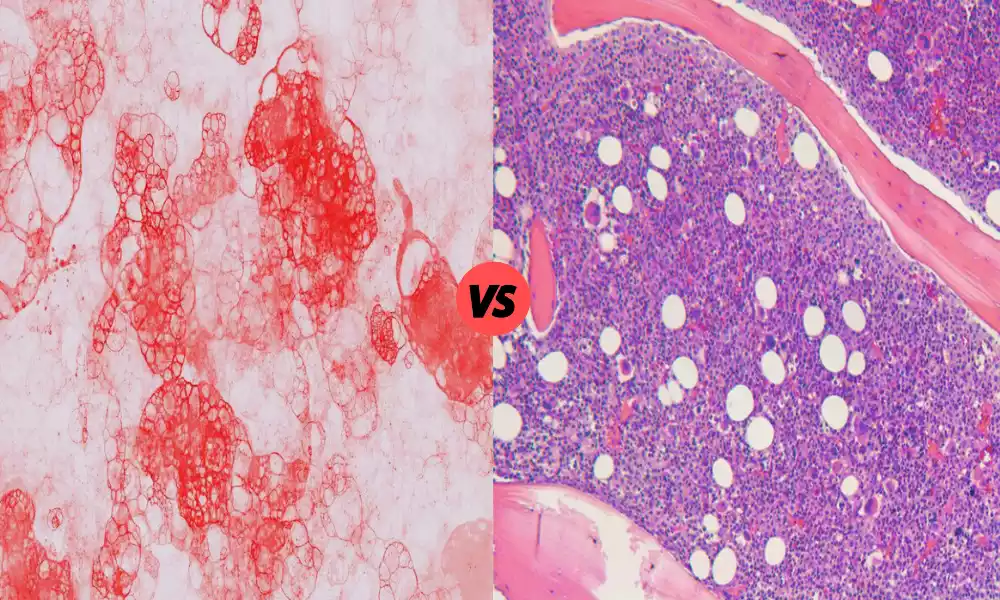
- Effectiveness of Beta-Cell Function: Sulfonylureas function by stimulating the release of insulin from beta cells in the pancreas. They are especially efficient in patients with a beta-cell function that is not fully restored.
- Cheap Cost: The primary benefit of Sulfonylureas is that they’re typically available as generic low-cost drugs, which makes them a feasible choice for a lot of patients.
While Sulfonylureas can be effective in reducing blood sugar levels, they’re associated with the possibility of Hypoglycemia (low levels of blood sugar) and weight increase.
As time goes by their effectiveness could diminish, leading to an issue with beta-cell exhaustion. The choice of an antidiabetic drug that includes Sulfonylureas must be tailored depending on the individual’s requirements, medical history, and risks.
Healthcare professionals typically take into consideration the benefit-risk ratio when prescribing Sulfonylureas to control glycemic levels.
Drug Interactions and Cautions
Sulfonylureas and Meglitinides both classes of anti-diabetic medications have distinct interactions with other drugs, and there are some warnings patients and healthcare professionals must keep in mind.
Here’s a summary of the principal drug interactions and the warnings in each category:
Sulfonylureas:
- Hypoglycemia Risk: Sulfonylureas are known to reduce blood sugar levels in a significant way. In combination with other drugs that reduce blood sugar levels (such as insulin or other oral antidiabetic medications), there is an increased chance of developing hypoglycemia. Monitoring blood glucose closely is vital.
- Alcohol: Consuming alcohol when taking Sulfonylureas may cause developing hypoglycemia. It is important to be cautious with the consumption of alcohol and should avoid eating after drinking alcohol.
- The Symbol for NSAIDs (Non-Steroidal anti-inflammatory drugs): Some NSAIDs such as ibuprofen may alter the actions of Sulfonylureas and cause fluctuations in the blood sugar level. Patients should consult their physician prior to using these medications together.
- CYP2C9 The inhibitors are: Some medications that interfere with this CYP2C9 liver enzyme could increase the levels of specific Sulfonylureas within the body, leading to a greater risk of hypoglycemia.
- Hepatic or renal impairment: Patients who suffer from impaired kidney or liver function could require dosage adjustments due to the metabolism and elimination of Sulfonylureas.
Meglitinides:
- Hypoglycemia Risk: Similar to Sulfonylureas Meglitinides are also associated with the risk of hypoglycemia. This risk is higher when it is taken alongside other medicines that reduce blood sugar levels.
- Food Timing: Meglitinides must be consumed just prior to meals in order to increase insulin release. If you skip a meal or delay it long after taking the medication could increase the risk of developing hypoglycemia.
- CYP2C8 as well as CYP3A4 interactions: Some medications that are metabolized or inhibited by or block CYP2C8, as well as CYP3A4 liver enzymes, could interfere with meglitinides. These interactions could influence the metabolic process of Meglitinides, and increase the chance of developing hypoglycemia or hyperglycemia.
- Renal Impairment: If you have kidney impairment Meglitinides can require adjustments to dosage since the drug is eliminated by the kidneys.
- Liver Function: Patients who suffer from impaired liver function might also require dose adjustments using Meglitinides since they are metabolized primarily within the liver.
It is essential for healthcare professionals to know the full history of medication taken by a patient and any health issues that may be underlying when prescribing Meglitinides or Sulfonylureas.
Patients should also inform healthcare providers of any medications they’re taking, including prescription drugs and supplements, in order to ensure the safe and effective treatment of diabetes and minimize the chance of drug interactions and negative side effects.
Continuous monitoring the blood sugar levels is vital for these medications to reduce the chance of hypoglycemia.
Insights into drug interactions and precautions
Understanding drug interactions and taking precautions is crucial when taking Meglitinides and Sulfonylureas for managing diabetes.
Here are some tips on the drug interactions and precautions that are required for both types of medications:
Sulfonylureas:
- Hypoglycemia Risk: Sulfonylureas may cause lower blood sugar levels (hypoglycemia). This risk increases when used together with other medications which lower blood sugar levels. Be aware of your blood sugar levels frequently Be aware of symptoms of hypoglycemia, such as shaking, sweating, or confusion.
- Alcohol: Alcohol can increase the hypoglycemic effects of Sulfonylureas. Take care to limit alcohol consumption If you drink, make sure that you eat before drinking to stabilize blood sugar levels.
- NSAIDs and certain medications: Some non-steroidal anti-inflammatory medications (NSAIDs) may alter blood sugar levels as well as the effects of Sulfonylureas. Certain drugs, such as beta-blockers, can cause hypoglycemia to be less noticeable. Be sure to consult your physician regarding how to use these drugs in conjunction with Sulfonylureas. They will be able to advise you on the appropriate dosages and monitor.
- Hepatic and Kidney Impairment: Sulfonylureas are processed and eliminated through the kidneys and the liver. A dysfunctional kidney or liver may affect how the body responds to these drugs. Be aware that dosage adjustments could be required in patients with impaired kidney or liver function. Check with your physician to determine the proper dosage.
Meglitinides:
- Hypoglycemia Risk: Meglitinides are also associated with the risk of hypoglycemia especially when used in conjunction with other medicines that reduce blood sugar. Precaution: Frequent blood sugar monitoring is essential. Consume Meglitinides prior to meals to ensure that they are synchronized with the food consumption.
- Time of meal: Meglitinides must be taken 15-30 mins prior to eating to boost insulin release. Inadequately reserving your meals or delaying them following the administration of the medication could cause lower blood sugar. Make sure you follow your meal plan in line with the time of your medication.
- CYP Enzyme Interactions: Certain medicines that are able to interact with CYP2C8 or CYP3A4 liver enzymes could affect the metabolism of Meglitinides. Take care to discuss all medicines with your physician to find out if they have any potential interactions and adjust dosages accordingly.
- Renal Impairment: Meglitinides, which are eliminated by the kidneys, impairment in renal function could affect their clearance. A dose adjustment may be necessary for those who have impaired kidney function.
- Liver Function: Liver impairment could affect the Meglitinide metabolism therefore, those with liver problems might require dosage adjustments. Take care to inform your doctor of any liver-related conditions or issues.
It’s essential to keep open and honest communication with your healthcare professional. They can aid you through the complex interactions of drugs and help you tailor the diabetes management program to your particular needs and situation.
Regular checking of blood glucose levels and adherence to the prescribed schedule of medication is essential to ensure that you are able to have safe and effective management.
Similarities Between Sulfonylureas and Meglitinides
Sulfonylureas and Meglitinides belong to two categories of oral antidiabetic drugs that are used to treat Type 2 Diabetes.
Although they have some distinctions they have many similarities:
- Mechanisms of action: The two Sulfonylureas and Meglitinides increase the production of insulin from beta cells of the pancreas. They work by binding to specific receptors found on beta cells, which results in an increase in insulin release. This mechanism of action assists in lowering blood sugar levels in people suffering from diabetes.
- Effects on Postprandial glucose: Both types of drugs have proven to be particularly effective in controlling the post-meal (postprandial) glucose spikes. Through promoting the release of insulin, they can help control blood sugar levels following meals.
- Quick Onset of Action: The two Sulfonylureas and Meglitinides have a quick start of action. This means they begin functioning shortly after taking them, which helps to regulate glucose levels after meals.
- Oral administration: Both sulfonylureas as well as Meglitinides are available as oral tablets which makes them ideal for patients who prefer oral medicines instead of injections.
- Multiple Agents Within Every Class: The two Sulfonylureas and Meglitinides contain a range of different medicines that are available in the respective class. This allows healthcare professionals to tailor their treatment to each patient’s requirements.
- Shorter Time of Action: In comparison to other medications that treat diabetes, such as metformin and metformin, the two Sulfonylureas and Meglitinides have a significantly shorter time to take effect. This allows for greater glycemic control in a short time frame without the danger of long-lasting effects.
- Hyperglycemia Risk: One of the most common side effects associated with each of Sulfonylureas as well as Meglitinides, is hypoglycemia or low blood sugar levels. Patients who take these medications must be aware of their levels of blood glucose and take steps to prevent hypoglycemia.
It’s crucial to keep in mind that, while there are similarities however, there are important differences between the two classes of drugs, which include their properties, duration of action, and the specific drugs in each category.
Healthcare professionals take into consideration these differences and similarities when deciding on the best treatment for a patient suffering from type 2 diabetes.
Conclusion
Sulfonylureas and Meglitinides are two types of oral antidiabetic medication frequently used to manage Type 2 Diabetes. They have similarity in their mechanisms of action, speedy time to action, and their effectiveness in limiting the post-meal blood glucose spikes. They differ in terms of the duration of effect, adverse reactions as well as individual effectiveness.
Healthcare professionals and patients should be aware of these aspects when selecting between these drugs making sure that the treatment plan is tailored to the specific requirements and preferences of each patient.
Effective management of diabetes involves more than just the choice of the appropriate medication, but also regular monitoring and adjustments to lifestyle to ensure the best blood glucose control.