Immunity, the body’s defense system against invaders from outside, may malfunction at times. If it is mistakenly targeting our own tissues, autoimmune illnesses develop. However, when it is unable to defend us properly and causes immune deficiencies, they can occur.
Although they are on opposite sides of the spectrum of immune system responses both diseases share fascinating similarities. This article explores the similarities, differences, and the unique intersection in which both conditions may coexist in the same person.
What is Autoimmune Disease?
An autoimmune disorder is a condition that occurs when the immune system of the body mistakenly detects its own tissues, cells, and organs, as invaders from another country, and initiates the attack. The faulty immune response could cause swelling, tissue damage, and even dysfunction in the organs affected.
The precise reason behind how the immune system reacts against cells in the body isn’t known however, it is believed to be a mixture of environmental, genetic, and hormonal influences. For instance, rheumatoid arthritis Type 1 diabetes, and Lupus erythematosus.

What is Immune Deficiency?
Immune deficiency, sometimes referred to as immunodeficiency refers to a condition in which the immune system’s ability to ward against infectious agents (like viruses, bacteria as well as fungi) is diminished or absent.
This may result in an increased susceptibility to infections, long recovery times, and, in certain cases, the infections that are normally thought to be considered harmless, can become severe or even fatal.
Immune deficiencies can be caused by genetics (present in the womb due to genetic causes) as well as acquired (developed later in life as a result of external causes). Some examples include common variable immune deficiency (CVID) as well as acquired immune deficiency syndrome (AIDS) that results from HIV infection.

Comparison Table of Autoimmune Disease and Immune Deficiency
Certainly! Here’s a comparison table highlighting the primary differences between autoimmune diseases and immune deficiencies:
| Feature/Aspect | Autoimmune Disease | Immune Deficiency |
|---|---|---|
| Basic Definition | The immune system mistakenly attacks the body’s own tissues. | The immune system’s ability to fight infections is compromised or absent. |
| Nature of Dysfunction | Overactive or misguided immune response. | Underactive or absent immune response. |
| Target of Dysfunction | Body’s own tissues or organs. | External pathogens (e.g., bacteria, viruses). |
| Common Causes | Genetic factors – Environmental triggers – Hormonal changes | Genetic mutations (primary) – External factors like infections, treatments, or malnutrition (secondary) |
| Examples | Rheumatoid arthritis – Type 1 diabetes – Systemic lupus erythematosus | Common variable immunodeficiency (CVID) – HIV/AIDS |
| Treatment Approaches | Immunosuppressive drugs – Symptom-specific treatments | Boosting the immune system – Antibiotic prophylaxis – Immunoglobulin therapy |
This table provides a concise comparison between the two conditions. Each can be delved into further for a more comprehensive understanding.
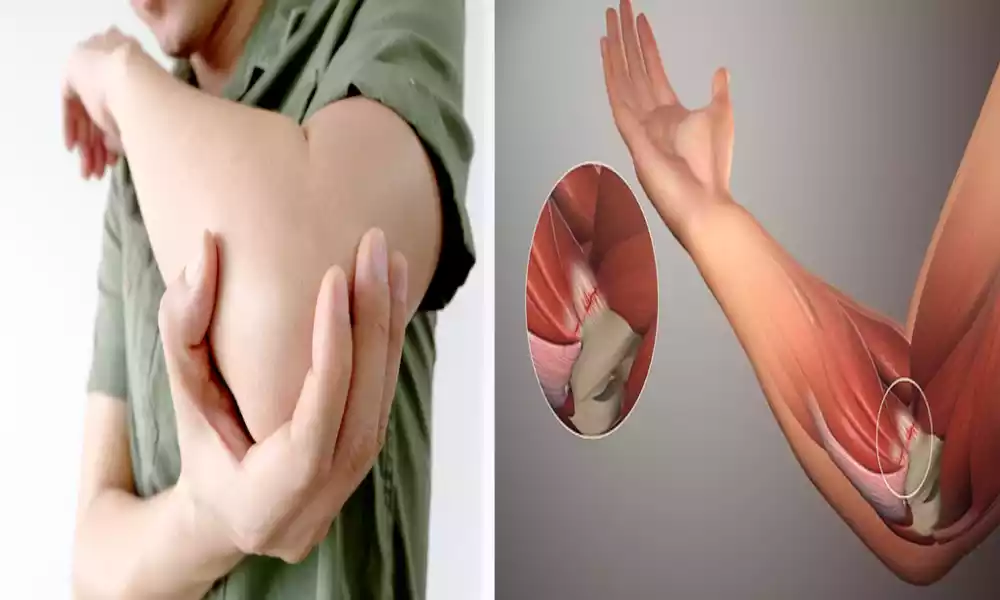
Physical therapy and lifestyle adjustments
The practice of physical therapy (PT) along with lifestyle changes is frequently recommended to people who suffer from a variety of health conditions such as autoimmune diseases and other diseases. They play an important part in managing symptoms improving function and improving overall health.
Here’s a brief outline of the importance of both of them in the area of health management:
Physical Therapy (PT)
- Purpose :
- Restore or enhance physical functionality.
- Help ease pain and discomfort.
- Control or prevent chronic health problems.
- Benefits :
- Enhances Mobility: helps patients get better mobility, especially following surgeries or injuries.
- Treatment for Pain: It can be a viable alternative to opioids, or lower the need for prescriptions.
- Strengthening: targets weak muscle groups to increase performance and decrease the risk of injury.
- Flexibility: Enhances flexibility, while reducing pain and stiffness.
- Postural Corrections: address imbalances within the body, frequently decreasing pain and preventing injuries.
- Conditions that benefit from PT :
- Rheumatoid arthritis
- Osteoarthritis
- Multiple Sclerosis
- Fibromyalgia
- Recovery from surgery
- Techniques :
- Manual Therapy: Techniques that involve hands, such as massage manipulatives, mobilizations, or massages.
- Therapy Exercises: Specific exercises targeted at particular muscles or movement patterns.
- Modalities: The most common are ultrasound or electrical stimulation, and therapy with cold and heat.
Lifestyle Adjustments
- Purpose :
- Improve overall well-being and overall health.
- Control and ease the symptoms of illnesses and conditions.
- Reduce the chance of the disease progressing or an onset.
- Key Adjustments :
- Dietary changes: Anti-inflammatory diets Gluten-free diets, gluten-free diets, or other diets that are special based on the condition.
- Exercise: Regular physical activity that is adapted to the individual’s capabilities and health condition.
- The concept of stress management: Techniques include meditation deep breathing exercises and yoga.
- The importance of sleep hygiene: Insuring good quality and adequate sleep.
- Avoiding triggers: These could involve allergens, foods, or environmental factors which can cause a worsening of conditions.
- Regular health check-ups Monitor the state of your health and change treatments if needed.
- Benefits :
- Improved quality of life: Feel better every day with more energy and less ailment.
- Reduced Needs for Medication: In certain situations, lifestyle changes can decrease the requirement for certain medications.
- Disease Prevention: Healthful lifestyles can stop the development or progression of a variety of conditions.
- Support :
- Counseling, support group therapy, or support groups can help individuals deal with the emotional challenges of changing lifestyles or managing chronic illnesses.
Both physical therapy and lifestyle adjustments emphasize a holistic approach to health, focusing not just on treating symptoms but on improving overall quality of life.
Treatments like chemotherapy
Chemotherapy is one type of treatment for cancer that employs drugs to slow or destroy the growth of cancerous cells. Although it is most commonly used in conjunction with treatment for cancer chemotherapy is also employed in other conditions particularly autoimmune disorders to reduce the body’s immune system.
This article will provide a comprehensive overview of chemotherapy:
Chemotherapy: An Overview
- Purpose:
- Treatment for cancer: to reduce tumors, stop cancer recurrence, ease symptoms, and in certain instances, treat the cancer.
- Immune Suppression: Use in smaller doses to treat conditions that cause autoimmune disease and to make the body more receptive for organ transplantation.
- How It Works:
- Specialized for the cell cycle: targets cells at various stages of their development.
- Cell Cycle Un-specific: works on cells regardless of their stage during the growth cycle.
- Delivery Methods:
- Oral: in pills or in liquid forms.
- Intravenous (IV): Directly into the bloodstream.
- Intramuscular (IM): Into the muscle.
- Topical: Apply to the skin.
- Intrathecal: Directly into the spinal column.
- Common Side Effects:
- Short-term: Nausea, vomiting, hair loss, fatigue, low blood count.
- Long-term: possible harm to vital organs such as kidneys, the heart, or the lungs Secondary cancers; problems with fertility.
- Benefits:
- Effective: Effectively shrinks tumors, or even treats certain kinds of cancer.
- Flexible: can be used in conjunction with other treatments, such as surgery, radiation, or targeted treatments.
- Challenges:
- Toxicity: can harm healthy cells, resulting in adverse consequences.
- Resistance: Certain cancer cells could become resistant in time.
- Use in Non-Cancer Conditions:
- Autoimmune Diseases: conditions like lupus rheumatoid arthritis or multiple sclerosis can be treated using smaller doses of chemotherapy in order to block the immune system.
- Bone Marrow Transplant: This is used to kill the bone marrow prior to transplantation.
- Organ Transplants: suppress the immune system to stop the rejection of organs.
When receiving chemotherapy, it’s crucial for patients to be closely monitored by their healthcare providers to manage side effects and ensure the treatment’s effectiveness. The choice to use chemotherapy, whether for cancer or other conditions, is made after careful consideration of the benefits versus potential risks.
Bone marrow or stem cell transplants for severe cases
Bone marrow and stem cell transplants are medical procedures that are highly advanced and treat a variety of illnesses, including blood-related diseases and certain cancers. The aim is to replace damaged cells (like those that have been damaged by radiation or chemotherapy) using healthy stem cells that restore and regenerate the patient’s immune system.
Here’s a deeper look:
Bone Marrow/Stem Cell Transplants: An Overview
- Types of Transplants:
- Autologous Transplant: Utilizes the stem cells of the patient. It is commonly used to treat conditions such as lymphoma and multiple myeloma.
- Allogeneic Transplant: uses stem cells of a donor. It could be a relative (sibling typically) as well as an individual donor that has an identical type of tissue.
- Sources of Stem Cells:
- Bone Marrow: It is harvested directly from bone, most often the hip.
- Peripheral blood stem cells (PBSC): Collected from the bloodstream following stimulation of the donor by growth factors.
- Cord blood: Stem cells are extracted from the umbilical cord right after birth.
- Preparation for the Transplant:
- Patients are able to undergo high doses of chemotherapy with or without radiation, in order to eliminate the cancerous cells and to make room for stem cells that are being created. This procedure is known as “conditioning” or “myeloablation.”
- Procedure:
- They are then infused with stem cells into the patient’s bloodstream similar to the process of a blood transfusion.
- The cells move to the bone marrow where they start to make new blood cells. This is which is known by the term “engraftment.”
- Post-Transplant Recovery:
- The initial recovery takes place in the hospital in the hospital, where patients are watched for signs of complications.
- The full recovery process can last from weeks to months and requires regular medical checks.
- Benefits:
- It could be curative for certain diseases, such as leukemia or lymphoma.
- Creates a healthier, fresh immune system that will also fight off residual diseases, also known as the “graft-versus tumors. “graft-versus-tumor” effect.
- Risks & Challenges:
- Graft-Versus-Host-Disease (GVHD): Occurs in allogeneic transplants where the transplanted cells inflict harm on the body of the recipient.
- Infections: caused by an impaired immune system following transplant.
- Organ damage: from high-dose radiation or chemotherapy.
- Relapse: The disease that started it could be recurring.
- Uses Beyond Cancer:
- Autoimmune diseases: conditions like systemic lupus erythematosus, or sclerosis, in which other treatments have not worked.
- IBDs that are genetically inherited: such as sickle cell or thalassemia.
- Immunities: like serious combined immune deficiency (SCID).
Bone marrow or stem cell transplants are complex procedures with significant risks, but they also offer the possibility of long-term remission or even cure for certain conditions. Deciding on a transplant involves careful consideration and discussions with medical specialists.
Some treatments for autoimmune diseases can lead to immune deficiency
It’s an important aspect. A lot of treatments for autoimmune disorders are designed to reduce the immune system’s overactive response. Although they may be effective in limiting the process of autoimmune disease they affect immunity, making it more vulnerable to infections as well as other complications. This is essentially pushing the balance of an over-reactive immune system to an inactive one.
Treatments for Autoimmune Diseases Leading to Immune Deficiency:
- Corticosteroids:
- Examples: Prednisone, and methylprednisolone.
- Function: Reduce inflammation and reduce your immune system.
- Risks: Use for a long time can increase the risk of infection and osteoporosis, weight gain, and other ill effects.
- Disease-Modifying Antirheumatic Drugs (DMARDs):
- Examples: Methotrexate, leflunomide, hydroxychloroquine.
- Function: Function to modify or block your immune system.
- Risks: Risks Liver damage, bone marrow suppression, and a higher risk of infection.
- Biologic Agents:
- Examples: Infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira).
- Function: Function to target specific areas that are part of our immune system to lessen inflammation.
- Risks: Reactivation of the tuberculosis latent, an increase in risk of serious infections as well as rare cancers.
- Immunosuppressive Medications:
- Examples: Cyclophosphamide, azathioprine, mycophenolate mofetil.
- Function: The function of HTML0 is to block the immune system’s activities.
- Risks Risks: Greater risk of infection, and risk of liver or kidney damage.
- Selective Immunomodulators:
- Examples: Fingolimod (for Multiple Sclerosis).
- Function: Modify your immune system in a particular way, typically by encapsulating certain immune cells within lymph nodes.
- Risks Risks: Increased risks of viral infection, and potential heart-related consequences.
Considerations :
- Monitoring Infections: Patients who are taking these treatments must be on the lookout for signs of infection like cough, fever, or other unusual symptoms of fatigue and seek medical attention immediately if they develop.
- Immunization: Before beginning immunosuppressive therapy, it’s vital to have current vaccinations. Certain live vaccines can be harmful prior to the start of treatment.
- Regular monitoring: Regular visits to the doctor and blood tests are required to confirm that the medication isn’t causing negative reactions or a major decrease in the immune system.
- Risk-benefit analysis: The potential advantages of these treatments for fighting autoimmune diseases typically outweigh the risks. It is nevertheless essential that healthcare providers and patients be aware of the possibility of complications and to be vigilant.
Although treatments for autoimmune disorders can effectively treat symptoms and slow the progression of the disease they are often accompanied by the risk of the risk of having an immune deficit. Regular monitoring of medical conditions and patient education are essential to making sure that patients are safe and efficient in their treatment of these treatments.
Rare instances where individuals can have both conditions
The combination of an autoimmune disease and an immune deficiency is extremely rare, yet it can happen. The scenarios that arise can be a bit complicated and can present problems in the diagnosis and treatment.
Here are a few examples and situations that could result in this type of overlap:
- Common Variable Immunodeficiency (CVID):
- Description: CVID is one of the most often identified primary immune deficiencies. People suffering from CVID are deficient in serum immunoglobulins. This makes them vulnerable to infection.
- Overlap with Autoimmunity: Infuses Autoimmunity 20% to 30 percent of CVID patients are susceptible to developing autoimmune complications. The most common autoimmune manifestations comprise autoimmune hemolytic anemia (AIHA) and immune thrombocytopenic purpura (ITP).
- Autoimmune Lymphoproliferative Syndrome (ALPS):
- Description: The ALPS genetic disorder in which the body can’t regulate the amount of lymphocytes in its immune system leading to lymphadenopathy as well as splenomegaly.
- Overlap with immunodeficiency and autoimmunity: ALPS patients often suffer from an autoimmune manifestation (like hemolytic anemia, thrombocytopenia, or). They also may suffer from issues of immunodeficiency due to their inability to develop effective reactions to certain pathogens.
- IgA Deficiency:
- Description: It is the most prevalent primary immunodeficiency in which there is the absence or insufficient amount or insufficient levels of immunoglobulin A (IgA) within the blood.
- Infuses Autoimmunity: People who have selective IgA deficiency are more susceptible to autoimmune disorders such as celiac as well as systemic lupus, erythematosus (SLE), and rheumatoid arthritis.
- Immune Dysregulation, Polyendocrinopathy, Enteropathy, X-linked (IPEX) Syndrome:
- Summary: IPEX is a rare genetic disorder that affects the immune system.
- Cross-over with Autoimmunity as well as Immunodeficiency IPEX sufferers IPEX typically have multiple autoimmune signs (like thyroiditis and type I diabetes and skin issues) and immune deficiency-related symptoms which makes them more susceptible to infection.
- Secondary Causes:
- Description: Conditions acquired or interventions may cause both autoimmune disorders as well as immune deficiencies.
- Examples :
- Someone suffering from Rheumatoid Arthritis (autoimmune) receiving treatment by immunosuppressive medications could be diagnosed with secondary immune deficiency due to the drugs.
- The HIV/AIDS virus causes immune deficiencies, but people are also susceptible to developing an autoimmune disorder, such as thrombocytopenic purpura or Sjogren’s syndrome.
The interplay of autoimmune disorders and immunodeficiencies underscores how delicately balanced the immune system is. When the balance of the immune system is disrupted it may result in an array of manifestations of the disease. The proper diagnosis and treatment of these multiple conditions require an integrated approach and knowledge of immunology.
Similarities Between Autoimmune Disease and Immune Deficiency
Immune deficiencies and autoimmune diseases are two distinct types of disorders affecting the immune system. They do have certain similarities in their mechanisms of origin as well as clinical manifestations and methods of management.
There are a few similarities between the two:
- Dysregulation of the Immune System:
- Both kinds of disorders stem from an ineffective immune system. In autoimmune disorders, the immune system erroneously attacks the body’s tissues, when it is afflicted by immune deficiencies the immune system is unable to protect the body against infections.
- Genetic Predisposition:
- All autoimmune diseases as well as some primary immune deficiencies are genetic elements. Some people inherit genes that make them more susceptible to developing these diseases.
- Symptoms Overlap:
- Signs of joint pain, fatigue, and susceptibility to infections may be seen in both autoimmune disorders and immune deficiencies.
- Increased Risk of Infections:
- Although immune deficiencies typically manifest as an increased vulnerability to infection, a variety of auto-immune diseases can also lead to an increased susceptibility to infection, whether as a result of the disease or as a consequence of treatment for immunosuppression.
- Complex Diagnosis:
- Both autoimmune disorders and immune deficiencies are difficult to identify due to their diverse and sometimes overlapping symptoms.
- Immunosuppressive Therapies:
- There are many treatments for autoimmune disorders such as corticosteroids or immunomodulatory drugs, which can suppress your immune system. In contrast, even though these medications help treat autoimmune conditions, however, they can also cause an immune deficiency, which makes the patients more prone to infection.
- Regular Monitoring Required:
- Patients suffering from either autoimmune disorders or immune deficiencies usually require regular medical checks to check for disease progression treatments, as well as possible complications.
- Environmental Triggers:
- All autoimmune diseases as well as some immune deficiencies can be caused or worsened by environmental triggers like stress, infections, and exposure to chemicals.
- Overlap in Conditions:
- As mentioned previously it’s possible, although uncommon, for a person to suffer from both an autoimmune illness and an immune deficiency that blurs the distinction between these two types of diseases.
- Need for Multidisciplinary Care:
- Treatment of both autoimmune diseases and immune deficiencies typically requires a team of experts that includes immunologists, rheumatologists, as well as infectious disease specialists, and others.
Despite these commonalities it’s important to differentiate between autoimmune disorders and immune deficiencies in relation to their causes, the specific signs and symptoms, as well as therapeutic strategies. Understanding the commonalities will aid in providing comprehensive care to patients and aid in the development of new therapeutic approaches.
Conclusion
Both autoimmune diseases and deficiencies are signs of an unregulated immune system. While they arise from different imbalances–autoimmunity from an overactive response against the body’s own tissues and immune deficiencies from an underperforming defense mechanism–they share commonalities in genetic predispositions, symptoms, and certain treatment approaches.
Understanding these similarities can help inform the treatment of patients however it is essential to recognize the difference between them for an accurate diagnosis and appropriate treatment. As our knowledge about the immunity system grows we’re hoping to create more effective and refined treatments for these difficult conditions.