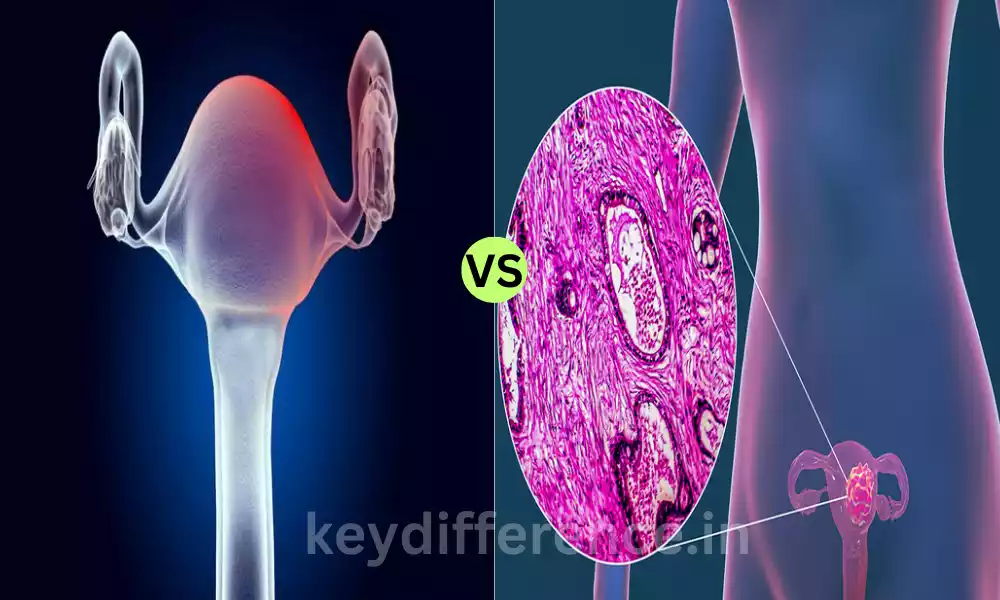
Polycythemia Vera and Essential Thrombocythemia are two distinct myeloproliferative tumors both of which are characterized by abnormal manufacturing of blood cells. Although they share some similarities with respect to genetic changes and the possibility of complications, they have significant differences in the primary involvement of blood cells in the clinical presentation and treatment.
This outline of content will dive into these differences, assisting in understanding the difference between ET and PV, while highlighting the importance of a precise diagnosis and customized treatment strategies.
Explanation of Polycythemia Vera
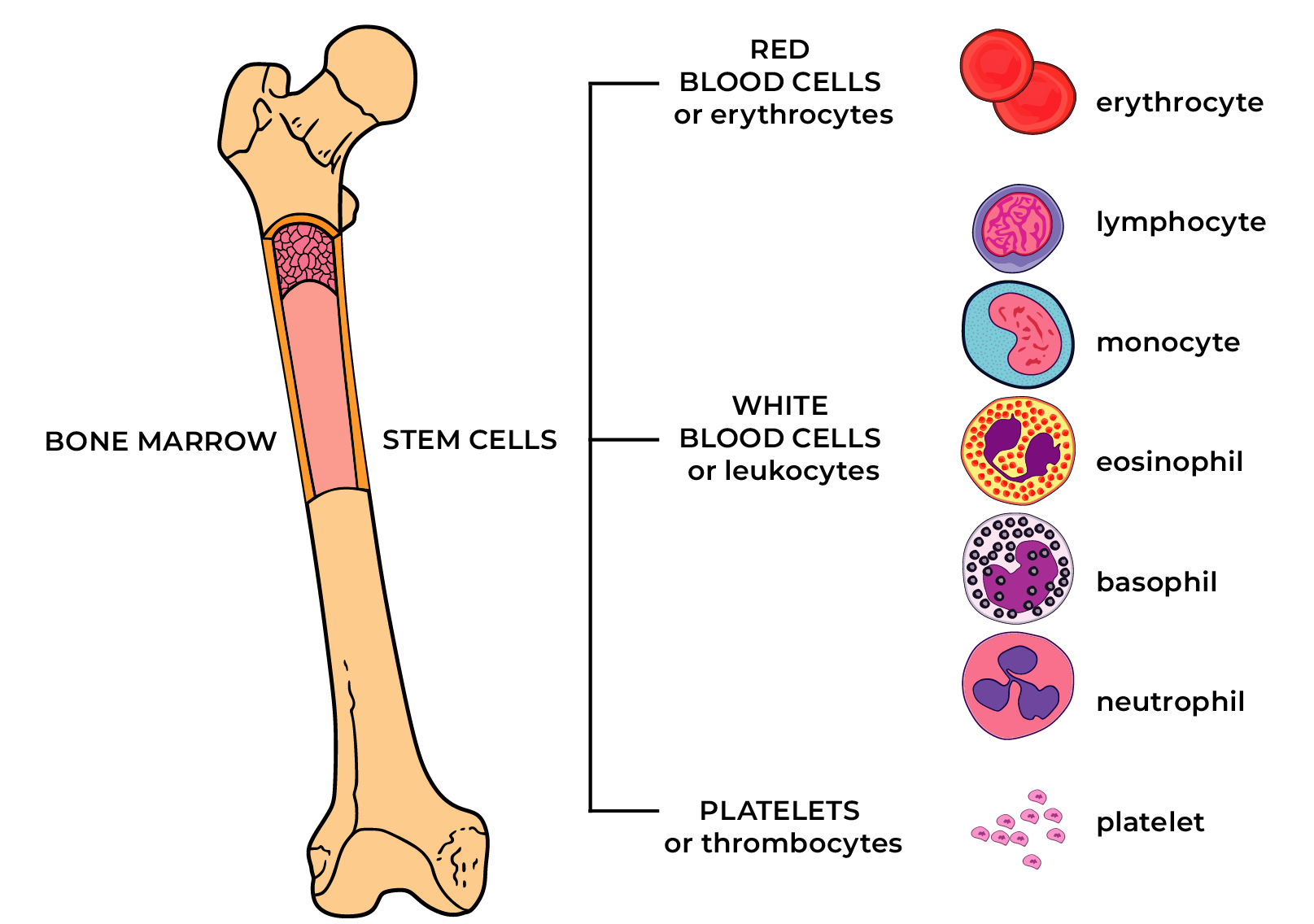
Polycythemia Vera (PV) is an uncommon, chronic, as well as progressive disorder of blood that is classified as a myeloproliferative tumor. In the bone marrow of patients, it produces a high amount of blood red cells as well as white blood cells and platelets.
This excess production of blood cells could result in an increase in the thickness of blood (viscosity) and an increased chance of developing blood clots. The condition is typically caused by erythrocytosis.
It is a condition that causes an increase in the number of red blood cells and is usually linked to genetic disorders, including that of JAK2. PV may cause various issues, including the increased chance of thrombosis (such as heart attacks) as well as myelofibrosis (a condition in which bone marrow gets scarred) and occasionally it can lead to the development of acute leukemia.
Treatment usually focuses on reducing the amount of blood cells and minimizing the risk of blood clotting. PV requires continuous medical surveillance and treatment to avoid complications and enhance the patient’s overall health.

Explanation of Essential Thrombocythemia
Essential Thrombocythemia (ET) is a rare myeloproliferative tumor (MPN) that is distinguished by the excessive production of platelets (thrombocytosis) within the bone marrow.
Contrary to Polycythemia Vera (PV), in ET it is not a significant rise in red blood cells or white blood numbers. The main problem is the over-production of platelets that could increase the risk of bleeding and the formation of clots (thrombotic) incidents.
ET is usually caused by particular genetic disorders, which include mutations in genes like JAK2, CALR, or MPL. These mutations play a significant part in the diagnosis and classification of ET.
Many people with ET remain unaffected and are diagnosed by regular blood tests some may be afflicted with symptoms like headaches or dizziness, vision issues, or an overly large spleen (splenomegaly). ET may also cause complications, such as strokes, blood clots as well and bleeding incidents.
Treatment of ET usually involves taking steps to decrease the chance of clotting such as low-dose aspirin therapy, and sometimes cytoreductive medicines to reduce the number of platelets in cases with high risk. Monitoring and regular follow-up are vital to managing ET efficiently and avoiding complications.
Importance of distinguishing between PV and ET
Differentiating the difference between Polycythemia Vera (PV) and Essential Thrombocythemia (ET) is vitally important in the field of oncology and hematology for a variety of significant reasons:
- Treatment Choice: Treatment and management strategies for ET and PV differ greatly. PV typically requires treatments designed to reduce the excess red blood cell production like phlebotomy. ET concentrates on regulating platelet counts and decreasing the chance of clotting using drugs like aspirin or cytoreductive drugs. A precise diagnosis will ensure that patients receive appropriate and effective treatment and improve their health and their prognosis.
- Risk assessment: PV has an increased chance of suffering from thrombotic events such as strokes and heart attacks because of the increased blood viscosity. However, ET is most commonly linked to clotting and bleeding risks associated with elevated platelet counts. The distinction between the two conditions aids in determining a patient’s risk profile precisely, which allows the patient to take individualized preventive steps.
- Monitoring and Follow-up: Regularly monitoring blood counts and progression of the disease is crucial for both ET and PV patients. However, the frequency and purpose of the monitoring can vary. Patients suffering from PV might require more frequent checking of red cell parameters and ET patients might require greater monitoring of platelet counts. An accurate diagnosis helps health professionals establish the appropriate monitoring schedules and can detect the progression of disease or any complications in time.
- Prognosis: Knowing if the patient is suffering from ET or PV may significantly affect the outlook. PV is usually associated with a greater risk of progressing to myelofibrosis, or acute leukemia in comparison to ET. A precise diagnosis can help in predicting the probable course of the disease providing better long-term care and counseling for patients.
- Genetic testing: The genetic changes related to the PV (JAK2) as well as ET (JAK2, CALR, MPL) are distinct. The identification of the specific mutation in a blood disorder of a patient will help confirm the diagnosis and adjust treatments in line with the diagnosis. It also assists in counseling genetically impaired patients as well as their family members.
- Research and Clinical Trials: Differentiating between ET and PV is crucial for clinical research. Researchers who study these diseases require precise patient classifications in order to design targeted treatments and increase knowledge of the root mechanisms.
In short, the accurate distinction between ET and PV is essential for proper treatment selection and monitoring, risk assessment and prognosis assessment as well as genetic testing and research efforts. It is directly affecting the management and treatment of patients suffering from these neoplasms. This makes it a crucial element within the field of Hematology as well as oncology.
Comparison Table of Polycythemia Vera and Essential Thrombocythemia
Certainly, here’s a comparison table outlining the key differences between Polycythemia Vera (PV) and Essential Thrombocythemia (ET):
| Characteristic | Polycythemia Vera (PV) | Essential Thrombocythemia (ET) |
|---|---|---|
| Disease Classification | Myeloproliferative Neoplasm (MPN) | Myeloproliferative Neoplasm (MPN) |
| Genetic Mutation | JAK2 Mutation (often present) | MPL Mutation (sometimes present) |
| Main Blood Cell Affected | Red Blood Cells | Platelets |
| Increased Cell Production | Red Blood Cells (Erythrocytosis) | Platelets (Thrombocytosis) |
| Hematocrit Levels | Elevated | Normal or slightly elevated |
| Platelet Counts | Normal or slightly elevated | Elevated |
| Clinical Symptoms | Headache – Fatigue – Pruritus (itchiness) – Sweating, especially at night – Vision changes | Headache – Fatigue – Pruritus (itchiness) – Sweating, especially at night – Vision changes |
| Complications | Thrombosis (blood clots) – Cardiovascular issues – Splenomegaly (enlarged spleen) | Bleeding – Thrombosis (blood clots) – Cardiovascular issues |
| Diagnosis | Elevated Hematocrit – JAK2 Mutation Testing – Bone Marrow Biopsy | Elevated Platelet Count – MPL Mutation Testing (if present) – Bone Marrow Biopsy |
| Treatment | Phlebotomy (bloodletting) – Hydroxyurea – JAK Inhibitors (in some cases) | Low-dose aspirin – Hydroxyurea – Interferon-alpha (in some cases) – Anagrelide (in some cases) |
| Prognosis | Risk of myelofibrosis or leukemia transformation – Regular monitoring required | Risk of thrombotic events – Long-term antiplatelet therapy – Monitoring platelet counts |
Please note that the presentation and severity of these conditions can vary among individuals, and treatment plans are tailored based on the specific needs and risks of each patient. Always consult a healthcare professional for accurate diagnosis and appropriate management.
Abnormal proliferation of red blood cells, white blood cells, and platelets
The excessive proliferation of red blood cells white blood cells and platelets is the condition in which the blood cell types mentioned above are produced in high amounts by bone marrow. This condition can manifest in a variety of medical conditions, such as myeloproliferative tumors such as Polycythemia Vera (PV) and Chronic Myeloid Leukemia (CML).
This is a more thorough explanation of this abnormality:
- Red Blood Cells (RBCs): In normal circumstances, the creation of blood red cells can be controlled by the body’s response to oxygen levels. However, under conditions like PV, there’s a growth in red blood cell production that is not influenced by the body’s need for oxygen. This can result in a higher quantity of blood red cells within the bloodstream. This can cause an increase in volumetric viscosity (thickness).
- White Blood Cells (WBCs): Abnormal growth of cells called white blood could be seen in a variety of disorders that include certain forms of leukemia as well as myeloproliferative tumors. In these instances, bone marrow is responsible for producing an overabundance of cells called white blood cells which could compromise the immune system’s ability to function and cause symptoms such as fatigue and susceptibility to infection.
- Platelets: The term “platelets” refers to small blood cell fragments which play an essential role in blood clotting. In the case of Essential Thrombocythemia (ET), there is an abnormal growth of platelets in bone marrow.This results in an increase in platelet count within the bloodstream. This may increase the likelihood of forming blood clots that can lead to the occurrence of thrombotic events, such as strokes or deep vein thrombosis.
The abnormal growth of these types of blood cells is typically attributed to genetic changes that alter the signaling pathways that regulate the production of blood cells. These mutations may lead to uncontrolled expansion and division of precursors to blood cells within the bone marrow.
Treatment and management of diseases that are characterized by abnormal blood cell proliferativeness typically involves treatments aimed at regulating blood cell counts, decreasing the chance for complications (such as bleeding, and clotting), and addressing root causes of the genetic mutations, if applicable.
A precise diagnosis and customized treatment plans are vital for improving the outcomes of patients and improving quality of life.
Increased risk of thrombosis (stroke, heart attack)
A greater chance of thrombosis, which includes diseases like stroke and heart attacks, is a serious issue for specific medical issues, especially ones that are characterized by irregular blood cell growth and/or clotting tendencies.
This is how these conditions may result in an increased risk of thrombosis:
- Polycythemia Vera (PV): In PV there is an abnormal growth in the number of blood red cells present in the bloodstream. The increase in red blood cells could cause an increase in volumetric viscosity (thickness) and make it difficult for blood to flow freely across blood vessels.In turn, the chance of blood clots appearing in veins and arteries is increased. The clots may result in serious thrombotic incidents like stroke (if the clot stops cerebral blood circulation) or heart attacks (if it is found in the coronary arteries that supply your heart muscles).
- Essential Thrombocythemia (ET): ET is defined by an unnatural rise in platelet production that results in elevated platelet numbers. Platelets are vital to clotting blood, but when their levels are too high, they can increase the likelihood of malfunctioning in the formation of clots. Platelet-rich clots may block blood vessels, leading to the occurrence of thrombotic events such as heart attacks, strokes, or clots in different parts of the body.
- Another Myeloproliferative Neoplasms (MPNs): In addition to ET and PV other MPNs, including Chronic Myeloid Leukemia (CML) can cause an increased chance of developing a thrombosis. In CML it is possible to observe an increased amount of the white blood cell count (particularly Granulocytes) and this can contribute to the formation of blood clots.
To lessen the risk of thrombosis that is that is associated with these diseases, medical treatment generally consists of:
- Phlebotomy: In the PV procedure, phlebotomy for therapeutic purposes is done to reduce blood thickness by eliminating extra red blood cells.
- Aspirin: Aspirin with a low dose is frequently prescribed to prevent platelet aggregation as well as decrease the chance of clots forming in both ET and PV.
- Cytoreductive Therapy: Drugs such as interferon or hydroxyurea can be used to lower blood cell counts, and reduce the chance of developing thrombosis.
- Anticoagulants In certain instances anticoagulant medicines are prescribed to help prevent the formation of clots or help treat existing clots.
Monitoring blood counts regularly as well as other factors that increase risk are crucial in identifying and managing thrombotic risks efficiently in people who suffer from these ailments. It’s essential for healthcare professionals to develop treatment plans in accordance with the particular requirements and risk profile of every patient.
The risk of complications remains, especially with high platelet counts
When it comes to Essential Thrombocythemia (ET), the chance of developing complications, including thrombotic as well as bleeding events, is still important, particularly when there is an ongoing increase in platelet count. This is a critical factor in managing ET.
Let’s take a closer analysis of why the risks continue to exist:
- Thrombotic events: Increased platelet counts during ET increase the chance of blood clot formation which could lead to thrombotic events. These can affect a variety of organs of the body for instance, the brain (resulting in strokes) and the cardiovascular system (leading to heart attack) as well as other organs. Platelets play an essential part in the formation of blood clots. Therefore, when they’re in high numbers they are more likely to clot.
- Blood clotting complications: In paradox despite the focus on the risk of thrombosis, certain people who suffer from ET might also be afflicted with bleeding-related complications. This is due to the fact that the high levels of platelets can trigger abnormal platelet function leading to a decrease in blood clotting and bleeding-related tendency. The bleeding could manifest as nosebleeds easily bruising, or even digestive bleeding.
- Risk stratification: Risk stratification is essential for managing ET. Healthcare professionals evaluate each patient to assess their risk of developing complications from thrombosis. Patients at high risk, especially those who have risk factors that are not present (such as being over 60 years old an underlying thrombosis history, or a JAK2 mutation) could require more aggressive treatments to lower platelet counts and reduce the chance of developing clots.
- Aspirin Treatment: A low-dose aspirin is commonly recommended for ET patients to reduce the chance of thrombotic incidents by stopping platelet aggregate. However, it might not completely eliminate the risk for those at risk, and further treatment with cytoreductive therapy could be required.
- Monitor regularly: Monitoring closely platelet counts as well as other risk factors is essential in controlling ET. Treatment plans can be based on fluctuations in the platelet count as well as the overall risk profile of the patient.
- individualized treatment: Treatment strategies for ET should be customized and take into consideration the patient’s age and overall state of health, the risk factors, and signs. For patients at high risk, cytoreductive therapy using drugs such as interferon or hydroxyurea may be suggested to decrease the number of platelets and decrease the risk of thrombosis.
The treatment of ET is about managing the risk of thrombosis and bleeding-related complications, especially those with platelet counts that are elevated. A customized approach to treatment and continuous monitoring is essential to improve the treatment and quality of life for those suffering from ET.
Similarities Between Polycythemia Vera and Essential Thrombocythemia
Polycythemia Vera (PV) and Essential Thrombocythemia (ET) are both myeloproliferative tumors (MPNs) that cause an abnormal proliferation of cells in the bone marrow.
While they differ they have some commonalities which include:
- Clonal Disorders: Both ET and PV are caused by clonal diseases of hematopoietic stem cell populations in the bone marrow. In both one abnormal stem cell leads to a cloned population of similarly infected blood cells.
- Genetic Mutations: One of the major similarities is the existence of specific genetic mutations in these diseases. The most prevalent mutation observed within the two conditions PV ET and PV ET is the JAK2 mutation that plays an important part in the pathogenesis of both diseases. Yet, ET can also be related to CALR as well as MPL mutations in a few instances.
- Risk of thrombosis: the conditions PV as well as ET have been linked with a greater chance of developing thrombotic events. That means that people who suffer from either of these conditions have a greater chance of developing blood clots. This could cause serious problems such as cardiac attacks or the formation of clots in other areas of the body.
- Bone Marrow Examining: Diagnostically, both ET and PV typically involve a bone marrow exam. This test allows healthcare professionals to determine the composition of cells in the bone marrow. They can also detect abnormal cell proliferation and determine genetic mutations that are typical of these disorders.
- treatment modalities: Treatment strategies vary between ET and PV however, they both share a few common strategies. Both conditions can require the treatment of cytoreductive therapy in order to reduce the number of blood cells and lower the chance of complications. In addition, low-dose aspirin is commonly used to prevent thrombosis in both ET and PV. ET.
- Continuous Monitoring: Both ET and PV require continual medical monitoring to monitor blood counts, treat symptoms, and modify treatment as required. Regular follow-up visits to medical professionals are vital to track the progression of disease and the response to treatment.
- Health Impact: The two conditions may influence a patient’s quality of life because of symptoms associated with increased blood cell counts, like headache, fatigue, and an increased chance of clotting or bleeding events. Strategies for managing the condition aim to improve the health of patients and lessen the severity of symptoms.
While there are some similarities between ET and PV there are some significant differences, particularly in relation to the primary blood cells involved (red blood cells of PV and platelets of ET) and the particular issues and treatments related to each. Therefore, precise diagnostics and differentiation are vital for the correct management of each condition and for maximizing the patient’s outcomes.
Reference Books
Certainly! Here are some reference books on various topics that you might find valuable:
General Knowledge and Reference:
- “The New Encyclopedia of Modern Bodybuilding” by Arnold Schwarzenegger
- “The World Almanac and Book of Facts” by Sarah Janssen (Annual Publication)
- “The Oxford English Dictionary” by John Simpson and Edmund Weiner
Science and Technology:
- “Cosmos” by Carl Sagan
- “A Short History of Nearly Everything” by Bill Bryson
- “The Feynman Lectures on Physics” by Richard P. Feynman
- “The Selfish Gene” by Richard Dawkins
History:
- “A People’s History of the United States” by Howard Zinn
- “Guns, Germs, and Steel: The Fates of Human Societies” by Jared Diamond
- “Sapiens: A Brief History of Humankind” by Yuval Noah Harari
Literature and Writing:
- “The Elements of Style” by William Strunk Jr. and E. B. White
- “The Oxford Companion to English Literature” edited by Margaret Drabble
- “On Writing: A Memoir of the Craft” by Stephen King
Philosophy:
- “Meditations” by Marcus Aurelius
- “Sophie’s World” by Jostein Gaarder
- “Critique of Pure Reason” by Immanuel Kant
Conclusion
These reference books can be valuable sources for learning about a variety of topics. When it comes to the complexities of history, science literature, or even philosophy books provide many sources of information and insights.
They serve as a base for research, education, and personal development and are essential for those who want to discover and comprehend the world that surrounds them.