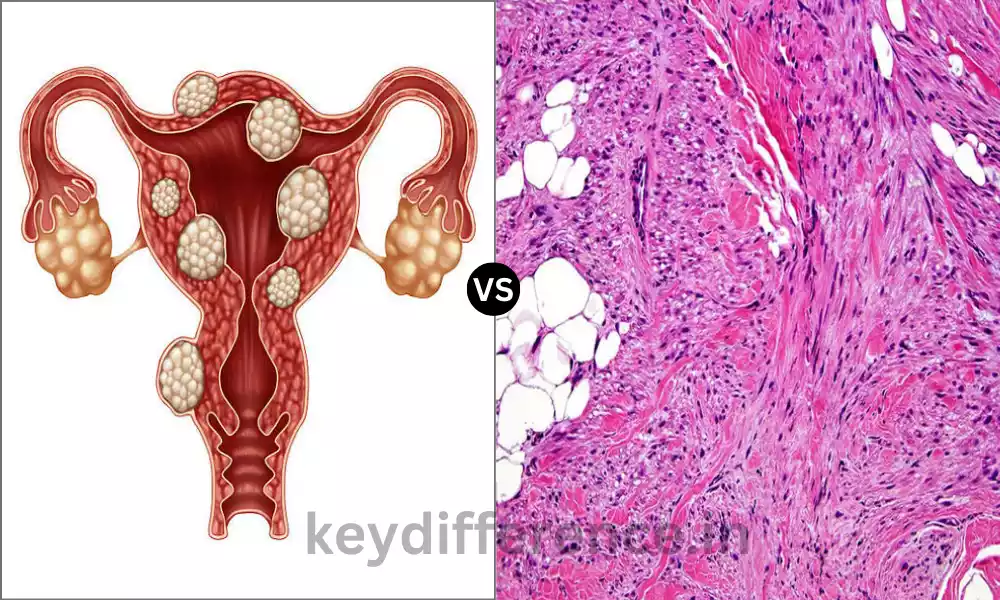
Leiomyoma and Leiomyosarcoma are both cancerous tumors that originate from smooth muscle cells however they differ greatly in their character and impact on health. Although leiomyomas, also known as fibroids are benign growths commonly found in organs such as the uterus and uterus, leiomyosarcomas are malignant tumors that can be extremely dangerous to health.
The distinction between the two is essential since their treatment, prognosis, and effects differ greatly. This guide focuses on the main distinctions between them providing information for doctors and patients.
What is Leiomyoma?
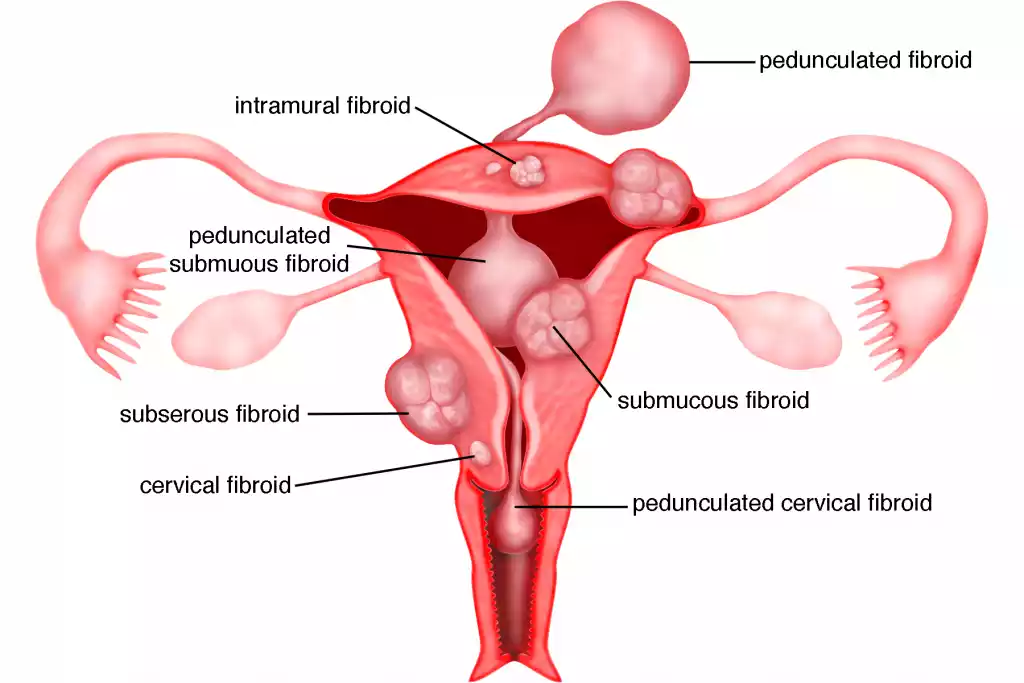
Leiomyoma often called fibroid is a benign tumor of the smooth muscle that originates primarily from the myometrium, or the tunica muscle layer of other viscera. The tumors consist of smooth muscle cells as well as fibrous connective tissue.
The most frequently encountered location for leiomyomas can be found in the uterus. They are usually referred to as “uterine fibroids”. However, they are present in other parts of the body, where there are smooth muscles including the digestive tract and the skin.
Leiomyomas develop due to hormones such as estrogen and tend to shrink or become stable after menopausal change. They are of various sizes and range from tiny nodules to huge masses that spread out the organ within which they’re located.
What is Leiomyosarcoma?
Leiomyosarcoma can be described as a rare and aggressive malignant tumor that originates from smooth muscles. As opposed to leiomyomas, leiomyosarcomas possess the potential to invade the surrounding tissues and then spread to different parts of the human body and could be life-threatening.
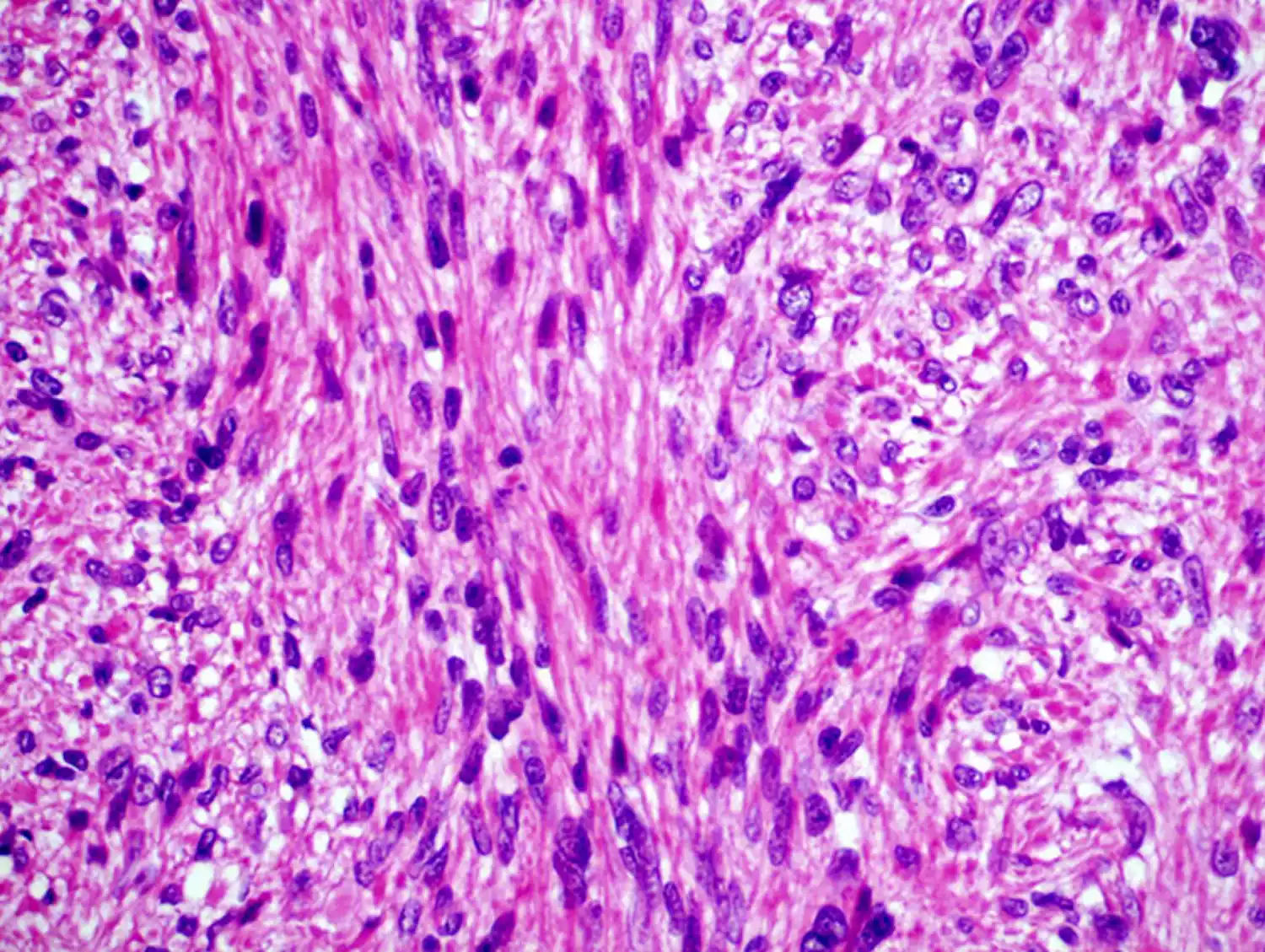
The tumors can develop from any area in which smooth muscle is present in the uterus, the gastrointestinal tract, blood vessels, and even the skin. They are identified by an increase in mitotic activity, cell abnormalities, and usually the presence of necrosis in the tissue. Because of their aggressive nature early detection, correct diagnosis, and timely treatment are vital to improving the outcomes of patients.
Importance of distinguishing between benign and malignant tumors
- Nature and Behavior of Growth:
- Bony tumors: such as leiomyomas develop locally and do not infiltrate nearby tissues or expand across distant organs. They develop at a slower rate and usually have a well-defined border.
- Malignant tumors: such as leiomyosarcomas infiltrate surrounding tissues, can cause metastasis to distant organs, and can develop quickly. The borders of these tumors are typically uneven.
- Treatment Approaches:
- Benign tumors are sometimes discovered without intervention immediately or surgical removal in the event that they cause symptoms.
- Malignant tumors require aggressive treatment such as surgery, chemotherapy radiation, or combinations of these treatments according to the nature and severity of the cancer.
- Prognosis:
- Benign tumors, after removal typically do not recur and are not the risk of life-threatening danger unless their location or size interferes with essential functions.
- Malignant tumors have a chance of recurrence, even after removal. They can also dramatically reduce the lifespan.
- Follow-up and Surveillance:
- People with benign tumors might require regular monitoring, particularly when the tumors have not been completely removed.
- Patients with malignant tumors require regular and consistent follow-up in order to look for recurrence and metastasis, as well as to evaluate the efficacy of treatment.
- Psychological Impact:
- The diagnosis of malignant tumors may have profound psychological consequences which can cause depression, anxiety, and stress, due to the mortality and morbidity dangers.
- Although benign tumors may create anxiety, particularly prior to confirmation of diagnosis, psychological effects are generally less severe.
- Economic and Social Impact:
- Malignant tumors can lead to long-term treatment, hospitalizations, and even time off from work, which can lead to financial difficulties.
- Benign tumors, absent a symptomatic condition could not have as significant an economic impact.
- Genetic and Familial Implications:
- Certain tumors that are malignant are genetically or inherited which makes screening and counseling essential for families.
- Although certain benign tumors may have genetic connections, however, the consequences are typically less serious.
- Informed Decision-making:
- Knowing whether an abnormality is malignant or benign can help patients make informed choices about treatments, lifestyle modifications, and plans for the future.
The distinction between malignant and benign tumors is crucial for guiding the patient’s treatment, setting expectations, planning long-term monitoring, and assessing the potential outcome.
Comparison Table of Leiomyoma and Leiomyosarcoma
Comparison Table: Leiomyoma vs. Leiomyosarcoma
| Aspect | Leiomyoma | Leiomyosarcoma |
|---|---|---|
| Definition | A benign smooth muscle tumor | An aggressive malignant tumor originating from smooth muscle cells |
| Origin | Smooth muscle cells | Smooth muscle cells |
| Common Locations | Uterus (uterine fibroids), gastrointestinal tract, skin | Uterus, gastrointestinal tract, blood vessels, skin |
| Growth Behavior | Localized growth, non-invasive | Invasive, can metastasize to other organs |
| Rate of Growth | Generally slow | Typically rapid |
| Borders | Well-defined | Often irregular |
| Cellular Appearance | Uniform, similar to normal smooth muscle cells | Atypical, with increased mitotic activity |
| Metastasis | Does not metastasize | Has the potential to metastasize |
| Treatment | Observation, hormonal therapy, surgical removal | Surgical removal, chemotherapy, radiation |
| Prognosis | Usually good; non-life-threatening | Variable can be life-threatening depending on stage and location |
| Recurrence after Removal | Rare, especially if fully excised | Possible, especially if not fully excised |
| Hormonal Sensitivity | Often sensitive to hormones like estrogen | Not typically hormone-sensitive |
| Risk Factors | Hormonal imbalances, genetics, age | Genetics, exposure to radiation, certain chemicals |
| Follow-up and Surveillance | Periodic monitoring if not removed | Regular and close follow-ups to monitor for recurrence and metastasis |
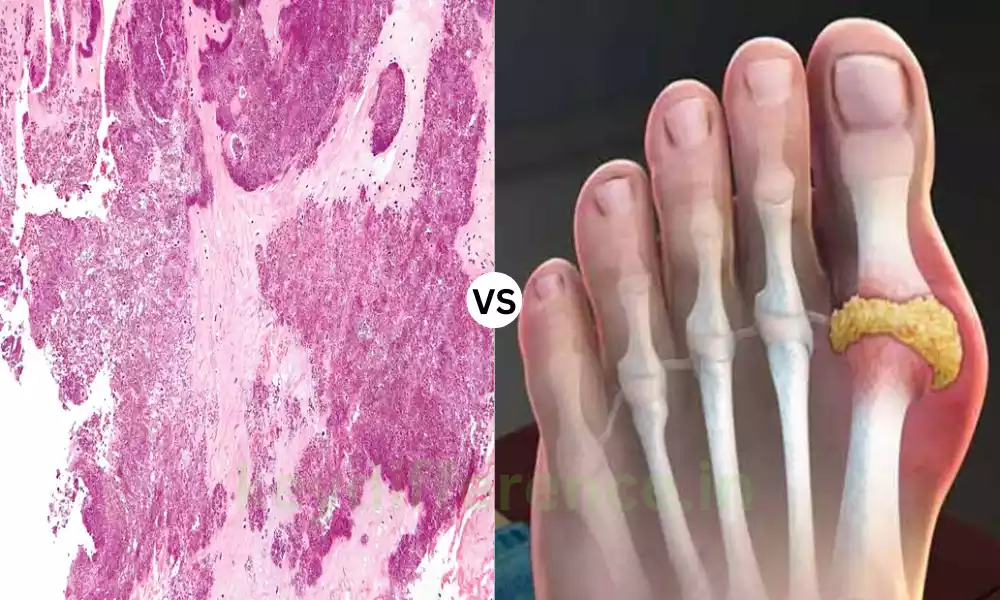
| Histological Characteristics | Smooth muscle bundles with fibrous connective tissue | Cellular atypia, high mitotic rate, possible tissue necrosis |
This table provides a side-by-side comparison of leiomyoma and leiomyosarcoma, highlighting their key differences in various aspects. It’s crucial to consult medical professionals for diagnosis and understanding of individual cases.
Warning signs that might indicate malignancy
Warning Signs That Might Indicate Malignancy
- Rapid growth: The increase in size of a previously stable or slow-growing area over an extended period of time is a concern.
- Tenderness or Pain: Although benign tumors may be uncomfortable sudden pain or a shift in the character of the pain could indicate malignancy.
- Skin Ulceration skin: A malignant tumor that penetrates the skin or causes changes to the skin such as ulceration, could be malignant.
- Unexplained Loss of Weight: A sudden and substantial weight loss that does not have a specific reason could be a sign of cancer.
- Changes in appearance: Any sudden changes in the appearance, color, or texture of a lesion lump could indicate malignant change.
- bleeding or discharge: Unexpected bleeding or discharge from an opening (like the nipple or the rectum) may be alarming.
- Persistent fatigue: Continuous fatigue that is not explained by other factors could suggest malignancy.
- Night sweats or fever: Inexplicably constant fevers or night sweats may be an indication of certain cancers.
- Loss of appetite: A sudden and unproved loss of appetite could be due to malignancy.
- Difficulty swallowing: Progressive difficulties in swallowing (dysphagia) may be a sign of cancer within the throat or the esophagus.
- Persistent cough or hoarseness: A cough that doesn’t go away or hoarseness that lasts more than a couple of weeks should be examined.
- Undiagnosed Anemia: A decrease in red blood cell counts with no obvious cause could be caused by cancer that affects the digestive tract.
- lymph node enlargement: Lymph nodes that are swollen in particular, particularly when they are they are hard or growing, could be an indication of cancer.
- Moles as well as Freckles: Modifications in the appearance, shape size, color, or texture of a freckle or mole or the appearance of moles that appear irregular could indicate skin cancer.
- Irregular borders: In the context of skin lesions ones with jagged, irregular, or blurred edges could be a sign of malignancy.
- Functional Impact: A difficulty in the organ’s function (e.g. changes in bladder habits, bowel function) may be a sign of malignancy.
It’s important to keep in mind whether the appearance of any of these signs does not necessarily indicate cancer. Some of these symptoms could be due to benign conditions or health problems. However, any recurring or unusual symptoms should be examined by a medical professional to determine if there is malignancy and make a precise diagnosis.
Diagnostic procedures and criteria
Diagnostic Procedures and Criteria for Tumors
Differentiating between malignant and benign cancers is a process that involves medical evaluation, imaging, and laboratory studies.
Here are the primary tests and methods used to diagnose:
- Clinical Examination:
- History-taking: understanding the duration, progress of symptoms, the family history, and the risk elements.
- Physical Exam: The examination focuses on the size and shape, consistency, tenderness, mobility, and location of the tumor.
- Imaging Studies:
- X-ray: It is useful for detecting lung lesions or bone tumors.
- Ultrasound: is used to evaluate tissues, specifically in organs such as the thyroid, liver, and breast.
- Mammography: specifically on breast lesions.
- Computed Tomography (CT) Scan: provides detailed images of body structure, useful in assessing the size of tumors, the location of the tumor, and the involvement of nearby structures.
- Magnetic Resonance Imaging (MRI): Provides superior contrast in soft tissue and is particularly beneficial for spinal, brain, and musculoskeletal tumors.
- Positron Emission Tomography (PET) Scan: can help to identify metabolically active lesions that could suggest malignancy.
- Endoscopy: Direct visualization of digestive, respiratory, and Urological tumors.
- Laboratory Investigations:
- Testing for Blood: specific markers such as PSA (for prostate cancer) CA-125 (for ovarian cancer) and AFP (for tumors in the liver) could be a sign of malignancy.
- Full Blood Count: To determine anemia or other blood disorders.
- Tissue Biopsy: It is the standard in diagnosis.
- HD0_ Needle Aspiration (FNA): Utilizes a fine needle to remove cells from a tumor.
- Core Needle Biopsy: uses a bigger needle to obtain an organ sample.
- The Excisional and Incisional biopsy: The part (incisional) or whole (excisional) of the tumor is surgically eliminated to allow for an examination.
- Endoscopic biopsy: Tissue samples are collected during endoscopy.
- Histopathological Examination:
- Examines the microscopic structure of the biopsy specimen. It identifies the type of the cells that are involved as well as their arrangement as well as other characteristics like the rate of mitosis.
- Immunohistochemistry uses antibodies to identify specific proteins, which can help in tumor classification.
- Molecular and Genetic Testing:
- Finds specific molecular and genetic changes within tumor cells, which aid in the diagnosis as well as prognosis and treatment plan.
- Staging: For malignant tumors.
- The TNM system: Classifies tumors based on size (T) as well as Lymph Node involvement (N) and the existence of Metastasis (M).
- Other Staging Systems: Vary according to the kind of cancer.
- Other Diagnostic Procedures:
- Bone Marrow Biopsy: particularly for cancers that are hematological.
- Lumbar Puncture: To evaluate the spinal cord for tumors.
An accurate diagnosis is the use of a variety of methods specific to the patient’s symptoms and the suspected type of tumor. Always it is best to use a multidisciplinary approach. ideal, which includes pathologists, radiologists, and experts in the area.
Adjuvant therapies like chemotherapy and radiation
Adjuvant Therapies: Chemotherapy and Radiation
Adjuvant therapy refers to a procedure used in conjunction with the primary, principal, or first treatment in order to increase the effectiveness of treatment, typically with the intention of reducing the chance of cancer returning. The most frequently used adjuvant treatments for treating cancer include chemotherapy and radiation.
- Chemotherapy
Definition: Chemotherapy makes use of medications to stop or limit the growth of cancerous cells.
Application in Adjuvant Setting:
- Post-surgery, the drug is administered to destroy any remaining cancerous cells which may not be surgically removed.
- Reduces the chance of Recurrence.
- The precise medication (or combination) of medications will depend on the stage and type of cancer.
Methods of Administration:
- Oral: Oral tablets, capsules.
- Intravenous (IV): Injected into the vein.
- Intramuscular (IM): Injected into the muscle.
- Subcutaneous: Injected under the skin.
- Intrathecal: Injected in the spinal canal.
- Directly into an organ or the site of the tumor.
Side Effects:
- Nausea and vomiting.
- Hair loss.
- Fatigue.
- Infection risk results from a decrease in white blood cells.
- Anemia.
- Tendencies to bleeding due to a decrease in platelets.
- A change in the appetite.
- Mouth sores.
- Radiation Therapy (or Radiotherapy)
Definition: Utilizes radiation with high doses (X-rays Gamma rays as well as charge particles) to kill cancerous cells and shrink the size of tumors.
Application in Adjuvant Setting:
- The procedure is used post-surgery to kill remaining cancerous cells within the area of treatment.
- Reduces the possibility of recurrence within the radiation region.
- The exact method and dosage will depend on the type of cancer stage, location, and type.
Methods of Delivery:
- External beam radiation: Radiation that is emitted by a body part outside and targeted at the cancerous region.
- Internal radiation (Brachytherapy): Radioactive material is inserted inside or close to the tumor.
- Systemic radiation: The radioactive substances are taken in the form of a pill or injection for treatment of certain types of cancer.
Side Effects:
- Fatigue.
- Skin changes occur at the irradiated location (redness dryness).
- Loss of hair in the area of treatment.
- Nausea (especially when the abdomen can be treated).
- Inability to swallow (for radiation that is in the chest or neck area).
- Diarrhea (if the lower pelvis or the lower abdomen are treated).
- Redistribution of blood cell counts.
Both radiation therapy and chemotherapy are designed to increase the chance of a cure and decrease the chance of recurrence when they are used as adjuvant therapies. But, they can have possible side effects, which is why it’s crucial for patients to be aware and closely monitored.
Treatment decisions tend to be based on the stage of the cancer, the type of the disease, location, overall health, and the potential advantages versus the risks.
Expected outcomes with and without treatment
Expected Outcomes with no treatment for malignancies
The anticipated outcomes for patients with malignant tumors differ widely according to the type, stage, and location of the tumor and also the general health and aging that the person.
Here’s a summary of what to expect:
- With Treatment:
- Higher Survival Rates: The treatment process can often extend the life span of patients. For certain cancers that are early-stage, treatment may be curative.
- Reduced symptoms: The treatment can help alleviate symptoms caused by tumors like obstruction, pain, or bleeding.
- Prevention of spread: Treatment of the primary tumor may stop or slow the process of metastasis (spread) into other areas in the body.
- Maintaining Function: Treatments may help to maintain the functionality of the organ that is affected by cancer.
- Better quality of life: Relief from symptoms and the possibility of a longer longevity can improve overall health however, adverse effects of treatments may affect your quality of life in the short term.
- The possibility of recurrence: In spite of treatment it is possible to experience cancer recurrence. However regular follow-up and monitoring can identify and deal with instances of recurrence early.
- Without Treatment:
- Progression of the disease: The tumor could increase in size and infiltrate surrounding organs or tissues.
- Metastasis: If not treated the cancer may expand to other parts of the body. which can affect many organs and systems.
- Amplification of Symptom Burden: The symptoms caused by tumors or their metastasis (like fatigue, pain breathing problems, etc.) tend to worsen with time.
- Reduced Survival: If not treated numerous malignancies can cause premature death. The timeframe for treatment varies greatly depending on the type of cancer and severity of the cancer.
- Complications: The tumor expands and becomes infected with the bowel, which could cause complications. For instance, a tumor in the bowel could create obstructions or lung cancer could result in respiratory failure.
- Declining quality of life: Physical decline, pain, and other signs can have a significant impact on the health of a patient as well as their everyday functioning.
It’s important to know that for certain cancers in the early stages of tumors found in patients with major health issues, the best strategy is patiently waiting for symptom control without the need for aggressive treatment. For the majority of cancers, particularly those that are aggressive treatment is the best chance of a successful result.
Each patient’s case is different for each patient. Treatment decisions must be made in conjunction with healthcare professionals. They should consider the particular type and stage of cancer, the overall health, the potential advantages and dangers of treatment, as well as the patient’s values and preferences.
Similarities Between Leiomyoma and Leiomyosarcoma
Both leiomyomas as well as leiomyosarcoma are in smooth muscle cells. They share some similarities in appearance and features.
Here are some similarities between them:
- Source of Tissue: The two leiomyomas and leiomyosarcoma originate in muscles that are smooth. The type of tissue is present in a variety of areas within the human body such as the uterus, the gastrointestinal tract, as well as blood vessels.
- Location: The two can be found in similar places, particularly in the uterus. But, they can also be present in the gastrointestinal tract, the skin, or blood vessels.
- Appearance: Particularly in the beginning stages, or without detailed imaging it is often difficult to discern between the two solely on their appearance. Both are able to appear as solid masses.
- Symptoms: Both tumors may result in similar symptoms depending on their size and location. For instance, if they are located in the pelvis, they both could create pelvic pain irregular bleeding, or signs of pressure.
- hormonal influence Leiomyomas, particularly in the uterus, may be affected by hormonal levels (e.g. estrogen). Although leiomyosarcomas generally aren’t as sensitive to hormones as leiomyomas some instances may display sensitivity to hormones.
- Image Overlap: When using imaging modalities such as ultrasound CT as well as MRI the tumors of both look similar, and a biopsy is essential for a clear diagnosis.
- Surgery Management: The two types of leiomyoma leiomyosarcoma may require surgery in their treatment. In the case of leiomyoma, it could be for relief from symptoms as well as for leiomyosarcoma. it’s typically for the removal of tumors and is an essential part of treatment.
It is crucial to comprehend these resemblances since they highlight the need for specific diagnostic procedures to differentiate between benign (leiomyoma) and malignant (leiomyosarcoma) diseases. The correct differentiation can ensure the most prompt and effective treatment.
Conclusion
Leiomyoma and leiomyosarcoma both, while stemming out of similar smooth muscle cells, and sharing some similarities in appearance and site, differ greatly in their biology as well as the potential risk and the implications of treatment.
Leiomyoma is a benign growth, while leiomyosarcoma is an aggressive, malignant, and dangerous tumor. Making the right distinction between these two is vital because it determines the prognosis and treatment of the individual. Comprehensive diagnostic procedures, such as biopsy and imaging, are crucial to ensure precise differentiation, allowing timely and appropriate treatments.