Vasculitis is a class of immune-mediated disorders that cause inflammation in blood vessels. Of these, Giant Cell Arteritis and Takayasu Arteritis are distinct entities that possess distinctive characteristics, clinical profiles, and treatment strategies. This content outline will highlight the major distinctions between GCA and TA to aid in the diagnosis of their exact nature and the appropriate treatment.
What is Giant Cell Arteritis?
Giant Cell Arteritis (GCA) which is also referred to as temporal arteritis is an autoimmune chronic condition that predominantly is a problem for large and medium arterial arteries, with a particular focus on the temporal arteries along both sides of your head.
The condition causes an inflammation of the arterial wall, which may cause a variety of symptoms such as extreme headache as well as headache jaw claudication (pain when chewing), and visual disturbances.
GCA is more prevalent among those who are over 50 and is typically caused by elevated levels of inflammatory indicators in blood tests such as the erythrocyte-segregation rate (ESR) and C-reactive Protein (CRP).
If not treated, GCA can lead to severe complications, including stroke and blindness, making timely diagnosis and treatment essential. Treatment usually involves corticosteroid medication to ease inflammation and prevent complications.

What is Takayasu Arteritis?
Takayasu Arteritis (TA), often referred to as “pulseless disease,” is an uncommon chronic inflammatory disorder that primarily affects the large arterial arteries, including the aorta and its principal branches.
The autoimmune disorder causes swelling, thickening, and tightening of arteries affected and restricts the flow of blood to different tissues and organs. The most frequent signs of Takayasu Arteritis are abnormalities in the pulse and hypertension (high blood pressure) the symptom of claudication (pain and fatigue while doing physical activities) and possible neurological signs.
Takayasu Arteritis can be diagnosed by clinical examination imaging studies, such as angiography, as well as tests for blood to determine inflammation markers such as erythrocyte sedimentation rate (ESR). Because it is a risk to cause serious complications like stroke or organ damage prompt diagnosis and treatment is essential.
Treatment options for Takayasu Arteritis usually involve immunosuppressive medication to reduce inflammation, manage symptoms, and maintain blood vessel health. Due to its limited number of cases and diverse manifestations, the need for a multidisciplinary approach that involves cardiologists, rheumatologists, along other medical specialists is required for the full treatment of people suffering from Takayasu Arteritis.

Comparison Table of Giant Cell Arteritis and Takayasu Arteritis
Here’s a comparison table summarizing the key differences between Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA):
| Characteristic | Giant Cell Arteritis (GCA) | Takayasu Arteritis (TA) |
|---|---|---|
| Definition | Chronic autoimmune inflammatory disease primarily affects medium and large arteries, often the temporal arteries. | Rare chronic inflammatory disorder predominantly impacts large arteries, particularly the aorta and its branches. |
| Age of Onset | Typically occurs in individuals over 50 years old. | Can affect a wide age range, including younger individuals. |
| Gender Prevalence | Slightly more common in women. | Gender distribution varies by region but can affect both sexes equally. |
| Clinical Symptoms | Severe headache – Scalp tenderness – Jaw claudication – Visual disturbances – Constitutional symptoms (fatigue, weight loss, etc.) | Pulse abnormalities (e.g., absent or weak pulses) – Hypertension (high blood pressure) – Claudication (pain during physical activity) – Neurological symptoms – Constitutional symptoms (fever, fatigue, etc.) |
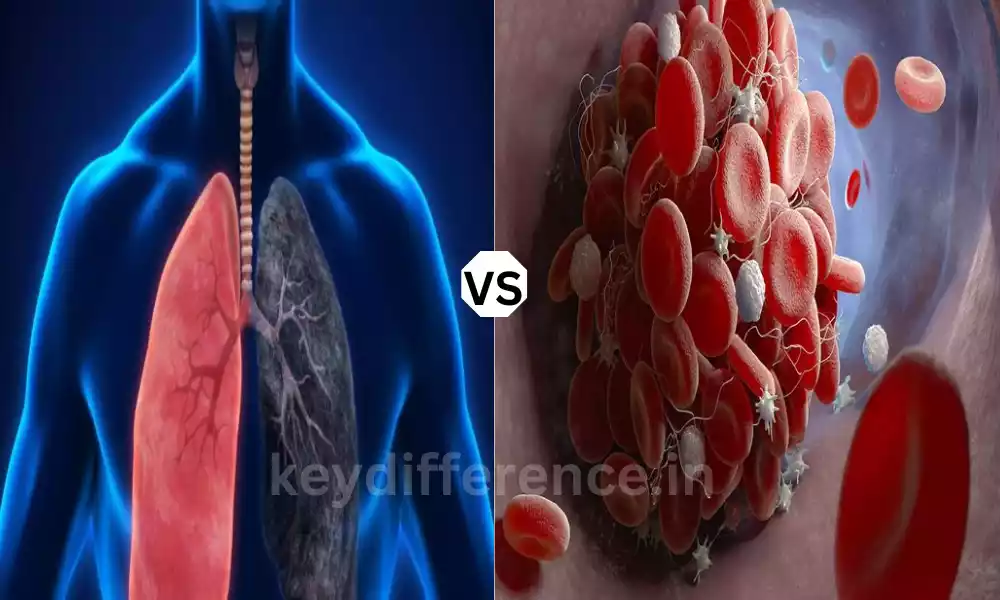
| Affected Arteries | Primarily medium and large arteries, especially temporal arteries. | Large arteries, notably the aorta and its branches. |
| Diagnostic Methods | Clinical evaluation – Laboratory tests (e.g., ESR, CRP) – Imaging (e.g., temporal artery ultrasound) | Clinical evaluation – Imaging (e.g., angiography) – Laboratory tests (e.g., ESR, CRP) |
| Treatment Approach | Predominantly managed with corticosteroid medications to reduce inflammation. | Typically requires immunosuppressive therapy to control inflammation and preserve vascular health. |
| Potential Complications | Blindness due to involvement of ophthalmic arteries – Stroke – Aortic aneurysms – Arterial stenosis – Scalp necrosis – Other organ damage | Organ damage due to reduced blood flow – Hypertensive complications – Stroke – Cardiac involvement – Vascular stenosis or aneurysms |
This table highlights some of the key differences between Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA), including their demographics, clinical presentations, affected arteries, diagnostic methods, and treatment approaches.
It’s important to note that both conditions are serious and require specialized medical care for proper diagnosis and management.
Importance of distinguishing between Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA)
The distinction between Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA) is essential in the medical field and patient care, due to a variety of important reasons:
- Tailored Treatment Methodologies: GCA as well as TA are treated differently. GCA is usually treated with corticosteroid drugs, while TA usually requires immunosuppressive therapy. The wrong treatment could result in inadequate control of the disease unneeded side effects and even worse outcomes. An accurate diagnosis can ensure your patients get the most effective and appropriate treatments.
- Preventing Complications: GCA and TA could cause serious complications, such as blindness, cerebral stenosis, stroke, or organ damage. Knowing the particular condition helps health professionals to track and treat these issues proactively. For instance, when it comes to GCA treatment, timely corticosteroid therapy could help to prevent loss of vision.
- Different Patient Demographics: GCA primarily affects older people, specifically people over 50 however TA may affect a wider range of age groups which includes children and younger children. Knowing the characteristics of these diseases aids healthcare medical professionals in their diagnostic criteria and clinical evaluations.
- Risk assessment Multiple: Vascular regions are implicated with GCA in addition to TA. GCA predominantly affects arteries with medium-sized diameters which include the temporal arteries. Meanwhile, TA is primarily focused on bigger arteries such as the aorta as well as its branches. Knowing the arteries that are most at risk aids clinicians in assessing the risk for complications and adapting their treatment and diagnostic strategies to suit.
- Prognostic ImplicationsThe prognosis and the long-term outcomes may differ among GCA as well as TA. The TA can cause greater complications and vascular damage which makes an early diagnosis and aggressive treatment crucial. However, GCA, when promptly treated, usually has an improved prognosis. The distinction between the two conditions can help predict the progression of the disease as well as guide the patient’s expectations.
- Resource Allocation: The distinction between GCA and TA could help in the efficient allocation of healthcare assets. For instance, TA patients may require more specific interventions and constant surveillance due to how they are affected by their involvement with the arterial. A precise diagnosis allows healthcare providers to provide the appropriate treatment and support for the specific medical condition.
- research as well as Clinical Trials: Conducting research and clinical trials to discover new treatments and to understand the fundamental mechanisms that cause these conditions is dependent on specific diagnostic criteria as well as accurate classification of patients. Differentiating from GCA and TA assures that the populations of study are uniform, resulting in greater research results.
In the end, knowing the difference between Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA) is crucial to providing optimal care to patients, preventing complications, customizing treatments, and aiding research efforts.
It emphasizes the importance of a precise diagnosis as well as the importance of a multidisciplinary approach that involves cardiologists, rheumatologists, as well as other experts to guarantee the most optimal outcomes for patients suffering from these conditions.
Predominantly affects medium and large arteries
I notice you’ve highlighted “predominantly affects medium and large arteries.” This is a valid statement for the two conditions Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA), because both diseases primarily cause the inflammation of arterial vessels in large and medium arteries. To clarify:
- Giant Cell Arteritis (GCA): GCA generally affects large and medium arteries, with a preference for those arteries that are temporal (medium-sized arteries) along the side that runs through the skull. However, it could also affect other large blood vessels in the body, like the aorta as well as its branches.
- Takayasu Arteritis (TA): TA typically affects large arteries particularly the aorta as well as the major branches of it, that are regarded as large arteries. Although TA is primarily a problem for large arteries, it may also affect arteries of medium size in some instances.
It is important to remember that both of these conditions can cause severe vascular inflammation, possibly leading to complications due to a decrease in blood flow or damaged arterial.
A precise diagnosis and proper management is essential to reduce these risks and offer the most effective care possible for patients suffering from GCA as well as TA.
What are the Similarities Between Giant Cell Arteritis and Takayasu Arteritis
Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA) are two different types of vasculitis and although they are distinct traits, they have a few similarities:
- Autoimmune Nature: The two GCA along with TA are autoimmune conditions which means they trigger an unnatural immune system response in which the immune cells of the body attack its blood vessels within. The autoimmune system that is shared between the two is responsible for the inflammation in the system that is seen in both.
- Vascular Inflammation: For both GCA and TA there is inflammation of blood vessels. While the arteries that are affected are different, the root vasculitis process (inflammation of blood vessels) is a common occurrence.
- Higher Inflammatory Markers: Lab tests for inflammation, including the erythrocyte sedimentation rate (ESR) and C-reactive proteins (CRP) generally elevated in both of the conditions. These markers can help diagnose and track disease activity.
- Systemic symptoms: Both GCA and TA are able to be accompanied by constitutional or systemic symptoms that include an increase in fever, fatigue, or weight loss. These symptoms indicate the nature of inflammation in the system which is a hallmark of these ailments.
- Higher Risk of Complications: If untreated or poorly controlled Both GCA and TA may cause serious complications, such as organ damage, stroke, and aneurysms, or vascular stenosis.
- Multidisciplinary Treatment: The management of both GCA and TA usually necessitates a multidisciplinary treatment, involving different medical specialists including rheumatologists cardiologists, ophthalmologists, and vascular surgeons. This multidisciplinary approach provides comprehensive medical care for patients.
- Immunosuppressive Treatment: Although the exact medications and treatment strategies might vary, the two conditions generally require the use of immunosuppressive medications to reduce inflammation and slow the progression of disease.
- The importance of early diagnosis: Early diagnosis is vital for both GCA as well as TA to start treatment in a timely manner and decrease the chance of complications. A delayed diagnosis could lead to grave consequences for both conditions.
- Vascular Imaging: Techniques for imaging, like angiography, can be utilized to determine the presence of vascular vessels and assess disease activity both in GCA and TA.
Despite these similarities, it is crucial to understand it is important to recognize that GCA and TA remain distinct illnesses with different the demographics and affected arterial arteries as well as clinical signs and treatment strategies. A precise distinction is essential in order to ensure appropriate treatment for those affected.
Reference Books
Certainly, here are some reference books that cover vasculitis, including Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA), as well as related topics in rheumatology and autoimmune diseases.
These books can be valuable resources for healthcare professionals, researchers, and individuals looking to learn more about these conditions:
- “Vasculitis: Diagnosis and Management” by Richard A. Watts and David G. I. Scott
- This comprehensive book provides an in-depth overview of vasculitis, including various types, clinical features, diagnosis, and management strategies.
- “Vasculitis in Clinical Practice” by Robert J. Moots and David L. Scott
- A practical guide covering the clinical aspects of vasculitis, including diagnostic challenges and treatment options.
- “Takayasu Arteritis” by John H. Stone
- This book focuses specifically on Takayasu Arteritis, offering insights into the epidemiology, clinical manifestations, and management of this rare condition.
- “Giant Cell Arteritis: A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References” by Icon Health Publications
- A resource that includes an extensive bibliography of research articles and materials related to Giant Cell Arteritis.
- “Rheumatology Secrets” by Sterling West and Jason Kolfenbach
- This book covers various rheumatological conditions, including vasculitis, in a question-and-answer format, making it a useful resource for quick reference and review.
Conclusion
Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA) are distinct vasculitis-related autoimmune conditions that typically affect large to medium-sized arteries, causing the development of inflammation and potentially causing complications.
Although they have some commonalities in terms of autoimmune causes and inflammation throughout the body, however, they differ with respect to the time of onset and gender, the prevalence of affected arteries, clinical signs, and treatment methods.
A precise diagnosis and a customized treatment are essential for enhancing patient outcomes and preventing major complications from these diseases.