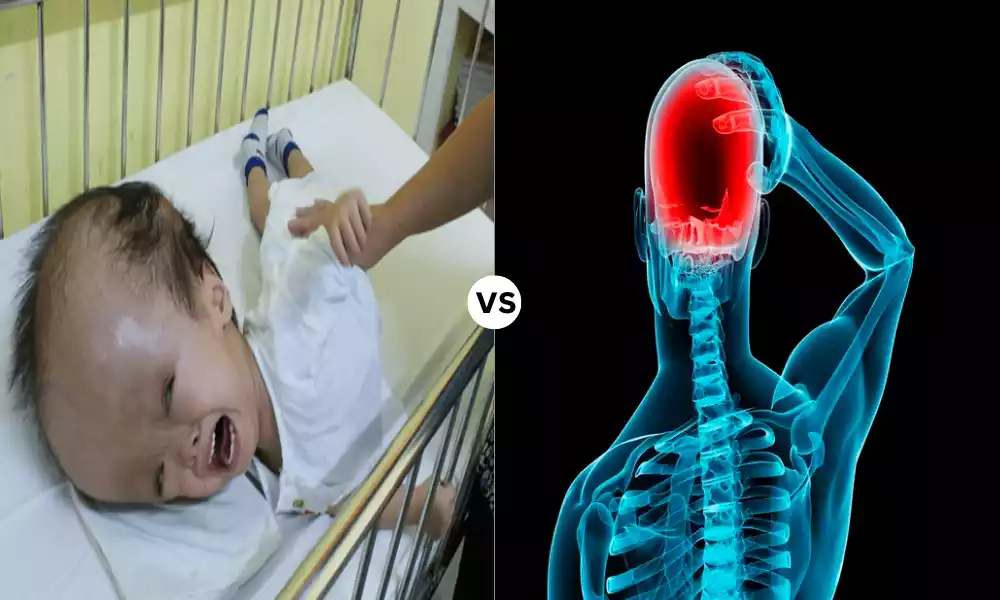
“Hydrocephalus and Pseudotumor Cerebri (Idiopathic Intracranial Hypertension) are two neurological conditions that involve elevated intracranial pressure, often causing symptoms such as severe headaches and visual disturbances.
Despite some similarities in clinical presentation, these conditions differ significantly in their underlying causes, diagnosis, and treatment approaches. This brief guide explores the key distinctions between Hydrocephalus and Pseudotumor Cerebri, shedding light on the importance of accurate differentiation for effective medical management.”
What is Hydrocephalus?
Hydrocephalus is an illness caused by an excessive concentration of cerebrospinal fluid (CSF) in the brain cavity (ventricles) within the brain. The excessive fluid buildup could cause pressure to the brain, leading to neurological signs and complications.
Hydrocephalus can develop at any age and can be the result of various causes, such as congenital malformations, infections tumors, or blockages of or blocking of CSF flow pathways.
The condition usually requires medical treatment to control the overflowing fluid and ease the symptoms associated with it. These could include nausea, headaches vomiting, headaches, and, in the most severe cases, motor and cognitive impairments.
Treatment options for hydrocephalus usually require surgical procedures to divert the drain or regulate the cerebrospinal fluid flow to keep the pressure in the intracranial area at a normal level and avoid further damage to the brain.

What is Pseudotumor Cerebri?
Pseudotumor Cerebri, also referred to as idiopathic intracranial Hypertension (IIH) is a medical condition that is defined by a rise in cerebral pressure (pressure within the skull) that resembles the symptoms of a brain tumor even though there isn’t an actual tumor.
The phrase “pseudotumor” means “false tumor,” because the disease has similar symptoms and features as those experienced by patients suffering from brain tumors, including intense headaches visual impairments, and nausea.
The most important characteristics of pseudotumor cerebri include an increase in cerebrospinal fluid (CSF) pressure, even in the absence of a structural brain defect or tumor.
The precise reason for the pseudotumor cerebri is generally unidentified (idiopathic) however, the theory is that it could be connected with factors such as overweight and hormonal changes, certain medications, and other medical conditions.
Pseudotumor Cerebri can cause various signs and symptoms, such as extreme headaches and visual impairments (such as double or blurred vision) as well as pulseless hearing loss (ringing in the ear which coincides with heartbeat) and, in a few instances, vomiting and nausea. If it is not treated the condition can cause the optic nerve to be damaged and cause vision loss.
The diagnosis of pseudotumor cerebral typically involves a medical examination as well as examinations using imaging (like MRI or CT scans) as well as a puncture in the lumbar region (spinal tap) to determine CSF pressure. Treatment options could include weight management, medication to lower CSF production or decrease the pressure in the intracranial area as well as in some instances surgery to relieve pressure or eliminate excess CSF.
It is important to remember that pseudotumor cerebri can be a serious disease that requires prompt medical examination and treatment to avoid complications and to preserve vision.

Importance of Differentiating Between Hydrocephalus and Pseudotumor Cerebri
The distinction between pseudotumor and hydrocephalus cerebri (idiopathic intracranial hypertension) is vital within the fields of neurology as well as neurosurgery.
There are a number of reasons why it is important to differentiate from these conditions:
- The Divergent Causes: Hydrocephalus is caused by an unnatural accumulation of cerebrospinal liquid (CSF) usually due to structural or blockages within the CSF circulation system. Contrarily there is a pseudotumor cerebri that causes an increase in intracranial pressure but there is no identifiable obstruction or structural defect. A precise distinction is vital because the underlying causes and, therefore the treatment strategies for these conditions differ.
- Therapies: Hydrocephalus typically necessitates surgery to remove excess CSF and relieve pressure in the intracranial area. It could involve the installation of a shunt, or different surgical treatments. In the case of pseudotumor cerebri, treatment options begin with medications to decrease intracranial pressure or control contributing factors like obesity. Surgical procedures for pseudotumor cerebri are usually reserved for patients who are not responding to medical treatment. A precise diagnosis is essential for guiding the appropriate treatment choices.
- Prognosis and outcomes: The long-term outcomes and prognoses for hydrocephalus as well as pseudotumor cerebri are different. If left untreated, hydrocephalus can cause serious neurological problems and complications, such as motor and cognitive impairments.
pseudotumor cerebri tends to be less likely than other types of neurodegeneration but could result in loss of vision when left untreated. A timely diagnosis and treatment can assist in preventing or minimizing these consequences. - Health Resource Allocation: A clear distinction between these conditions will ensure that healthcare resources are appropriately allocated. Inappropriate hospitalizations and procedures are avoided if the proper diagnosis is determined at an early stage of the evaluation process.
- Patient Well-being: A precise diagnosis can reduce patient anxiety and ambiguity. Family members and patients frequently encounter difficult situations when they have to deal with symptoms of neurological. Knowing the exact diagnosis and treatment plan gives the patient clarity and confidence.
- Studies as well as Advancements: Distinguishing between pseudotumor cerebri and hydrocephalus is crucial to advance medical research and enhance the treatment options for both. An accurate diagnosis can help identify those who need clinical trials or studies, which ultimately leads to better outcomes and treatments.
The distinction between pseudotumor cerebri and hydrocephalus is vital to ensure effective treatment of patients, individualized treatment plans, more accurate prognoses, and advancement of knowledge and treatment for neurology as well as neurosurgery. It allows healthcare professionals to focus on the specific aspects of each disease and maximize the outcomes for patients.
Comparison Table of Hydrocephalus and Pseudotumor
Here’s a comparison table highlighting the key differences and some similarities between Hydrocephalus and Pseudotumor Cerebri (Idiopathic Intracranial Hypertension):
| Characteristic | Hydrocephalus | Pseudotumor Cerebri |
|---|---|---|
| Definition | Accumulation of CSF in brain ventricles, causing increased intracranial pressure. | Elevated intracranial pressure without a structural brain abnormality. |
| Underlying Causes | Structural abnormalities, blockages in CSF circulation, infections, tumors. | Often idiopathic (unknown cause); linked to obesity, medications, and hormonal changes. |
| Age of Onset | Can occur at any age, including infants (congenital) and adults (acquired). | Typically affects adults, especially overweight women of childbearing age. |
| Symptoms | Varies based on age and cause but may include headache, nausea, vomiting, and cognitive and motor deficits. | Severe headaches, visual disturbances (blurred or double vision), pulsatile tinnitus, nausea. |
| Diagnostic Tools | Imaging studies (MRI, CT scans), clinical evaluation, lumbar puncture (measuring CSF pressure). | Imaging studies, clinical evaluation, lumbar puncture (measuring CSF pressure). |
| Treatment Options | Surgical intervention (shunt placement, endoscopic third ventriculostomy) to drain excess CSF. | Medications (acetazolamide), weight management, and, if needed, surgical intervention (CSF shunt, optic nerve sheath fenestration). |
| Prognosis | Varied, depending on the cause, age, and promptness of treatment. | Generally good, with vision loss being the most serious complication if untreated. |
| Potential Complications | Cognitive and motor impairments, developmental issues in children. | Vision loss (papilledema), but often reversible with prompt treatment. |
| Ongoing Monitoring | Requires ongoing monitoring and adjustments, especially for shunt maintenance. | Regular follow-ups for medication adjustments and monitoring of symptoms. |
| Research and Advancements | Ongoing research into shunt technology and alternative treatments. | Research focuses on identifying underlying causes and improving medical management. |
This comparison table highlights the main differences in terms of definition, causes, age of onset, symptoms, diagnosis, treatment, prognosis, and ongoing care between hydrocephalus and pseudotumor cerebri. While they both involve increased intracranial pressure, their causes and treatment approaches are distinct.
What are the similarities between hydrocephalus and pseudotumor cerebri?
The pseudotumor cerebri and hydrocephalus (idiopathic intracranial hypertension) share some similarities, despite their major differences.
Here are the most significant similarities between the two conditions:
- Increased Intracranial Pressure (ICP): Both conditions result in elevated pressure inside the skull due to an increase in cerebrospinal fluid (CSF) as well as an increased blood intracranial volume. The pressure increase can cause similar symptoms in both of the conditions.
- Neurological Symptoms: Pseudotumor cerebri and Hydrocephalus may cause similar neurological symptoms, which include severe headaches, visual impairments (such as double or blurred vision), and nausea. These symptoms are often caused by the pressure put on the brain’s structures.
- Potentially Associated Complications If untreated or untreated the two conditions could cause grave complications. In the case of hydrocephalus, this can be accompanied by motor and cognitive impairments, primarily for children and infants. In pseudotumor cerebri vision loss caused by an edema (swelling on the nerve’s optic head) may be the main serious possible complications.
- A requirement for ongoing monitoring: Patients with both pseudotumor cerebri and hydrocephalus generally require continuous surveillance to evaluate the progress of their condition and modify treatment if needed. Monitoring can involve clinical assessments as well as imaging studies and for those suffering from pseudotumor cerebri, periodic tests of the visual system.
- Response to treatment: Both of the conditions respond positively to treatment. Hydrocephalus can be treated with the placement of shunts and other procedures that drain excess CSF and pseudotumor cerebri is treated by taking medications to decrease the pressure inside the skull, as well as weight management and in some instances surgical procedures.
- Importance of a timely diagnosis: Early diagnosis and treatment are crucial for preventing or minimizing the risk of complications, and enhancing the overall outcome.
Although these are all very similar however, it is important to understand that pseudotumor cerebri and hydrocephalus have different causes, ages of diagnosis, and treatment strategies. So, an accurate distinction between the two is vital to ensure proper treatment and improved outcomes for patients.
Symptoms and Clinical Presentation
The symptoms and clinical manifestations associated with Hydrocephalus as well as Pseudotumor Cerebri (Idiopathic Intracranial Hypertension) might overlap, but there are distinct differences because of the distinct reasons for these disorders.
These are the typical symptoms and clinical signs for each condition:
Hydrocephalus Symptoms and Clinical Presentation:
- Headaches: Sometimes described as continuous and severe the headaches may worsen in the morning, or while sitting down because of increased intracranial pressure.
- Nausea and vomiting: Nausea and vomiting particularly in the morning, may be caused by headaches.
- Vision Disturbances: Hydroxycephalus could cause vision issues, including double or blurred vision, difficulty in focusing or changes in the visual clarity.
- Mental and motor changes Based on the patient’s age as well as the seriousness of their problem hydrocephalus could cause problems with memory, cognitive decline problems, and motor problems like gait problems and lack of coordination.
- Incontinence: Hydrocephalus could cause urinary and fecal incontinence.
- A swelling in the Fontanelle (in infants): In infants with congenital hydrocephalus small soft spot on the baby’s head (fontanelle) can swell or become tight.
- Papilledema: The optic nerve’s head. This can be observed through an eye exam.
Pseudotumor Cerebri Symptoms and Clinical Presentation:
- Headaches: As with hydrocephalus the pseudotumor cerebri can cause severe headaches. They are typically described as throbbing. It can be worse in the morning, or while lying down.
- Visual disturbances: Visual symptoms are typical and could include blurred vision and the phenomenon of double vision (diplopia) or temporary visual obscurements (temporary visual loss) and Pulsatile Tinnitus (ringing in the ear that is that is synchronized with heartbeat).
- Vomiting and Nausea: Similar to hydrocephalus Pseudotumor cerebri can cause vomiting and nausea.
- Temporary Visual Loss: Patients might have brief periods of loss of vision, usually caused by body posture changes.
- Papilledema: The swelling of the optic nerve’s head caused by an increase in intracranial pressure is a characteristic of pseudotumor cerebri. It’s usually detected in an examination of the eyes.
- Neck and back pain: People with pseudotumor cerebri might be suffering from back and neck pain.
It’s crucial to recognize that, while the symptoms are similar in both of the conditions, the root reasons and treatment methods differ. In addition the intensity and severity of symptoms may differ between patients.
An immediate medical evaluation as well as diagnosis from a medical specialist, which may include Ophthalmological and neurological tests are essential to determine the condition that is causing it and establish the proper treatment.
Prognosis and Long-term Management
The long-term prognosis and treatment for Hydrocephalus, as well as Pseudotumor Cerebri (Idiopathic Intracranial Hypertension), vary based on a variety of aspects, such as the root causes as well as its severity problem at the time of diagnosis, as well as the efficacy of treatment.
Here’s a brief overview of the prognosis as well as long-term treatment for each of the conditions:
Hydrocephalus:
Prognosis:
- The prognosis for patients with hydrocephalus can differ greatly. It’s based on variables like the patient’s age the reason for hydrocephalus the time it took to be diagnosed, and the efficacy of treatment.
- In the case of congenital hydrocephalus (present at birth), It is important to diagnose the condition early and treatment that is appropriate, typically with shunt placement and other procedures could result in better outcomes.
- In cases of acquired hydrocephalus, the prognosis is based on the root causes. If the root cause is effectively removed or treated (e.g. removal of tumors or treatment for infection) the prognosis could be good.
Long-term Management:
- The long-term treatment of hydrocephalus usually requires ongoing monitoring and possible changes to treatment.
- Shunts, that divert the excess cerebrospinal fluid (CSF) out of the brain need regular periodic check-ups to make sure they’re working properly. Shunt malfunctions are not unusual.
- Certain people may have complications or require shunt revisions in time.
- Children suffering from hydrocephalus might require assistance with their development and education as they develop and are faced with the possibility of motor and cognitive difficulties.
Pseudotumor Cerebri:
Prognosis:
- The outlook for patients with pseudotumor cerebri is usually positive when the disease is treated and diagnosed promptly.
- Vision loss is among the most severe complications resulting from pseudotumor cerebri. However, by taking the appropriate action the condition can be avoided or reversed.
- Pseudotumor Cerebri doesn’t usually cause permanent neurological impairments when it is treated effectively.
Long-term Management:
- Long-term treatment for pseudotumor cerebri typically requires regular medical and ophthalmological treatment.
- Acetazolamide is a medication that can be prescribed to decrease the pressure in the intracranial area.
- The management of weight is vital especially in patients who are overweight, since losing weight can lead to improvements in symptoms.
- Regular visits to an eye doctor are required to check for papilledema and assess the changes to vision.
- In certain situations surgery, like the fenestration of the optic nerve may be considered in cases where medical treatment is not sufficient.
The long-term treatment is focused on ensuring that symptoms are controlled as well as preventing any complications and improving the patient’s health. Regular follow-up visits with health professionals are necessary to evaluate the progression of the illness and make any adjustments to the treatment regimen.
Patients and their family members should be informed about the warning indicators of potential issues and the importance of following the guidelines for managing the condition.
Patient Cases Illustrating Pseudotumor Cerebri
Here are two possible cases of patients suffering from an idiopathic cerebri (idiopathic intracranial hypertension) to give a comprehension of the way this disorder can impact patients:
Patient Case 1: Jane’s Journey
Jane is a woman aged 28 who has suffered from obesity for the majority years. In the last few months, she’s suffered from increasingly severe headaches, mainly in the morning and while lying down. The headaches are usually followed by vomiting and nausea. Jane has noticed that her vision is becoming blurred, and sometimes she has double vision. Inquired about her condition Jane decides to speak with her primary healthcare doctor.
After examining Jane’s eyes, the doctor detects papilledema in an eye examination, and the head of the optic nerve is swollen. An MRI, as well as a lumbar puncture, are used in order to establish the presence of a pseudotumor cerebri. A lumbar puncture can reveal elevated cerebrospinal liquid (CSF) tension.
Treatment and Long-Term Management:
- Jane’s healthcare team prescribes acetazolamide medication that decreases CSF production and assists in lowering the pressure in the intracranial area.
- Jane is being referred to a neurologist and an eye doctor for continuous surveillance and management.
- It is recommended that she lose weight by combining diet and exercise in order to reduce pressure in the intracranial area.
- Regular check-ups with her healthcare specialists are scheduled to keep track of her condition and alter her treatment plan if needed.
- With consistent medical treatment and weight loss strategies, Jane’s symptoms begin to improve. Her vision is clearer and her headaches are less frequent and a bit more intense.
Patient Case 2: Mark’s Challenge
Mark is a man aged 42 who is active and eats well. But, he starts to notice strange symptoms. He experiences intense and throbbing headaches, which tend to be most severe during the early morning hours.
The headaches are often accompanied by pulsatile tinnitus. there is a pulsating hearing ringing within his ears that is to match the beat of his heart. At times, he may experience intermittent visual obscurations that cause his vision to fade.
Inquired about his symptoms Mark plans appointments with an optometrist. During the exam, the doctor observes the presence of papilledema. This prompts further examination. An MRI and puncture of the lumbar area verify the presence of pseudotumor cerebri.
Treatment and Long-Term Management:
- Mark’s neurologists and ophthalmologists suggest acetazolamide for reducing intracranial pressure.
- He should maintain his weight and healthy lifestyle since obesity isn’t a factor that contributes to his situation.
- Eye exams are regularly scheduled to check the condition of papilledema and to evaluate any changes to his vision.
- Mark discovers how to control his illness effectively through lifestyle changes and medication.
- With time the symptoms get more frequent, and also less severe and he is able to see without significant issues.
These patient cases show how pseudotumor cerebri may affect people from different backgrounds and ages. Early diagnosis, proper treatment, and lifestyle adjustments can result in positive outcomes and a better standard of living for people affected by this disease.
Regular monitoring is vital to control symptoms and avoid problems such as vision loss.
Reference Books
Here are some reference books related to neurology, neurosurgery, and the conditions discussed, such as Hydrocephalus and Pseudotumor Cerebri. Please note that my knowledge is based on information available up to September 2021, so there may be newer publications available as well.
- “Principles of Neurological Surgery” by Richard G. Ellenbogen, Saleem I. Abdulrauf, Laligam N. Sekhar
- This comprehensive textbook covers various aspects of neurological surgery, including the management of conditions like hydrocephalus.
- “Pediatric Hydrocephalus” edited by Giuseppe Cinalli, Concezio Di Rocco, James M. Drake
- This book provides insights into the diagnosis and management of hydrocephalus in pediatric patients.
- “Hydrocephalus: Causes, Management, and Outcomes” edited by Julian T. Hoff
- A comprehensive resource on hydrocephalus, covering its causes, treatment options, and long-term outcomes.
- “Idiopathic Intracranial Hypertension: Understanding and Management” by Susan P. Mollan and Susan M. Downes
- This book focuses on idiopathic intracranial hypertension (pseudotumor cerebri), providing insights into its diagnosis and management.
- “Youmans and Winn Neurological Surgery” edited by H. Richard Winn
- A renowned textbook in the field of neurosurgery, covering a wide range of neurosurgical topics, including hydrocephalus.
Conclusion
Hydrocephalus as well as Pseudotumor Cerebri are two distinct neurological disorders that share common symptoms but differ in root causes, diagnostic methods as well and treatments. Knowing the distinct characteristics of the two conditions is essential for a correct diagnosis and effective treatment, which ultimately leads to enhanced outcomes for patients.
Early intervention, continuous monitoring, and patient education are vital components of the treatment of patients affected by these disorders. Medical research is constantly improving the understanding and treatment of these diseases providing the possibility of better treatment and results in the near future.