The brachial nerve is an intricate network of nerves that runs through the arm and shoulder region which are responsible for motor as well as sensory functions. Brachial plexus injuries can be classified broadly into postganglionic and preganglionic injuries that have distinct features and treatment methods.
The key distinctions between these Preganglionic and Postganglionic Brachial Plexus Injury of injuries, provide a clearer understanding of their anatomy the causes symptoms, diagnosis treatment, and management in the hope of providing knowledge of this complex medical condition.
What is Preganglionic Brachial Plexus Injury?
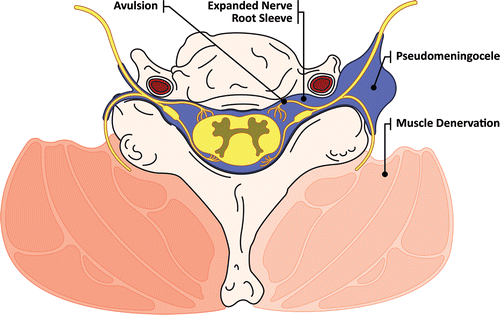
Preganglionic brachial plexus injuries are a result of damage or disruption that occurs close to (before) the development of the sympathetic nerve in the brachial area. In simple terms, this condition affects the nerves prior to reaching the Ganglia, which are the clusters of nerve cells.
Preganglionic traumas typically involve the nerve trunks in the brachial complex, which usually result from trauma or extreme stretching. These injuries may cause significant sensory and motor impairments within the affected arm.
What is Postganglionic Brachial Plexus Injury?
Postganglionic brachial plexus injuries are a result of the destruction or disruption that happens in the distal region (after) the development of sympathetic ganglia inside the plexus brachial. In simple terms, the injury affects nerves after they’ve passed the ganglia, which are the clusters of nerve cells.
Postganglionic injuries usually affect the nerves and nerve branches that have come out of the ganglia. They may result from a variety of causes such as trauma, compression, or entrapment. These can cause sensory and motor impairments in the affected arm.
Importance of understanding brachial plexus injuries
Knowing how to treat brachial plexus injuries vital for many reasons:
- Medical Diagnostics and Treatment: A precise diagnosis of brachial-plexus injuries is vital to provide adequate medical treatment. Understanding the severity of injuries helps medical professionals identify the severity and nature of the injury, permitting them to develop individualized treatment strategies.
- Rehabilitation of Patients: Understanding the brachial plexus injury is essential for physical therapists as well as rehabilitation specialists. They can design rehabilitation programs that target particular weaknesses and assist patients in regaining their motor and sensory functions efficiently.
- Surgical intervention: Surgeons require a knowledge of the brachial plexus injury to make surgical repairs if needed. Different injuries require specific procedures, and the right information will ensure the most effective results for patients.
- Information for Patients: Families and patients benefit from knowing the causes of their injuries. This allows them to make informed decisions regarding their treatment, establish realistic expectations for their recovery, and participate actively in their recovery process.
- Prevention and Risk Assessment: Understanding the causes and aspects of injuries to the brachial plexus can assist individuals and companies in adopting preventive steps. This is especially relevant for occupations that have the risk of injuries, such as sports or manual workers.
- legal and insurance Issues: Professionals from the legal and insurance fields dealing with personal injury as well as workers’ comp claims should be aware of the causes and impact of brachial-plexus injuries in order to guarantee the most equitable and fair outcomes for those affected.
- Studies and Advancements: Understanding injuries to the brachial plexus is vital for ongoing study in the fields of neurology as well as orthopedics. The advancements in the understanding of these injuries could help in the development of more effective diagnosis tools, treatment techniques as well as potential treatments.
- Public Health: Understanding brachial plexus injuries could contribute towards public health awareness and programs that help people recognize the symptoms of injuries like these and seek medical attention if needed.
- Qualities of life: Understanding brachial plexus injuries could significantly affect the quality of life of the people affected. The right treatment and rehabilitation methods can enhance the functional outcome and limit the long-term effects of impairments.
Understanding the severity of brachial plexus injuries is vital for medical personnel, patients, and the general public. It is not just helpful in obtaining an accurate diagnosis and treatment but also helps in preventing research and improvement in outcomes for those suffering from these difficult injuries.
Comparison Table of Preganglionic and Postganglionic Brachial Plexus Injury
Here’s a comparison table highlighting the key differences between preganglionic and postganglionic brachial plexus injuries:
| Characteristic | Preganglionic Brachial Plexus Injury | Postganglionic Brachial Plexus Injury |
|---|---|---|
| Location of Injury | Occurs proximal to the sympathetic ganglia within the brachial plexus. | Occurs distal to the sympathetic ganglia within the brachial plexus. |
| Nerve Damage | Affects nerves before reaching the ganglia, primarily involving upper roots or nerve trunks. | Affects nerves after passing through the ganglia, often involving nerve branches. |
| Causes | Typically results from severe stretching, trauma, or compression injuries. | Commonly caused by direct trauma, entrapment, or compression at the peripheral nerve level. |
| Motor Function | Severely impairs motor function in the affected arm, often resulting in paralysis. | This may lead to varying degrees of motor deficits, ranging from weakness to paralysis. |
| Sensory Function | Significant sensory deficits in the affected arm, including numbness and loss of sensation. | Sensory deficits such as numbness or altered sensation may also occur but can be less severe. |
| Prognosis | Generally associated with a poorer prognosis due to the complexity of regenerating nerves before ganglia. | Tends to have a relatively better prognosis because nerves can regenerate more effectively after ganglia. |
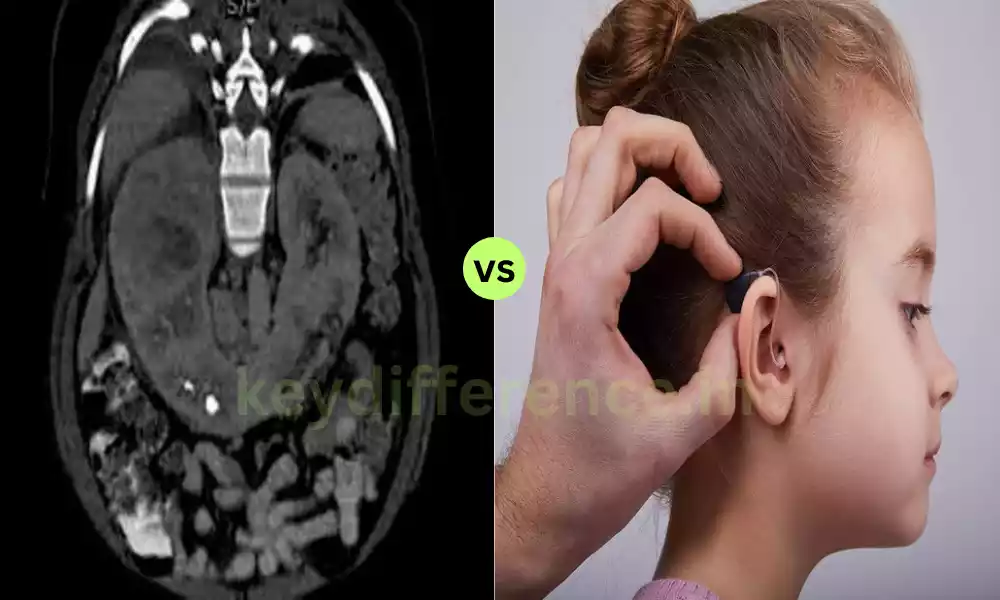
| Diagnosis | Diagnosed based on clinical examination, imaging (e.g., MRI), and electromyography (EMG) studies. | Diagnosed through clinical assessment, imaging, and EMG, similar to preganglionic injuries. |
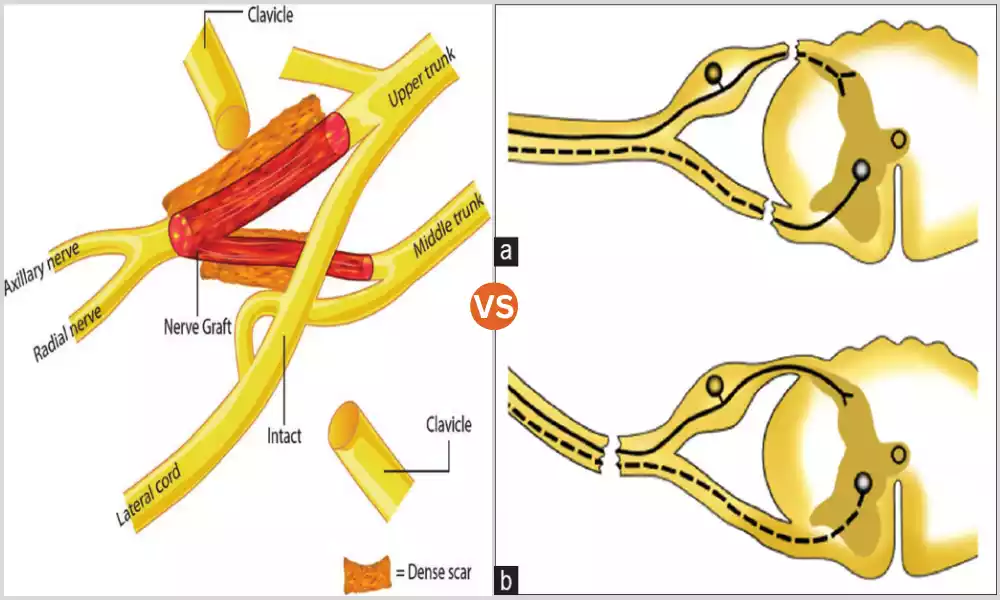
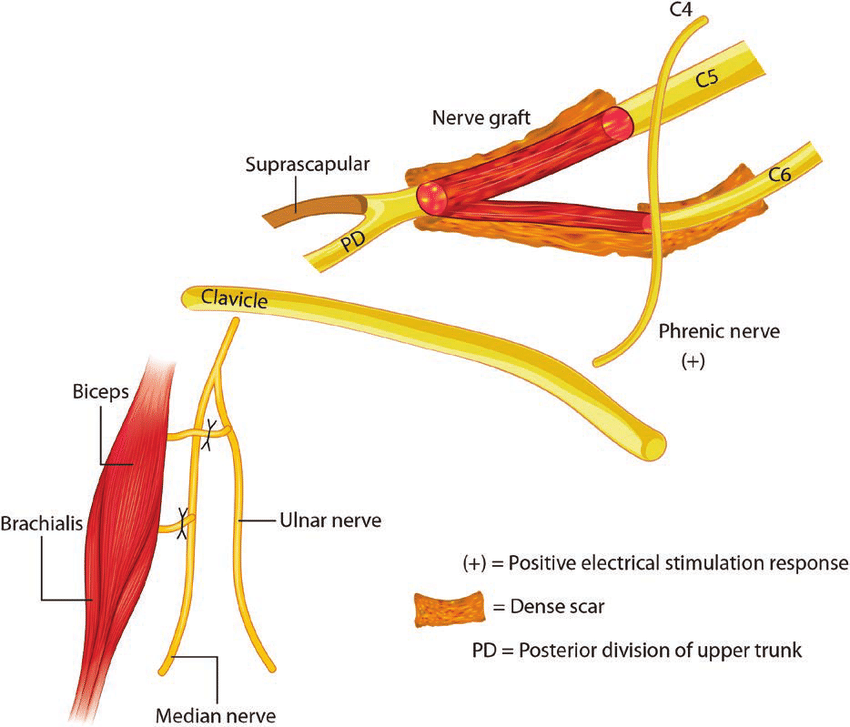
| Treatment | Treatment options may include surgical nerve grafting or nerve transfers, often with guarded outcomes. | Treatment may involve surgical repair, but outcomes are generally more favorable with a higher likelihood of nerve regeneration. |
| Rehabilitation | Rehabilitation is challenging due to the limited regenerative capacity of pre-ganglionic nerves. | Rehabilitation is typically more successful as post-ganglionic nerves have better regenerative potential. |
| Long-Term Outcomes | Often associated with more persistent and severe disabilities, with limited functional recovery. | Tends to offer better long-term outcomes, with a higher potential for functional improvement. |
Note: It’s essential to consult with a healthcare professional for a comprehensive evaluation and personalized treatment plan in cases of brachial plexus injuries, as individual circumstances can vary widely.
Clinical presentation and symptoms
The symptoms and clinical manifestations of postganglionic or preganglionic brachial plexus injuries may differ and understanding the difference is crucial for precise diagnostics and treatments.
Here are the most common symptoms and clinical signs that are associated with the various types of injuries:
Preganglionic Brachial Plexus Injury:
- Flaccid paralysis: Patients often present with a limp and flaccid shoulder on their affected side because of the impairment in motor functions. It can cause impossibility to move the arm, shoulder, or hand in a voluntary manner.
- Sensory Loss: The preganglionic injury can cause significant sensory deficiencies, which include the sensation of tingling and numbness as well as a reduction in sensation within the arm affected.
- Muscle Atrophy: In time muscle atrophy (wasting) can be observed in the arm affected because of the lack of motor nerves.
- Horner’s syndrome: In some instances, there could be a connection with Horner’s syndrome. It is characterized by the condition known as ptosis (drooping on the eyelids of upper limbs) as well as miosis (constricted pupil) and anhidrosis (lack or lack of sweating) on the affected face.
- Anomalies of Reflex: Deep tendon reflexes in the affected arm could be absent or diminished.
- The pain and Neuropathic symptoms: Some patients may suffer from neuropathic pain, burning sensations, or other abnormal sensations (paresthesias) within the arm affected.
Postganglionic Brachial Plexus Injury:
- Insufficiency: Patients typically exhibit weakness in the affected arm, rather than flaccid paralysis. The degree of weakness may range from mild to severe.
- Sensory Changes: Sensory impairments like numbness discomfort, or altered sensation are possible, but they are usually less noticeable than preganglionic injury-related injuries.
- Muscle Atrophy: Muscle atrophy could happen over time, but it is usually less severe than preganglionic injuries because of the greater regenerative capacity of postganglionic nerves.
- Horner’s syndrome (Rare): Horner’s syndrome is not as often linked to postganglionic injuries as when compared with preganglionic injuries.
- Reflexes: The deep tendon reflexes could be reduced or absent in the affected arm.
- Flexible Recovery: In general, postganglionic injuries are more likely to be successful and have the possibility of a certain degree of functional healing, subject to the degree of injury and the efficacy of rehabilitation and treatment.
It’s crucial to remember that the exact characteristics and severity of brachial-plexus injuries will vary from one case to the next. Furthermore, a thorough evaluation of the patient, which includes examinations as well as imaging studies as well as electromyography (EMG) is vital to accurately determining the nature and severity of the injury as well as determining the suitable treatment strategy.
Causes of postganglionic injuries
Brachial plexus injuries that are postganglionic can be caused by a variety of causes that can be caused by either direct trauma or compression at the level of the peripheral nerve.
Common causes of postganglionic brachial injuries are:
- Motor Vehicle Accidents High-impact collisions between motor vehicles such as collisions with motorcycles or cars could result in postganglionic brachial nerve injuries. Acceleration speeds that are too fast or force of impact can result in nerve damage.
- Falls: falls from high places or slips and falls could cause bruises to your brachial nerve, particularly when people fall on their arms that are stretched out.
- Sports-related injuries: Contact sports like rugby or football and activities that are high-impact like gymnastics may cause postganglionic injuries when there is an injury or dislocation to the joint of the shoulder.
- Penetrating and Stab Injuries: Sharp objects, like knives or glass shards, can cause injuries penetrating into the postganglionic nerves.
- Gunshot Wounds: Gunshot wounds may cause significant injuries to the brachial plexus which can result in postganglionic injuries.
- The growth of tumors or compression: Growths that are abnormal or tumors within the vicinity of the brachial plexus may cause nerve damage and compression and cause signs and symptoms.
- Iatrogenic causes: A few surgical operations like dissection of lymph nodes, and shoulder surgery, can cause postganglionic nerve damage.
- Repetitive overuse or microtrauma: The long-term overuse or repeated microtrauma (e.g. in the case of manual laborers or athletes) could result in nerve irritation or compression which can result in postganglionic injury in the course of time.
- Neurological Disorders: Certain neurological conditions or diseases, like neuro tumors (neuromas) or auto-immune disorders that affect peripheral nerves, can result in damage to the postganglionic nerve.
- Brachial plexitis (Parsonage-Turner Syndrome): This is an inflammation that can be a problem for the brachial nerve and cause postganglionic damage. The precise nature of the brachial plexus is not always obvious.
It’s crucial to know that postganglionic brachial-plexus injuries may vary in severity according to the reason for the injury and the severity of the extent of damage. A prompt medical examination and the right tests for diagnosis are essential to diagnosing the cause and developing the most effective rehabilitation and treatment strategies for those suffering from these injuries.
Nerve damage and regeneration potential
Regeneration and nerve damage differ in postganglionic and preganglionic brachial plexus injury due to their different location and the mechanisms they employ.
This article will explain how the damage to nerves and their regeneration possibilities differ between the two kinds of injuries:
Preganglionic Brachial Plexus Injury:
- Nerve damage: The majority of preganglionic injuries cause damage to nerve roots or trunks proximal sympathetic Ganglia. The nerves are typically damaged and avulsed (completely separated from the spine) or compressed. This kind of injury can result in more severe damage to the nervous system.
- The possibility of regeneration: The regeneration of nerve fibers following preganglionic injury is a challenge. Nerves need to regenerate from the site of injury to the spinal cord this is a difficult and long-lasting procedure. Regeneration is complicated due to the necessity of nerve transplants or transfer surgeries to connect the nerve that has been injured and the spinal cord.
- Functional Recovery: Recovery from functional preganglionic injuries is usually restricted, and the degree of recovery depends largely on the effectiveness of surgical treatments. Even after surgical repairs, some patients suffer from permanent motor and loss of sensory.
Postganglionic Brachial Plexus Injury:
- Nerve damage: Postganglionic injuries involve injuries to nerves and branches that are distal to the sympathetic ganglia. The resulting injuries can cause several degrees of nerve disconnection such as compression, stretching, or even partial tear.
- Possibility of Regeneration: The postganglionic nerves possess an essentially higher potential for regeneration as compared to preganglionic nervous nerves. They are this because they are more close to the tissue and muscles of the arm, as well as the neurons (neurons) that are responsible for regeneration are still in place.
- Functional Recoveries: In the majority of cases, postganglionic traumas provide a better chance in terms of functional healing. With the proper medical treatment as well as surgical repair and rehabilitation, a lot of people suffering from postganglionic injuries are able to regain different levels of sensory and motor function. The degree of recovery is contingent on various factors like the extent of the injury as well as the efficacy of the treatment.
The primary distinction in the damage to nerves and potential for regeneration between postganglionic and preganglionic brachial-plexus injuries is the site of the injury and its closeness to sympathetic ganglia as well as the spinal cord.
Preganglionic injuries usually result in more severe nerve damage, and pose greater difficulties for rehabilitation and recovery, while postganglionic injuries have a higher chance of improvement in function when treated appropriately.
Rehabilitation strategies for both types of injuries
Rehabilitation plays an important aspect in the rehabilitation of people suffering from brachial-plexus injuries regardless of whether the injury was postganglionic or preganglionic. However, the exact rehabilitation methods may differ based on the severity and type that the injuries.
Here are some typical methods of rehabilitation for both types of brachial plexus injuries:
Rehabilitation for Preganglionic Brachial Plexus Injury:
- Initial Assessment, and Plan: Begin rehabilitation as when the patient’s physical condition permits. An extensive assessment by a specialist in rehabilitation is crucial to assess the severity of the deficit and set achievable goals.
- Passive Range of Motion (ROM) Exercises: Initially, focus on light passive ROM exercises to reduce joints from contractures and stiffness in the limb affected. These exercises can require the assistance of a physical therapist or specialized equipment.
- Splinting: Based on the degree of paralysis or muscle weakness custom-designed splints could be employed to stabilize the arm affected and ensure the alignment of joints.
- Electrical Stimulation: The stimulation of the electrical nerve, including FES, or functional electrical stimulation (FES) can assist in retaining muscle strength and help prevent muscle atrophy in muscles that are paralyzed.
- Strengthening and Stretching: As recovery progresses Active and resistance-based exercises focused on the muscles remaining in the affected limb could aid in improving flexibility and strength.
- Neuromuscular Rehabilitation: The therapist can employ methods to assist the patient in gaining control over certain muscle groups while focusing on the tasks essential to daily life.
- Functional Training: Rehabilitation must include tasks that replicate real-life scenarios to increase the ability of the patient to carry out everyday tasks and gain independence.
- The Art of Pain Management: Treat neuropathic discomfort or pain by using a variety of methods such as the use of medication, nerve blockers, or other techniques for managing pain.
Rehabilitation for Postganglionic Brachial Plexus Injury:
- Evaluation and Preparation for Early Stages: Like preganglionic injury, start the rehabilitation process as early as possible after injury. An in-depth assessment can help determine the particular limitations and goals for functional rehabilitation.
- RMO Exercises: Begin by doing ROM exercises that are passive to keep joint mobility intact and prevent contractures. Gradually increase the intensity of ROM exercises based on the level of discomfort.
- Strengthening Exercises: Create a custom-designed strengthening program that targets the muscles that are affected and muscles. Training with resistance can improve the performance of your muscles.
- Sensory Re-education: Resolve sensory deficiencies by using techniques to help the patient to regain consciousness and the ability to discriminate sensory inputs within the affected part of the limb.
- Functional Activities: The focus should be on tasks that are similar to daily activities in order to help promote independence. The occupational therapist plays an essential role in this area of rehabilitation.
- The Management of Pain: Control discomfort and pain effectively so that the patient is able to participate in exercises for rehabilitation comfortably.
- Orthotic devices: Orthotic devices or assistive technology could be recommended to aid in specific tasks.
- Educational for Patients: Instruct the patient about their health condition and the importance of ensuring compliance through exercises, and strategies to manage everyday activities.
- Psychosocial Assistance: Address the emotional and psychological aspects of recovering since brachial plexus injury can be emotionally difficult.
Rehabilitation for both kinds of brachial plexus injuries is typically a procedure that calls for a multidisciplinary approach, involving occupational therapists, physical therapists, and others.
The rehabilitation program should be customized to each individual’s needs and continuously altered based on improvement. Furthermore, early intervention as well as ongoing support is essential to ensure the best results in functional terms.
Long-term outcomes and quality of life considerations
Quality of life concerns for people suffering from injuries to the brachial plexus, whether postganglionic or preganglionic, will vary based on many factors, such as the extent of the injuries, as well as the efficacy of treatment and the person’s reaction to rehabilitation.
Here are some of the most important factors to take into consideration regarding the long-term effects and the quality of life:
Long-Term Outcomes:
- Injuries of a high severity: The extent of the damage to nerves and functional impairments significantly affects the long-term outcome. Preganglionic injuries are typically associated with more serious and long-lasting impairments compared to postganglionic.
- Potential for Recovery: Postganglionic injuries tend to provide a better chance for functional recovery because of the greater regenerative capacity of the postganglionic nerves. However, preganglionic injury typically has a limited chance of full recovery.
- Surgery: The success of surgical procedures, including nerve grafting or transfers is able to significantly affect the long-term outcome. The successful repair of nerves can result in improved functionality and overall quality of life.
- Rehabilitation: Your commitment and efficacy of rehabilitation play an important role in the long-term results. Regular specific rehabilitation can assist people in regaining their motor abilities and overcoming any remaining deficiencies.
- Psychology Impact: Injuries to the brachial plexus could have a major psychological impact on a person. The process of dealing with permanent disabilities and adapting to a new style of life may be challenging.
- Pain Management: Persistent neuropathic pain is a common occurrence in the brachial area after injuries. Effective strategies for managing pain are crucial to improving your quality of life.
Quality of Life Considerations:
- Independence: Inspiring people to be independent in everyday activities is the primary objective for people suffering from injured brachial muscles. In addition, adaptive methods and assistive devices might be needed to accomplish this.
- Vocational and occupational considerations: The ability to return to work or develop the career you want to pursue could be affected by an injury. Rehabilitation and modifications to work may play a part in improving the quality of life.
- Sports and Social Activities: Maintaining connections with friends and engaging in recreational activities can improve the quality. Sports and leisure activities that can be adapted can be explored.
- Pain Management: Effective pain management is essential for improving general well-being and living quality. Multimodal approaches to managing pain could be required.
- Psychology Support: The accessibility to psychotherapy support or counseling groups can aid individuals with the emotional difficulties that arise from brachial plexus injuries.
- Adaptive Technology: The use of assistive devices and technology can increase the independence of people and allow them to participate in different aspects of everyday life.
- family and support from social networks: The assistance of friends and family members can have a significant impact on how well those suffering from brachial plexus injuries. Support and education for caregivers are also essential.
- Patient Advocates: Advocacy organizations and networks are a great source of sources, information, and opportunities for those suffering from injuries to the brachial plexus.
It is important to stress that even though brachial plexus injuries may cause major challenges, a lot of people have a fulfilling life and enjoy an excellent quality of life by combining medical treatment, rehabilitation assistance, and adapting to their surroundings.
The long-term results and quality of life will continue to improve as people adjust and develop their capabilities and strengths.
Similarities Between Preganglionic and Postganglionic Brachial Plexus Injury
Although postganglionic and preganglionic brachial plexus injury have distinct characteristics, they share some commonalities between them:
- Anatomical Localization: Both types of injuries affect the brachial plexus which is a system composed of nerves located within the neck and shoulder region that are responsible for sensory and motor functions in the upper lower limb. In both instances, the injuries are triggered by this intricate nerve system.
- Symptoms of motor and Sensory Deficits: Preganglionic and postganglionic injuries can cause motor impairments, like paralysis or weakness of muscles, and sensory impairments, such as the sensation of numbness, tingling, or loss of sensation in the arm affected.
- Evaluation of Clinical Needs: The initial clinical evaluation and diagnostic procedure for both kinds of injuries usually involve physical examination scans (e.g., MRI or CT scans) and electromyography (EMG) to assess nerve function and determine the extent and location of the damage.
- Treatment Modalities: Treatment strategies for both kinds of injuries could include surgical procedures as well as physical therapy, occupational therapy, as well as methods for managing pain. In both cases, the goal is to improve the quality of recovery and functional life.
- Rehabilitation: Rehab is a vital component of the recovery procedure for preganglionic as well as postganglionic injuries. Rehabilitation is focused on enhancing motor function, sustaining joint mobility, reducing pain, and improving general health.
- Long-Term Challenges: People suffering from both types of injuries could be confronted with long-term issues related to their condition, which could include injuries, physical restrictions, and possible emotional and psychological consequences. The long-term outlook as well as aspects of quality of life are crucial aspects to consider in both instances.
- Multidisciplinary care: In both types of injuries to the brachial plexus A multidisciplinary approach to medical care that includes health professionals from various disciplines, such as neurology, physical therapy, orthopedics, psychology, and occupational therapy is typically required for providing complete treatment and support.
Although these are all commonalities it’s important to understand that there are distinct differences between preganglionic as well as postganglionic injuries, especially with regard to the prognosis, potential for regeneration of nerves as well as the degree of damage to the nerve.
An accurate diagnosis and custom-made treatment plans are essential to deal with the unique challenges and specific characteristics that come with each kind of injury.
Reference Books
Certainly! Here are some reference books on various topics and genres. If you have a specific subject or area of interest in mind, please let me know, and I can provide more targeted recommendations.
- Medicine and Healthcare:
- “Harrison’s Principles of Internal Medicine” by Dennis L. Kasper, et al.
- “Gray’s Anatomy for Students” by Richard Drake, et al.
- “Robbins and Cotran Pathologic Basis of Disease” by Vinay Kumar, et al.
- Psychology and Mental Health:
- “Psychology” by David G. Myers and C. Nathan DeWall.
- “The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma” by Bessel van der Kolk.
- “Thinking, Fast and Slow” by Daniel Kahneman.
- Science and Popular Science:
- “A Brief History of Time” by Stephen Hawking.
- “Sapiens: A Brief History of Humankind” by Yuval Noah Harari.
- “The Immortal Life of Henrietta Lacks” by Rebecca Skloot.
- History:
- “A People’s History of the United States” by Howard Zinn.
- “The Guns of August” by Barbara W. Tuchman.
- “SPQR: A History of Ancient Rome” by Mary Beard.
- Fiction and Literature:
- “To Kill a Mockingbird” by Harper Lee.
- “1984” by George Orwell.
- “Pride and Prejudice” by Jane Austen.
- Self-Help and Personal Development:
- “The 7 Habits of Highly Effective People” by Stephen R. Covey.
- “Daring Greatly: How the Courage to Be Vulnerable Transforms the Way We Live, Love, Parent, and Lead” by Brené Brown.
- “Atomic Habits: An Easy & Proven Way to Build Good Habits & Break Bad Ones” by James Clear.
- Business and Economics:
- “The Lean Startup: How Today’s Entrepreneurs Use Continuous Innovation to Create Radically Successful Businesses” by Eric Ries.
- “Thinking, Fast and Slow” by Daniel Kahneman (also relevant to economics).
- Technology and Computer Science:
- “The Pragmatic Programmer: Your Journey to Mastery” by Andrew Hunt and David Thomas.
- “Clean Code: A Handbook of Agile Software Craftsmanship” by Robert C. Martin.
- Philosophy:
- “Meditations” by Marcus Aurelius.
- “Sophie’s World” by Jostein Gaarder (an introduction to philosophy through fiction).
- Cookbooks and Food:
- “The Joy of Cooking” by Irma S. Rombauer.
- “Mastering the Art of French Cooking” by Julia Child.
Conclusion
Reference books are invaluable sources that provide comprehensive information about a variety of topics, ranging from literature to medicine, science to self-help. They serve as guidebooks for exploration, learning, and personal development providing insights and advice by experts in their areas of expertise.
It doesn’t matter if you want to deepen your knowledge of a specific subject or simply relish enjoying the process of studying the books of reference, they are indispensable guides on your journey to knowledge.