Cellulitis and Filariasis are medical conditions that affect the skin and other tissues. Cellulitis is a bacteria-related disease that causes warmth, redness, and swelling. Filariasis is a result of parasitic worms that are transmitted via mosquito bites, resulting in serious lymphatic damage.
Although it is possible to experience skin swelling, the reasons for treatments, as well as their geographical frequency differ greatly. Understanding the difference between these two conditions is vital for a precise diagnosis and effective treatment.
What is Cellulitis?
Cellulitis is an acute and widespread bacterial infection of the skin and tissues directly beneath the skin. It manifests as swelling, red areas of skin that are tender and hot to the skin. The most commonly cited causes are the bacteria Staphylococcus aureus and Streptococcus pyogenes.
Cellulitis can manifest everywhere on the body but it’s most common to see it in the lower legs. If not treated the condition can be spread to lymph nodes and bloodstream, possibly becoming life-threatening.

What is Filariasis?
Filariasis is an infectious illness caused by nematode worms that resemble threads of the family Filariidae. These worms reside in the lymphatic system, and in some instances, the subcutaneous tissues in humans.
Infections to humans are mainly caused by the bites of mosquitoes that are infected the filariasis virus can trigger various symptoms. The most well-known of these is lymphedema. This occurs when the muscles and organs swell up significantly.
Patients can suffer from elephantiasis, which is a condition that is characterized by severe swelling and thickening of tissues and skin, and hydrocele which refers to an increase in the size of the scrotum. The condition is most found in subtropical and tropical regions across the globe.

Comparison Table of Cellulitis and Filariasis
Certainly! Here’s a comparison table detailing the differences between Cellulitis and Filariasis:
| Aspect | Cellulitis | Filariasis |
|---|---|---|
| Definition | An acute bacterial infection of the skin and underlying tissues. | A parasitic disease caused by nematode worms that affect the lymphatic system and subcutaneous tissues. |
| Causes | Commonly caused by bacteria: Staphylococcus aureus and Streptococcus pyogenes. | Caused by nematode worms: Wuchereria bancrofti, Brugia malayi, and Brugia timori. |
| Transmission | Through breaks or cracks in the skin. | Through the bite of infected mosquitoes. |
| Main Symptoms | Redness, warmth, swelling, pain or tenderness, fever (in some cases). | Lymphedema, hydrocele, fever, lymphangitis, and elephantiasis in chronic cases. |
| Commonly Affected Area | Lower legs, but can occur anywhere on the body. | Limbs, genitals, and other body parts depending on the worm species. |
| Geographical Distribution | Worldwide, not limited by geography. | Tropical and subtropical regions. |
| Treatment | Antibiotics (oral or intravenous). | Anti-parasitic drugs: Diethylcarbamazine (DEC), Albendazole, Ivermectin; lymphedema management. |
| Potential Complications | Abscess formation, sepsis, recurrent infections. | Severe lymphedema (elephantiasis), hydrocele, secondary bacterial infections, renal disease. |
| Prevention | Proper wound care, and skin protection. | Mosquito control, mass drug administration in endemic areas, use of mosquito nets and repellents. |
This table offers a concise comparison between the two conditions.
Prevalent in tropical and subtropical regions
A variety of diseases are common in subtropical and tropical regions due to a variety of elements like a warm climate, a lot of rain, and specific ecosystems that promote the development and reproduction of specific pathogens and vectors.
Here are a few diseases and conditions that are prevalent in these areas:
- Malaria: It is caused through the Plasmodium parasite, and transmitted through the female Anopheles mosquito. It’s among the most well-known illnesses in tropical regions.
- Dengue Fever: A virus that is that is transmitted by the mosquito Aedes. It can cause flu-like symptoms and sometimes can develop into severe dengue that can be fatal.
- Filariasis: As we have previously explained the parasitic illness is caused by nematode-infected worms spread through mosquito bites causing damage to the lymphatic system.
- Yellow Fever: A viral illness that is also transmitted by the mosquito Aedes that causes symptoms ranging from severe fever to liver disease.
- Chagas Disease: It is caused by the Trypanosoma cruzi parasite, it’s passed on to humans via blood-sucking bugs referred to in the field as “kissing bugs” or triatomine bugs.
- Leishmaniasis: Caused by protozoan parasites from the Genus Leishmania and transmitted through the bite of sandflies infected.
- Schistosomiasis (Bilharzia): A parasitic illness caused by trematode flatworms belonging to the Schistosoma family. It is transmitted when people come into contact with fresh water that has been contaminated by the parasites.
- Sleeping Sickness (African Trypanosomiasis): The protozoa that cause it is the species Trypanosoma brucei, and transmitted by the Tsetse fly.
- Chikungunya: A viral disease that is transmitted by mosquitoes Aedes and causes joint discomfort and fever.
- Zika Viral: Another infection caused by Aedes mosquitoes. This is especially important for women who are pregnant as it could create birth defects.
- Ebola disease: While outbreaks can be sporadic, however, it’s a very serious hemorrhagic virus with an extremely high mortality rate most often located within Central as well as West Africa.
- Buruli Ulcer: caused by the Mycobacterium ulcerans bacterium it causes the degeneration of the skin and soft tissue.
They thrive in subtropical and tropical regions because of favorable environmental conditions for the reservoirs, vectors as well and pathogens. Public health interventions that are effective such as the use of sanitation facilities, vector controls, and vaccination (where there is one) are essential in preventing and controlling these illnesses.
Specific countries and areas known for endemicity
The term “endemicity” refers to the continual presence of an infectious disease or agent within a particular geographic region or a population group.
Here’s a list of countries and regions where certain of the mentioned subtropical and tropical diseases are endemic:
- Malaria:
- Sub-Saharan: African countries such as Nigeria, the Democratic Republic of Congo, Mozambique, and Uganda along with Burkina Faso have high transmission.
- Southeast Asia: Regions in India, Myanmar, and Indonesia.
- South America: Amazon basin regions that are located in countries such as Brazil, Peru, and Colombia.
- Certain parts of Central America and the Caribbean.
- Dengue Fever:
- Southeast Asia: Philippines, Thailand, Indonesia, Vietnam.
- The Indian Subcontinent: India, Pakistan, Sri Lanka.
- Central as well as South America: Brazil, Mexico, Colombia, and more.
- The Caribbean.
- Filariasis:
- Sub-Saharan Africa.
- Southeast Asia: India, Indonesia, Philippines.
- Pacific Islands.
- Parts of Central and South America.
- Yellow Fever:
- The tropical regions of Africa are countries in the west and central regions such as Nigeria, the Democratic Republic of Congo, and Uganda.
- The tropical areas in South America: are Brazil, Colombia, Venezuela, and others.
- Chagas Disease:
- Most often, it is found within Latin America: Countries like Bolivia, Argentina, Mexico, and Brazil.
- Leishmaniasis:
- Cutaneous form: Areas that are located in the Middle East, North Africa, and some parts of South America.
- Visceral forms: India, Brazil, Sudan and Ethiopia.
- Schistosomiasis:
- Sub-Saharan Africa, specifically countries such as Nigeria, Tanzania, Ghana and Mozambique.
- Certain regions from Brazil, Yemen, and the Philippines.
- Sleeping Sickness:
- Sub-Saharan African countries, specifically in areas where tsetse fly larvae are common.
- Chikungunya:
- Africa.
- Indian Ocean islands.
- Southeast Asia.
- The Indian Subcontinent.
- Central and South America.
- Zika Virus:
- Brazil and the other South American countries.
- Central America.
- Parts of Southeast Asia.
- The Caribbean.
- Ebola Virus Disease:
- Central as well as West African countries, especially the Democratic Republic of Congo, Guinea, Liberia, and Sierra Leone.
- Buruli Ulcer:
- The majority of them are located in West African countries like Cote d’Ivoire and Ghana.
- There have been reports of cases in Australia.
Be aware that the incidence of the disease can fluctuate in time because of factors like efforts to control vectors and changes in the local ecological conditions, climate changes as well as public health initiatives, and the movement of people.
This is the state of affairs in the last time I updated it in 2022. Therefore, always make sure to check the most current sources such as The World Health Organization or Centers for Disease Control and Prevention to get the most current information.
Ultrasound to visualize adult worms in lymphatics
The use of ultrasound to detect adult worms within the lymphatics is usually used to diagnose filarial diseases, specifically those caused by parasites like Wuchereria bancrofti. This method capitalizes on an unusual phenomenon that occurs in filarial diseases, known in the field of medicine as “filarial dance.”
Here’s an explanation of the way this works:
- Filarial Dance Sign:
- Within lymphatic vessels, adult filarial worms display a distinctive undulating motion, which is aptly referred to”filarial dance. “filarial dance.” The movement is thought to result from the motion of the worms, in conjunction with the flow of lymphatic fluid surrounding them.
- “The “filarial dance sign” is the representation of this dance through ultrasonography.
- Ultrasound Technique:
- A linear transducer with a high frequency (7.5-10 Mhz) is usually used to treat lymphatic vessels that are superficial.
- This “dancing” or wriggling motion of adult worms can be observed in real time using B-mode ultrasonography.
- Advantages of Ultrasound:
- Non-invasive: Ultrasound does not require radiation or other invasive procedures.
- Instant results: The filarial dance is observable in real-time.
- Addition for another test: The test can be utilized in conjunction with the results of blood tests (like the detection of microfilariae during blood smears at night as well as serological testing) to confirm the diagnosis.
- Limitations:
- It requires trained personnel to recognize the filarial dance.
- Might not be as effective in the later phases of the disease, when adult worms may be dead or calcified.
- It may not be accessible in all regions endemic because of infrastructure or economic restrictions.
- Clinical Relevance:
- This technique is especially useful in areas where filariasis has become prevalent, as it allows for quick and clear imaging of adult worms.
- Alongside aiding in diagnosis, ultrasound may also be utilized to evaluate the effectiveness of treatment by observing a reduction in the burden of worms or the cessation of characteristic movement.
Ultrasound can be an effective method of diagnosis in the context of filarial diseases, providing direct evidence of the existence of adult worms within the lymphatic system.
Secondary bacterial infections in swollen limbs
The limbs that are swelling, particularly those caused by conditions such as elephantiasis and lymphedema (as found when filariasis is advanced) are prone to other bacterial diseases.
A weak lymphatic drainage reduces the local immune system and makes the limbs that are swollen more prone to infection. The infections that cause them can intensify the swelling, create further complications, and dramatically affect the health of the patient.
Here’s a brief overview of secondary infections with bacterial causes in swelling limbs:
- Cellulitis:
- Definition: as previously explained as a chronic bacteria-infected infection that spreads to the skin and tissues that lie beneath it.
- Signs: The symptoms include warmth, redness swelling, pain, the sensation of tenderness, fever, and occasionally chills.
- Causative Organisms: Most commonly Staphylococcus aureus and Streptococcus pyogenes.
- Lymphangitis:
- Definition: The inflammation of the lymphatic canals that results from an infection that occurs at a point that is distal to the channel.
- Signs and symptoms: are red streaks that extend from the original lesion or injury, which is often associated with pain, swelling as well as chills, fever, and fever.
- Causative Organisms: The most common is Streptococcus pyogenes.
- Abscess Formation:
- Definition: A small pouch of pus that develops inside organs, tissues, or in the body’s spaces.
- Symptoms: The symptom is a swelling, pus-filled, and painful area of the skin or under it. It may be accompanied by fever.
- Causative Organisms: Mainly Staphylococcus aureus, including Methicillin-resistant Staphylococcus aureus (MRSA).
- Folliculitis:
- Definition: Inflammation or infection of hair follicles.
- Symptoms: The symptoms are small pus-filled blisters or red bumps around hair follicles. Usually caused by burning or itching.
- Causative Organisms: Most often Staphylococcus aureus.
Risk Factors:
- Stable Lymph: Affected the flow of lymph in lymphedematous legs can create an environment favorable to proliferating bacterial growth.
- Skin changes: conditions like elephantiasis can cause skin to become thicker, more cracked, and dry, which makes it more prone to breakage and infections that follow.
- Reduction in Immune Response: Affected lymphatic function indicates that fewer immune cells are present in the affected area to fight off infection.
Prevention and Management:
- Skin care: Cleansing regularly and moisturizing to stop cracks and dryness, and immediate attention to cuts or insect bites could assist in preventing infections.
- Compression: Wearing compression clothing will help decrease symptoms of lymphedema, as well as the chance of contracting infections.
- Antibiotics: Treatment with antibiotics promptly is essential in the event of an infection being suspected. In the case of recurring cases, the use of prophylactic antibiotics could be recommended.
- Educational for Patients: Patients must be taught about the warning signs of illness and the need for immediate medical treatment.
Secondary infections caused by bacteria can increase symptoms of lymphedema, and cause severe discomfort and other complications. Rapid diagnosis and treatment are crucial, along with ongoing treatment to minimize the risk of repeated infections.
Similarities Between Cellulitis and Filariasis
Although filariasis and cellulitis are distinct conditions that have distinct causes and pathophysiologies They do have some similarities, especially in terms of the symptoms and the complications they may cause.
These are the commonalities between them:
- Affected Area:
- Both of these conditions can significantly affect the limbs, especially the legs.
- Swelling:
- Both filariasis and cellulitis can cause swelling or edema in the affected areas. Cellulitis causes swelling and edema caused by inflammation and infection and in filariasis, it’s usually due to lymphatic obstruction.
- Skin Changes:
- Both of them can alter the appearance of your skin. Cellulitis can cause hot, red, and tender skin, and the chronic form of filariasis (elephantiasis) can result in an increase in rough, thick, or bumpy skin. Both conditions make the skin more prone to infections that can cause secondary damage.
- Fever:
- The symptoms of systemic illness like chills, fever, and malaise may be present in both conditions.
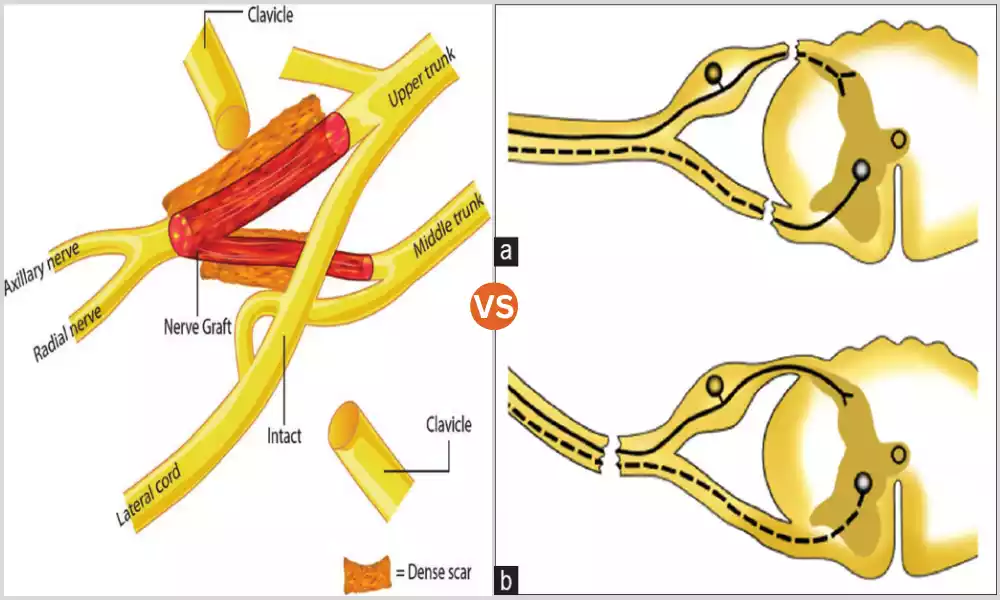
- Lymphatic System Involvement:
- Cellulitis is a bacterial inflammatory condition of the skin and subcutaneous tissues it can also cause lymphangitis (inflammation of the lymphatic canals). The condition, called filariasis, in contrast directly impacts the lymphatic system through having adult worms which can cause obstruction.
- Potential for Recurrence:
- Both of them are likely to develop into a recurring condition. Cellulitis-related episodes that are repeated can happen in particular cases where predisposing causes aren’t taken care of. In filariasis, even after treatment, lymphedema can persist, and individuals remain at risk for acute episodes of dermatolymphangioadenitis (ADLA).
- Secondary Bacterial Infections:
- Limbs that are affected by lymphedema that results from filariasis are susceptible to secondary infections with bacteria such as cellulitis. Thus, a patient with lymphedema caused by filariasis can develop cellulitis on the limb swelling.
- Management Involves Skin Care:
- A good skincare routine is crucial for the treatment of both of these conditions. In the case of cellulitis, it can help in resolving the issue and preventing repeat incidences. When filariasis is present, it’s essential to control lymphedema and avoid secondary infections.
- Complications:
- If not managed properly In the absence of proper management, both conditions may cause grave complications. Cellulitis can cause sepsis, and filariasis may cause elephantiasis as well as extreme disabilities.
It’s important to keep in mind that, even though they have a lot in common, however, they have distinct causes, root mechanisms, and treatments. A proper diagnosis is essential to ensure proper management and treatment.
References books
Here are some reference books that discuss cellulitis, filariasis, and related topics in depth:
- Cellulitis and Related Topics:
- “Fitzpatrick’s Dermatology in General Medicine” by Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, and David J. Leffell. This comprehensive dermatology textbook covers a wide range of skin conditions, including cellulitis.
- Filariasis:
- “Manson’s Tropical Diseases” by Jeremy Farrar, Peter Hotez, Thomas Junghanss, Gagandeep Kang, David Lalloo, and Nicholas White. This is a cornerstone textbook for tropical medicine and covers filariasis in detail.
- “Clinical Parasitology: A Practical Approach” by Elizabeth Zeibig. This book offers a detailed look at various parasitic diseases, including filariasis.
- Lymphatic System and Related Disorders:
- “The Lymphatic System: An Overview” by Amanda M. Prowse and Stanley G. Rockson. This provides a broad overview of the lymphatic system, its function, and related disorders.
- “Lymphedema: Presentation, Diagnosis, and Treatment” by Byung-Boong Lee, John L. Semple, and Stanley G. Rockson. This book delves into lymphedema, a common consequence of filariasis.
- Infectious Diseases:
- “Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases” by John E. Bennett, Raphael Dolin, and Martin J. Blaser. This is one of the most comprehensive textbooks on infectious diseases and covers both bacterial skin infections like cellulitis and parasitic diseases like filariasis.
- Parasitology:
- “Foundations of Parasitology” by Larry S. Roberts and John Janovy Jr. A detailed textbook covering a wide variety of parasitic infections, including filariasis.
Conclusion
It is evident that both diseases, despite having distinct causes, may manifest the same clinical signs, especially when considering the involvement of the limbs. Cellulitis is a bacterial infection and filariasis is a parasitic illness both have an impact on the skin and other tissues, causing swelling, possible secondary infections as well as other complications if they are not properly treated.
Their similarity highlights the importance of having a correct diagnosis since the treatments and long-term consequences differ. The success of treatment depends on a thorough knowledge of the condition and timely medical intervention and preventive actions.