Intubation is a crucial medical procedure that requires the introduction of tubes into the airway to ensure proper ventilation and oxygenation. Two main methods to achieve it are rapid Rapid Sequence Intubation and Normal Intubation.
The two methods differ in terms of approach, intent, and method of execution. we will examine the main differences in RSI and normal intubation. It will highlight the instances and reasons why each one is utilized in medical practice.
What is Rapid Sequence Intubation?
Rapid Sequence Intubation (RSI) can be described as a specific medical procedure that is used to protect the airway of a patient quickly and effectively. It involves the quick treatment of specific medications and then the insertion of an endotracheal tube in order to ensure a secure airway.
RSI is generally used in situations where immediate control of the airway is crucial like in critical or emergency medical situations. The primary objectives of RSI are to limit the risk of aspiration make sure that oxygen levels are adequate and provide the best conditions for oxygen or mechanical ventilation distribution to the patient.
What is Normal Intubation?
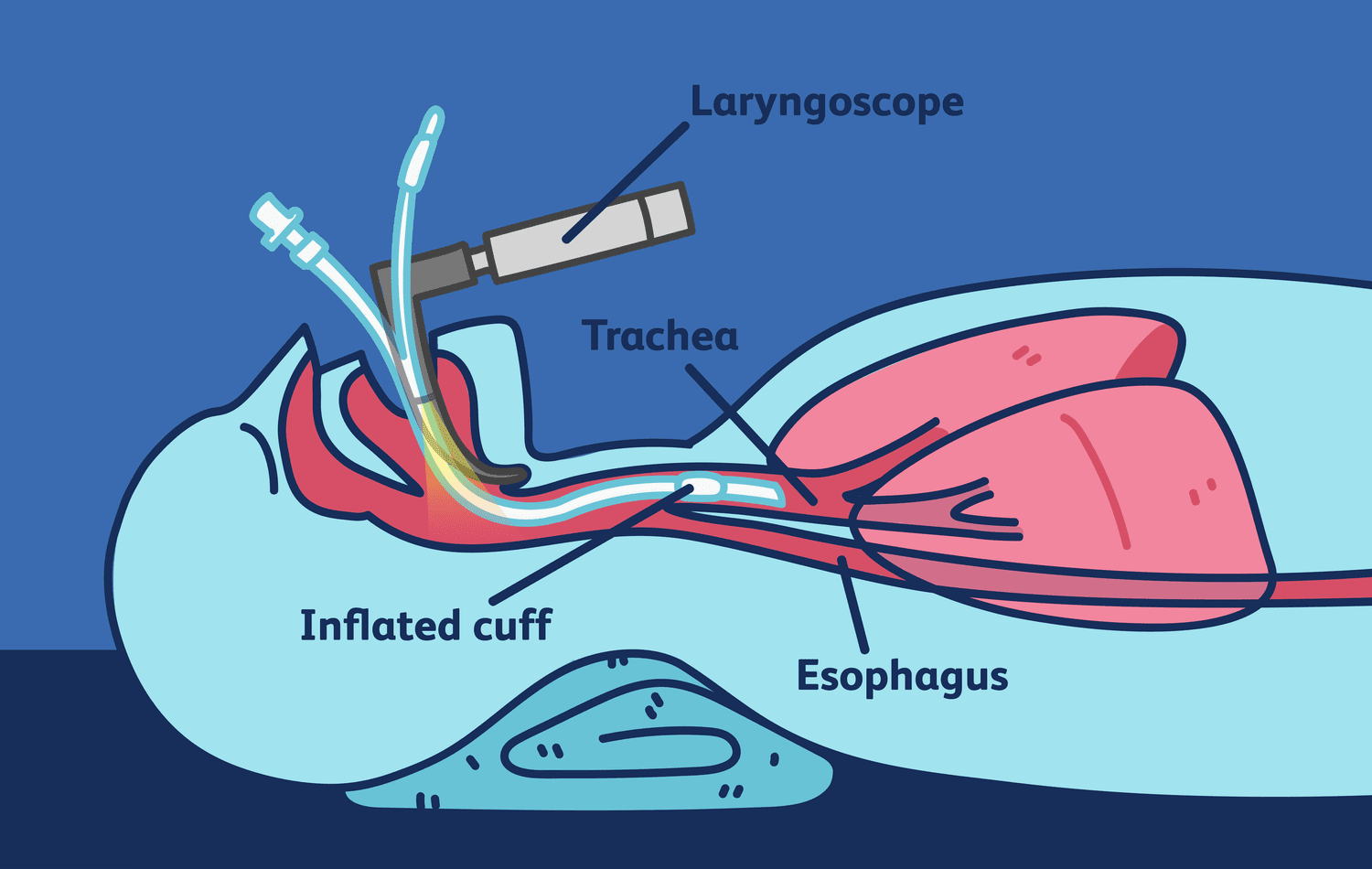
Intubation that is normal, commonly referred to as conventional or elective intubation is a medical procedure intended to create and secure an airway for a patient. It is done by inserting an endotracheal tubing into the trachea via the nose or mouth.
This procedure is generally carried out under specific circumstances like when planned surgery is being performed or in circumstances that are not urgent medical emergencies where the patient’s breathing needs to be taken care of for a prolonged period.
Normal intubation usually is performed after the patient is appropriately treated and sedated to limit discomfort and risk associated with the procedure. It allows for a careful assessment of the preparation and application of the appropriate medication and procedures to ensure effective and safe airway control.

Comparison Table of Rapid Sequence Intubation and Normal Intubation
Here’s a simplified comparison table highlighting the key differences between Rapid Sequence Intubation (RSI) and Normal Intubation:
| Aspect | Rapid Sequence Intubation (RSI) | Normal Intubation |
|---|---|---|
| Purpose | Swift and controlled airway management in emergency situations. | Planned airway management during elective procedures or non-emergencies. |
| Indications | High-risk situations like trauma, respiratory failure, or critical emergencies. | Elective surgeries, diagnostic procedures, or when patient stability allows. |
| Medications | Rapid administration of sedatives and paralytics. | Gradual administration of sedatives and analgesics. |
| Airway Assessment | Often limited due to urgency. | Thorough assessment before intubation. |
| Patient Preparation | Limited or none due to urgency. | Adequate pre-intubation preparation and positioning. |
| Sedation and Analgesia | Typically includes strong sedatives and paralytics. | Uses sedatives and analgesics, but is not as potent as in RSI. |
| Laryngoscopy and Tube Insertion | Rapid and often performed immediately after medication administration. | Laryngoscopy and tube insertion were performed after sedation and positioning. |
| Verification of Tube Placement | Typically follows intubation due to urgency. | Confirmation of tube placement is done after intubation. |
| Risks and Complications | Higher risk of complications, such as hypotension and hypoxia, due to urgency. | Lower risk of complications if proper patient assessment is performed. |
| Suitability | Emergency cases with unstable patients. | Planned procedures with stable patients. |
Note: The choice between RSI and Normal Intubation depends on the clinical scenario, patient condition, and the urgency of airway management, with each approach having its own advantages and risks. Proper training and clinical judgment are essential in making the appropriate choice.
Importance of intubation in medical procedures
Intubation is a vital medical procedure that has a variety of purposes and applications in a variety of medical environments.
Its importance is in its capacity to create a safe and controlled airway that is vital in a variety of surgical procedures and clinical scenarios:
- Respiratory Support: Intubation is typically employed to assist patients suffering from impaired respiratory function, like patients with acute respiratory distress (ARDS) severe respiratory failure, or pneumonia. It helps ensure a clear airway that allows for the transport of oxygen and the removal of carbon dioxide.
- Mechanical Ventilation: Intubation is the prerequisite for mechanical ventilation. It is vital in situations when the patient’s capacity to breathe properly is impaired. It allows healthcare professionals to monitor the patient’s breathing as well as oxygenation and ventilation parameters.
- Anesthesia administration: during surgery or other medical procedures, patients require being under general anesthesia in order to remain conscious and pain-free. Intubation is a method of delivering anesthesia gas directly into the lungs, which allows the precise control of anesthesia depth as well as the safety of the patient’s breathing.
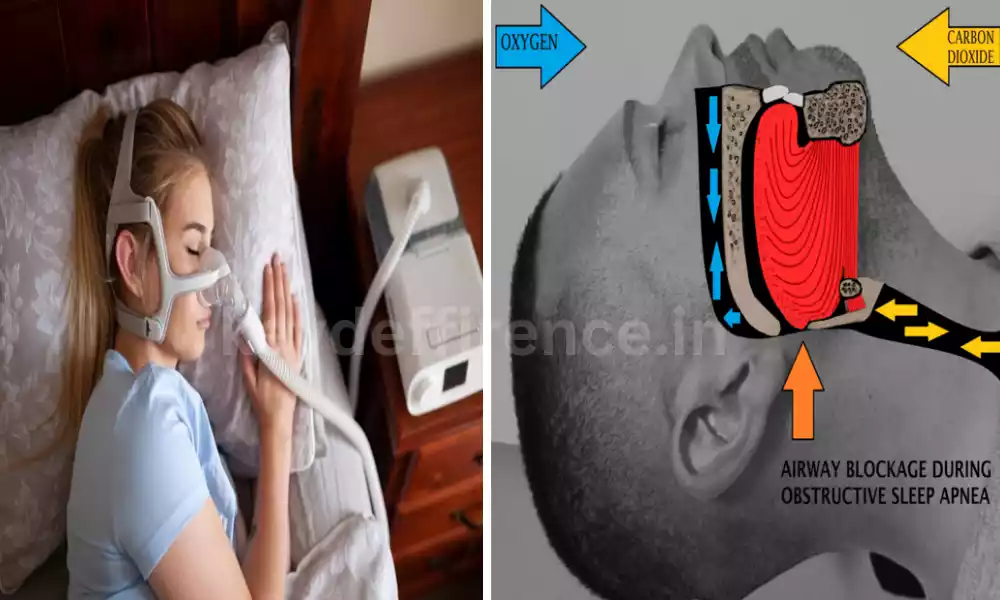
- Airway Protection: Intubation is essential to prevent inhalation aspiration and other substances in the lungs. This could cause severe respiratory problems, such as pneumonia.
- Treatment of the Secretion: Patients who are not able to eliminate respiratory secretions efficiently might require intubation to aid in suctioning and management of secretions and to prevent obstruction to the airways.
- Diagnostic procedures: In certain cases, it is required to intubate the patient to view and access the respiratory tract of lower and upper. This can aid in the diagnosis of procedures such as bronchoscopy. It permits the direct inspection of and collection of samples of the airways.
- Emergencies: In emergency medicine, intubation is typically used to quickly ensure the airway is secured for patients who are suffering from life-threatening ailments like cardiac arrest, or serious allergic reactions. It can be a lifesaving treatment in the most critical of circumstances.
- Security of Airway Reflexes: Intubation can be required to safeguard a person’s airway reflexes, particularly when they are at risk of aspiration because of changes in consciousness or neurological disorders.
- Preventing Hypoxia: Intubation helps ensure the continuous oxygen supply to the lungs of the patient to prevent anoxia (oxygen deficiency) which could result in organ damage or even failure.
- Drug Administration: In certain situations, specific medication, such as naloxone or epinephrine, might be required to be administered directly into the tube for endotracheal intubation to treat life-threatening illnesses promptly.
Intubation is an essential procedure that plays a vital part in the management of airways as well as the delivery of anesthesia, respiratory support, and overall health of patients in different medical environments.
It assists healthcare professionals in ensuring the health of the airway in order to ensure adequate oxygenation and ventilation. It is vital for life-saving procedures and planned medical procedures.
Introduction to Rapid Sequence Intubation (RSI) and Normal Intubation
The management of airways is a crucial element of healthcare. two main methods are employed to safeguard the airway of a patient in various situations The two main methods are Rapid Sequence Intubation (RSI) and normal Intubation.
These methods are crucial in making sure that oxygenation, ventilation, and overall health of patients however, they are used in distinct situations and each one has its own set of rules and protocols.
Rapid Sequence Intubation (RSI):
Rapid Sequence Intubation (SI) is a high-risk procedure, with a time-sensitive nature that is used mostly in critical and emergency care environments. It’s designed to swiftly and effectively protect an airway for a patient when prompt intervention is necessary.
RSI requires a meticulously planned sequence of administration of medications and airway management strategies to reduce the risk of aspiration, guarantee an optimal flow of oxygen, and offer an uncontrolled airway that allows mechanical ventilation. It is commonly utilized in situations like cardiac arrest, trauma or other life-threatening situations where there is a short time frame to make a thorough preparation.
Normal Intubation:
Normal Intubation on the contrary is a more systematic and less pressure-free method of securing the airway. It is generally used for surgical procedures that are not elective as well as situations where the patient is stable, and it’s sufficient time for thorough patient assessment and preparation.
This approach includes administering analgesics and sedatives to ensure patients’ comfort and cooperation a careful positioning of the patient and a slower procedure for inserting the tube to create an airway that is secure.
This allows healthcare professionals to effectively assess and manage the airway, which makes it ideal for interventions planned where patients’ safety is guaranteed.
In this study in this series, we will dig deeper into the fundamental practices, procedures, and crucial distinctions between rapid Sequence Intubation as well as Normal Intubation and will provide a better understanding of the reasons behind each technique and how it is utilized in the complicated world of managing airways. Knowing these methods is crucial for medical professionals to make informed choices and provide optimal treatment for patients in a variety of medical settings.
Risks and complications associated with RSI
Rapid Sequence intubation (RSI) is a high-risk medical procedure that comes with certain dangers and complications, primarily because of the urgency and specific drugs employed. Healthcare professionals should be aware of these possible negative outcomes while performing RSI to limit risk and give the highest quality of care to the patient.
The dangers and complications that can be attributed to RSI are:
- Hypoxia: A main concern during RSI is the possibility that a patient will suffer from the condition known as hypoxia (low oxygen level). The process involves sedating the patient and temporarily disrupting breathing independently. If the process of intubation is not quick and efficient it can result in oxygen saturation, possibly causing organ damage or even organ dysfunction.
- Aspiration: In the course of RSI, people with RSI may have at greater chance of inhaling stomach contents and any other liquids that enter the airway into the lung. This could lead to aspiration pneumonia and other respiratory problems.
- Hypotension: In the course of treatment for RSI specifically paralytics and induction agents could cause an increase in blood pressure. This can be particularly alarming for patients who are hemodynamically unstable.
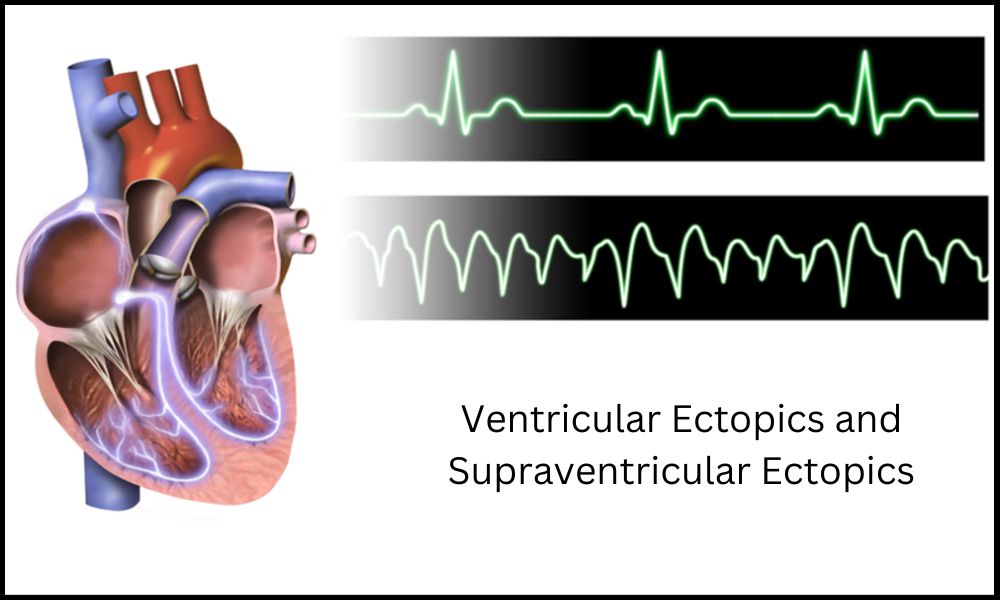
- Cardiac Arrhythmias: Certain induction agents and paralytics can trigger cardiac arrhythmias which could be life-threatening for patients suffering from certain cardiac disorders.
- Bronchospasm: In patients who are at risk, RSI medications can trigger the bronchospasm (narrowing in the airways) that can cause severe respiratory discomfort and the necessity for further treatments.
- Allergic Reactions: Although it is rare allergies to RSI medications are possible and can range from mild rashes or severe anaphylaxis.
- Difficult Intubation: Despite meticulous preparation, intubating certain patients can be difficult. Intubation difficulties can lead to repeated attempts, long times of desaturation, as well as and the risk of airway trauma.
- Trauma to the Oral Structures: The process of laryngoscopy or tube insertion could cause injury to the oral structure like dental damage and lacerations as well as trauma to the mucosa.
- Medication Errors: Dosing errors, administration mistakes, errors or drug interactions may be observed in RSI and could result in adverse reactions.
- Neuromuscular Blockade Reversal: After intubation, reversing the effects of neuromuscular-blocking agents is crucial. Failure to do this can cause prolonged intubation or a lack of ventilation.
- Esophageal Intubation: The incorrect placement of the tube may result in esophageal tube intubation. The tube enters the esophagus in place of the trachea. This results in inadequate ventilation.
- Barotrauma: The overinflation and suffocation of lungs or insufficient ventilation settings could cause barotrauma. leading to pneumothorax and pneumomediastinum.
Healthcare professionals who perform RSI need to be well-trained proficient, skilled, and ready to handle these dangers and complications quickly. The use of preoxygenation, careful assessment of the patient as well as the correct selection of drugs and dose monitoring are vital to taking care of these risks and guaranteeing the safety and effectiveness of the treatment.
Clinical scenarios where RSI is preferred
Rapid Sequence Intubation (RSI) is the preferred method for specific clinical situations when it is imperative to ensure the airway and oxygenation is crucial. RSI is designed to be used in situations in which immediate intervention is needed due to the severity of the patient’s medical condition.
A few clinical scenarios in which RSI is recommended include:
- Trauma patients: RSI is typically the preferred method to intubate severely injured trauma patients, like patients suffering from facial fractures, head injuries, or airways that are damaged from incidents. The goal in these situations is to safeguard the airway and avoid further injuries or complications.
- Cardiac arrest: In the event of cardiac arrest an immediate intubation with RSI might be necessary in order to secure the airway to allow for advanced life support measures, including chest compressions as well as administration of medication.
- Respiratory Failure: Patients who experience severe respiratory problems, be it caused by severe pneumonia acute respiratory distress syndrome (ARDS), or any other reasons, might be required to undergo RSI to ensure adequate ventilation and oxygenation.
- severe anaphylaxis: in cases that are characterized by severe reactions to allergens that result in airway obstruction, RSI may be the fastest method of securing an airway as well as administering lifesaving drugs like epinephrine.
- Nervous Emergencies: Patients suffering from neurological emergencies, like seizures or brain injuries that are traumatic might require RSI to avoid aspiration and to ensure sufficient oxygen levels while addressing the condition that is causing it.
- Obstructed Airway: RSI is commonly used when a patient is suffering from an obstruction caused by a foreign object that is blocking the airway and cannot maintain adequate oxygenation or ventilation.
- Sepsis, or Septic shock: In the case of severe sepsis, or septic shock, where the patient’s mental health changes and airway security is impaired, RSI may be necessary to control airway pressure.
- Overdose or poisoning: When there is a poisoning or drug overdose, RSI can be used to protect the airway and give mechanical ventilation as well as treat the overdose using antidotes.
- Intractable seizures: Patients suffering from prolonged or frequent seizures that don’t respond to the initial treatment might require RSI to control their airways in order to administer intravenous antiepileptic drugs.
- Children Emergencies: RSI is commonly used in pediatric emergencies, like serious respiratory distress (SRS), status epilepticus, or cardiac arrest. the rapid management of airways is vital because of the less room for error among children.
- burns as well as inhalation Injury: In the event of serious burns or inhalation injuries, RSI might be required to safeguard the airway against irritation from chemicals or edema.
- Hemorrhagic shock: Patients who are in hemorrhagic shock might require RSI to protect the airway and help stabilize hemodynamics through controlled airway ventilation.
It is important to remember that even though RSI is a useful method in these situations, it should only be carried out by skilled health professionals who are experienced in managing airways and have the appropriate tools and medications readily accessible.
A thorough assessment of the patient and consideration of specific aspects of the patient’s condition should be the basis for the decision to utilize RSI for each situation.
Similarities Between Rapid Sequence Intubation and Normal Intubation
Rapid Sequence Intubation (RSI) as well as Normal Intubation (NI) are both ways to secure a patient’s airway and have several similarities, such as:
- Airway Establishment: Both RSI and Normal Intubation are methods used to secure the airway through the intubation of an endotracheal tube through the trachea. This allows the passage of oxygen and mechanical ventilation.
- Endotracheal Tube: In both of these procedures an endotracheal tube is used to ensure the integrity of airways. The tube is inserted in or through the oral cavity (oral intubation) or through the nasal passage (nasal intubation) according to the medical situation and preference of the doctor.
- Analgesia and Sedation: Analgesic and sedative medication is administered both in RSI or Normal Intubation, to guarantee patient peace of mind, minimize discomfort, and limit the body’s response to intubation. The dosage and choice of the medications can differ however the concept of providing sedation is a common practice.
- Monitoring: Monitoring continuously important indicators such as blood pressure, heart rate oxygen saturation, as well as CO2 (carbon dioxide) levels, is crucial in both procedures to evaluate the patient’s reaction and adjust treatment accordingly.
- Equipment: similar equipment is utilized for both RSI and normal Intubation which includes laryngoscopes for visualization of the vocal cords, tubes for the endotracheal system of different sizes, and devices to secure the tube in a place like tie strips or adhesive strips.
- Preoxygenation: Both methods generally require preoxygenation for the patient to boost oxygen levels in the lungs prior to the intubation procedure. A proper preoxygenation regimen can keep the patient from becoming hypoxic throughout the process.
- Check Of Tube Placement: after the intubation procedure in the two cases of RSI or Normal Intubation, the location of the endotracheal tube needs to be confirmed to ensure that it is properly placed in the trachea and not the esophagus or the bronchus. This is usually done by auscultation, chest raise, and visualizing CO2 waveforms.
- Risks and Complications: Both procedures come with inherent risks and complications, such as hypoxia aspiration injuries to the airway or the structures surrounding it, as well as adverse reactions related to medication. Healthcare professionals must be on guard and ready to handle these issues.
- Collaboration among Team Members: In Both RSI and Normal Intubation Efficient communication and coordination between the members of the team are essential to ensure the safety and success of the procedure.
- Assessment of the Patient: Before intubation, medical professionals perform a thorough examination of the patient’s airway, medical history, and medical condition to determine the best method of intubation and the appropriate medications.
While there are some similarities however, it is crucial to note that the primary distinctions in RSI as well as Normal Intubation lie in the situations in the clinical setting, urgency, and specific protocols for the procedure. Healthcare professionals should select the most appropriate method depending on the needs of the patient and the context of the patient.
Reference Books
Certainly, here are some reference books across various fields of study and subjects. Please note that my knowledge is current as of September 2021, so there may be more recent publications available. Additionally, the availability of these books may vary by region and time.
Medicine and Healthcare:
- “Harrison’s Principles of Internal Medicine” by Dennis L. Kasper et al.
- “Robbins and Cotran Pathologic Basis of Disease” by Vinay Kumar et al.
- “Current Medical Diagnosis and Treatment” by Maxine A. Papadakis et al.
- “The Washington Manual of Medical Therapeutics” by Pavan Bhat et al.
- “Emergency Medicine: A Comprehensive Study Guide” by Judith E. Tintinalli et al.
- “Advanced Cardiac Life Support (ACLS) Provider Manual” by American Heart Association.
Psychology and Psychiatry:
- “Abnormal Psychology” by Ronald J. Comer.
- “Diagnostic and Statistical Manual of Mental Disorders (DSM-5)” by American Psychiatric Association.
- “Psychology” by David G. Myers and C. Nathan DeWall.
- “The Oxford Handbook of Clinical Psychology” by David H. Barlow.
Science and Technology:
- “Fundamentals of Physics” by David Halliday, Robert Resnick, and Jearl Walker.
- “Chemistry: The Central Science” by Theodore L. Brown, H. Eugene LeMay, and Bruce E. Bursten.
- “Introduction to Computer Science: A Textbook for Beginners” by J. Glenn Brookshear.
- “Artificial Intelligence: A Modern Approach” by Stuart Russell and Peter Norvig.
Literature and Fiction:
- “To Kill a Mockingbird” by Harper Lee.
- “1984” by George Orwell.
- “Pride and Prejudice” by Jane Austen.
- “The Great Gatsby” by F. Scott Fitzgerald.
- “One Hundred Years of Solitude” by Gabriel García Márquez.
History and Non-Fiction:
- “A People’s History of the United States” by Howard Zinn.
- “Sapiens: A Brief History of Humankind” by Yuval Noah Harari.
- “The Wright Brothers” by David McCullough.
- “The Immortal Life of Henrietta Lacks” by Rebecca Skloot.
Conclusion
“In an era marked by rapid advancements and expanding horizons, the pursuit of knowledge stands as a timeless endeavor. From the vast realms of science and technology to the intricacies of art and literature, our thirst for understanding fuels our progress.
In this ever-evolving landscape, we embark on a journey to explore, learn, and uncover the wisdom contained within the pages of reference books. These invaluable companions serve as beacons of insight, guiding us through the complexities of our world and illuminating the path to discovery.”