The pain in the knees is a frequent complaint that can be traced to a variety of underlying ailments among them are Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS). Both conditions cause pain in the kneecap area but they differ in characteristics, causes, and treatments.
We will look at the differences and similarities between Chondromalacia Patella and PFPS, aiding you in gaining an understanding of knee-related issues and ways you can manage them efficiently.
Definition of Chondromalacia Patella
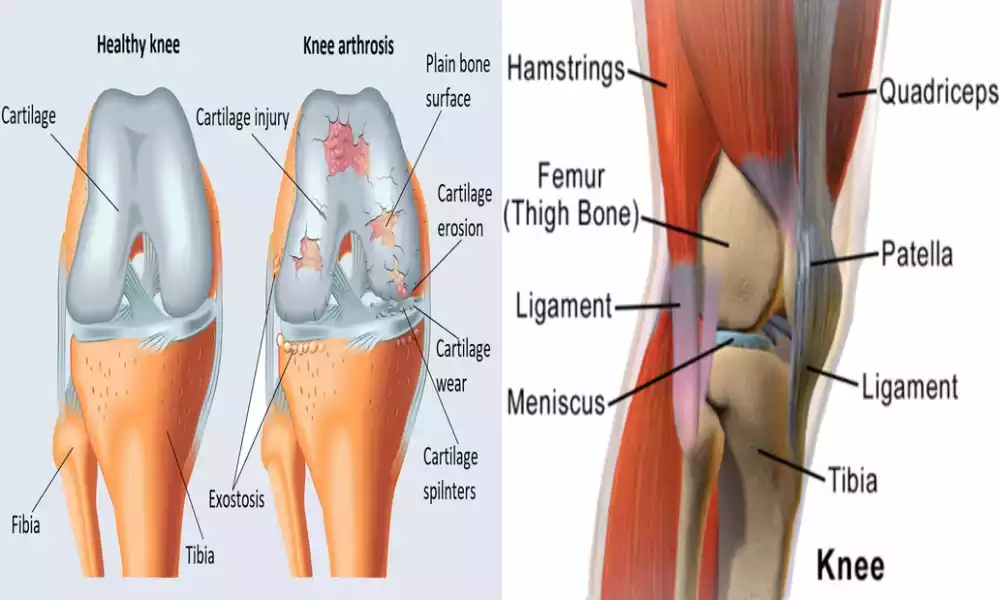
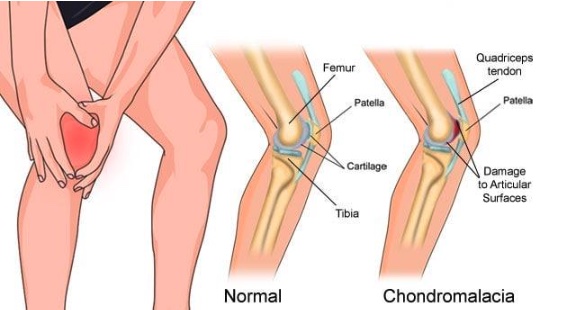
Chondromalacia Patella often referred to by the name of “runner’s knee,” is a medical condition that manifests itself in the weakening and degeneration of the cartilage that lies on the side of the patella (kneecap).
The condition is usually caused by many factors, including excessive use and muscle imbalances, injuries, or aging-related changes which can result in anterior knee pain or discomfort especially when performing activities that require bending the knee for running, walking, or climbing steps.
Chondromalacia Patella can be a frequent reason for knee pain, especially among athletes and people who perform a lot of physical activities.
Definition of Patellofemoral Pain Syndrome
Patellofemoral Pain Syndrome (PFPS) is a knee disorder that is characterized by discomfort and pain in the knee’s front particularly in the area where the patella (kneecap) is in contact with the femur (thigh bone).
It is a very common orthopedic problem, commonly known as “runner’s knee” or “anterior knee pain syndrome.” PFPS is typically caused by an imbalance in the forces that affect the patella during joint motion causing discomfort and pain.
People suffering from PFPS frequently experience pain when engaging in activities that require bending the knee. This includes running and walking, jumping or climbing up and down the stairs. Long-term sitting with knees bent may also cause pain.
The causes for PFPS are different, however, the most common contributing factors are muscle imbalances, excessive use and improper tracking of the patella, and issues with knee alignment and biomechanics. Treatment for PFPS usually includes rest or physical therapy, managing pain, and fixing the root causes of the issue.

Importance of distinguishing between Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS)
The distinction difference between Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS) is vital for a variety of reasons:
- Accurate diagnosis: Both diseases share common symptoms, such as knee pain. However, they have distinct factors and causes. An accurate diagnosis guarantees your patients get the best treatment that addresses the root cause of their particular problem.
- Customized Treatment: Chondromalacia Patella often results from cartilage damage, whereas PFPS can be linked to joints and muscle imbalances. Treatment options, like exercises in physical therapy, medicines, or surgical procedures are able to differ greatly. The ability to tailor treatment to your specific situation improves the effectiveness of treatment.
- Prevention: Understanding the specific problem allows for specific preventive steps. Patients are able to be educated about the risk factors and ways to prevent aggravating their specific problem. For instance, PFPS patients may benefit from exercises that increase the strength of their muscles and flexibility and flexibility, while Chondromalacia Patella patients may need to limit high-impact activities.
- Avoiding unneeded procedures: The wrong diagnosis can cause costly medical treatments, like surgeries. If a patient diagnosed with PFPS is not properly treated for Chondromalacia Patella or reversed, they could undergo surgery or procedures that do not treat the real issue which could lead to difficulties or even disappointment.
- Rehabilitation and Recovery: The rehabilitation programs available specifically designed for Chondromalacia Patella and PFPS vary dramatically. Understanding the proper condition is essential to ensure that patients follow the appropriate rehabilitation procedures, which could greatly affect the speed and effectiveness of the recovery.
- Long-Term Results: Effectively identifying and managing these issues can affect the long-term outcome. A well-planned treatment and management strategy could result in less discomfort, better knee function, as well as a higher level of living for the patients.
- Resources Allocation: A precise diagnosis can help healthcare professionals efficiently allocate resources. It helps ensure that patients suffering from specific medical conditions receive the correct quality of care, maximizing the use of healthcare resources.
Recognizing Chondromalacia Patella and Patellofemoral Pain Syndrome is crucial to provide people with efficient and appropriate treatment, enhancing their outcomes, while avoiding unnecessary medical procedures.
Comparison Table of Chondromalacia Patella and Patellofemoral Pain Syndrome
Here’s a comparison table highlighting the key differences between Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS):
| Characteristic | Chondromalacia Patella | Patellofemoral Pain Syndrome (PFPS) |
|---|---|---|
| Definition | Softening and deterioration of the cartilage beneath the patella. | Pain and discomfort around the front of the knee, usually due to patellar misalignment and muscle imbalances. |
| Common Names | Runner’s knee | Runner’s knee, Anterior Knee Pain Syndrome |
| Underlying Causes | Cartilage damage, overuse, muscle imbalances, trauma, or age-related factors. | Muscle imbalances, patellar tracking issues, overuse, biomechanical factors, or alignment problems. |
| Pain Location | Typically felt under or around the kneecap. | Predominantly in the front of the knee around the patella. |
| Pain Triggers | Activities involving knee bending, such as climbing stairs, running, or squatting. | Activities that load the knee, including running, jumping, squatting, or prolonged sitting with knees bent. |
| Crepitus (Grinding Sensation) | Often present due to cartilage wear. | Less commonly associated with crepitus. |
| Diagnosis | Physical examination, imaging (MRI, X-ray), and evaluation of symptoms. | Clinical assessment, imaging (X-ray, MRI, CT scan), and examination of knee function. |
| Treatment Options | Rest, activity modification, physical therapy, medications, injections, and surgery (in severe cases). | Rest, RICE (Rest, Ice, Compression, Elevation), physical therapy, pain management, bracing, injections, and surgery (rarely). |
| Primary Focus in Treatment | Addressing cartilage damage and inflammation. | Correcting muscle imbalances, improving patellar tracking, and addressing biomechanical issues. |
| Prevalence | Less common compared to PFPS. | More common, especially in active individuals. |
| Prognosis | Can be variable depending on the extent of cartilage damage. | Generally favorable with appropriate treatment, and full recovery is common. |
| Surgical Interventions | May be considered in severe cases involving significant cartilage damage. | Rarely necessary and typically considered only if conservative treatments fail. |
| Prevention | Emphasizes minimizing knee strain and addressing predisposing factors. | Focuses on muscle strengthening, flexibility, and alignment correction. |
| Long-Term Management | May require ongoing management, especially if cartilage damage is extensive. | Often manageable with lifestyle modifications and exercises. |
It’s important to note that accurate diagnosis by a healthcare professional is crucial to determine the specific condition and tailor the treatment accordingly.
How are they similar?
Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS) have a lot in common despite their distinct cause and mechanisms.
There are some similarities between these two conditions:
- The Anterior Knee Pain: Both of these conditions generally manifest as pain on the anterior part of the knees, particularly on the patella (kneecap).
- Aggravation due to Activities: For both Chondromalacia Patella or PFPS the pain can increase during activities that require bent knees like running, climbing stairs, jumping, or doing squats.
- Overlapping and its Risk Factors: Although the main causes are different, certain risk factors are common for both of the conditions. They include excessive use in the knee joint imbalances in the muscles (especially those of quadriceps muscle) and other actions that put stress on the knee.
- Alternatives for Conservative Treatment: The two conditions Chondromalacia Patella as well as PFPS may generally be treated with a conservative approach. Treatment options include physical therapy, rest, treatment for pain (e.g., NSAIDs), and lifestyle changes.
- Strengthening and rehabilitation: Physical therapy and exercises that strengthen the knee muscles are vital components of the treatment of both conditions. These exercises can aid in improving knee stability and ease pain.
- Bracing or taping: In some instances, bracing or taping techniques can be utilized for both conditions in order to support and ease the strain on the patella.
- Injections: Corticosteroid injections, or other injections (e.g. hyaluronic acids) can be considered part of the treatment plan for the two conditions Chondromalacia Patella and PFPS to lessen pain and inflammation.
- Surgery (in Extreme Cases): Although rare for both conditions surgery may be considered if conservative treatments are not effective or when there is intense chronic pain. Surgery options be used to treat cartilage injuries (Chondromalacia Patella) or realignment of the patella (PFPS).
- The emphasis is on lifestyle modifications: The two conditions typically require patients to alter their lifestyle for example, avoidance of activities that can cause discomfort and maintaining the weight of a healthy person to decrease stress on the knee joint.
Although Chondromalacia Patella as well as PFPS are distinct in their diagnosis and causes, they have common characteristics that include knee pain in the anterior region the possibility of treatment with a conservative approach, and the necessity of strengthening and rehabilitation in their treatment. Healthcare professionals must be able to identify the exact disease to provide the most effective treatment.
Symptoms and clinical presentation
The symptoms and the clinical manifestations and clinical presentation of Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS) are often similar however they also possess distinct characteristics.
Here’s a list of their distinct symptoms and clinical manifestations:
Chondromalacia Patella:
- Anterior knee pain: The main manifestation that is the hallmark symptom of Chondromalacia Patella will be continuous tender, dull pain on the knee’s front particularly around or behind the patella.
- Crepitus (Grinding Feeling): Patients may feel a popping, grinding, or cracking feeling (crepitus) whenever they move the knee joint. The sensation is usually caused by wear and tear on the cartilage.
- Pain Accompanied by Activity: It is common for pain to get worse when you bend the knee, like climbing or descending stairs, kneeling or squatting, or sitting for long periods in a knee-bending position.
- Pain after rest: People suffering from Chondromalacia Patella might also feel discomfort after prolonged periods of rest, particularly when they first get up early in the morning or after sitting for a long duration of time.
- Swelling: A few patients might experience mild knee swelling, especially after exercise or when knee pain becomes more severe.
Patellofemoral Pain Syndrome (PFPS):
- Anterior knee pain: Similar to Chondromalacia Patella, PFPS presents with anterior knee pain. The pain is usually located around the patella, but may extend to other areas.
- Pain triggered by Activities: The majority of pain is caused by activities like running and jumping, squatting as well as prolonged sitting while knees are bent. The pain associated with PFPS is typically described as a numbness that is deep.
- Pain During Descending Stairs: Patients suffering from PFPS can be particularly afflicted by pain while descending the stairs or down hills because this type of movement causes pressure on the patellofemoral joint.
- Pain after rest: Like Chondromalacia Patella, PFPS pain can also happen during rest, like when you stand up following a sitting few minutes.
- Grinding or Popping Sensation: A few people with PFPS might feel or hear the sound of grinding or popping in the knee area, particularly when the joint is moved.
- Knee instability: Patients may feel a sensation that their knees are unstable or “giving way,” although this isn’t as prevalent in other knee disorders.
It’s crucial to recognize that symptoms from each condition can differ in severity and can be temporary or disappear over the course of the. In addition, certain individuals might have a mix of these symptoms.
A precise diagnosis by a qualified healthcare professional is vital to distinguish from Chondromalacia Patella or PFPS and to develop a suitable treatment program based on the particular symptoms.
Pain during activities like running, jumping, or climbing stairs
The pain that occurs during sports like running or jumping stairs is a frequent sign that may be connected with knee problems of various kinds such as Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS).
The following is how the symptom could be present in both of these conditions:
Chondromalacia Patella:
When you suffer from Chondromalacia Patella, pain during sports like jumping, running, as well as climbing stairs, is a common sign. This is due to the weakening and degrading of the cartilage below the patella.
This may cause more friction and discomfort as the patella rubs in contact with the femur (thigh bone). The pain is generally described as having a dull painful sensation that is typically situated behind or around the kneecap. The pain can get worse as the activity progresses and it may continue to linger afterward.
Patellofemoral Pain Syndrome (PFPS):
PFPS can also cause discomfort during activities that strain your knee joint for example running or jumping up steps. The pain is typically felt in the front part of the knee near the patella. It is usually described as a throbbing pain.
The pain associated with PFPS typically stems from factors such as muscle imbalances, patellar tracking problems, or biomechanical issues that cause an abnormal amount of stress in the patellofemoral joint during these exercises. The climb up stairs, particularly can be very painful for those suffering from PFPS because it puts more stress on the patella.
It is important to remember that although pain associated with those activities can be a common symptom, the root causes of pain vary between the two types of conditions.
Chondromalacia Patella is typically caused by cartilage damage and PFPS is associated with issues such as muscle imbalances or joint mechanics. An accurate diagnosis by a medical specialist is crucial to identify the precise condition and create the appropriate treatment plan that is specific to the needs of the patient.
Potential need for surgical intervention in severe cases
In both Chondromalacia and Patellofemoral Pain Syndrome (PFPS) Surgery is usually thought of only in extreme cases that haven’t been able to respond adequately to conventional treatments.
Here’s a quick overview of the possible need for surgery for these ailments:
Chondromalacia Patella:
- The indications for surgery: The procedure to treat Chondromalacia Patella is a rare event and is generally reserved for the most severe cases when traditional treatments have failed to ease symptoms. Surgery could be considered if there is a large amount of cartilage damage or other structural defects that contribute to the problem.
- Surgery Options Surgery options to treat Chondromalacia Patella could comprise:
- Arthroscopy: The minimally invasive process uses a small camera to examine and treat cartilage that is damaged. Methods like debridement (removal of tissue that is damaged) and microfracture (stimulating the growth of new cartilage) are possible.
- Realignment surgery: In cases where problems with patellar alignment contribute to the problem surgery procedures such as a realignment of the patella or osteotomy in the tibia could be thought of to improve the alignment.
- Rehabilitation: Recovery from surgery for Chondromalacia Patella differs based on the procedure that is performed however, it is usually a time of rehabilitation, which includes physical therapy to help regain strength and mobility.
Patellofemoral Pain Syndrome (PFPS):
- Indications for Surgery: Surgery for PFPS is less frequent than Chondromalacia Patella. The procedure is typically thought of only after conservative treatments have failed, and the patient is still suffering chronic and debilitating symptoms.
- Surgery Alternatives: The surgical procedures that are available for patients with PFPS can include:
- Lateral Release The procedure involves cutting off the lateral retinaculum (tissue on the exterior of the patella) to relieve pressure and enhance patellar tracking.
- realignment surgery: In cases of extreme malalignment, procedures to realign the spine like an osteotomy of the tibial tubercle or Trochleoplasty can be thought of to fix the position of the patella.
- Rehabilitation: Recovery from PFPS surgery is a time of rehabilitation. This could include physical therapy to increase flexibility and strength. The precise timeframe and the requirements will depend on the surgical procedure used.
It’s important to note that surgery is typically considered to be a last resort when the alternatives have been exhausted It is usually reserved for those with significant discomfort, functional impairment, or structural issues that can’t be resolved with non-surgical approaches.
The decision to go through with surgery must be taken after consultation with a certified orthopedic surgeon who will examine the patient’s health and discuss the possible advantages and risks associated with the surgery.
Preventive measures for both conditions
The preventive measures that are available for both Chondromalacia Patella as well as Patellofemoral Pain Syndrome (PFPS) are mainly focused on reducing risks and addressing the biomechanical issues that may cause these conditions.
These are preventive steps that can be applied to both conditions:
- Maintain an appropriate weight: Excess body weight puts additional strain on your knee joints. Being healthy can decrease the likelihood of developing these conditions as well as reduce symptoms if already in the process of developing.
- Proper Warm-Up and Stretching: Always warm up prior to participating in physical activities. Also, include stretching exercises that are targeted at the quadriceps and muscle groups of the calf and hamstrings. Flexibility can be improved to avoid muscle imbalances and decrease strain on knee joints.
- Gradual increase in activity: When starting a new program of exercise or training begin slowly. Intense increases or duration may strain the knee joint, leading to injury and pain.
- Proper footwear: Wear appropriate footwear that is appropriate for the particular task you’re engaged in. The right shoes, that fit well, can assist in distributing forces evenly and minimize the likelihood of knee problems.
- Strength training: Incorporate strength-training exercises to strengthen the muscles surrounding the knee, specifically the quadriceps and the hamstrings. Strong muscles can stabilize the knee joint and absorb shocks during physical activity.
- Biomechanical Examination: Consult with a health professional or physical therapist to perform a biomechanical analysis of your gait, movement, and patterns. Recognizing and fixing issues such as malalignment or overpronation can lower the risk of knee injuries.
- Functional Training: Implement functional exercise routines that replicate the actions you routinely perform like squatting, for example, or climbing stairs. This can increase your body’s capacity to manage these activities without putting too much stress on the knee.
- Avoid sitting for long periods of time with bent knees: If your work or everyday activities require prolonged sitting, you should take breaks in between to get on your feet and stretch your legs. Maintaining knees bent for long periods of time can result in knee discomfort.
- Cross-training: Participate in a variety of physical exercises to prevent injuries caused by overuse. Cross-training helps you maintain your overall fitness and reduce the strain on your knees from repetitive exercise.
- Pay attention to your body: Pay attention to any indications of discomfort or pain that you experience during your physical activity. If you feel knee pain, you need to treat it immediately rest if needed, and seek medical assistance in the event that symptoms persist.
- Include low-impact activities: Include low-impact workouts like cycling, swimming, or elliptical exercise within your exercise routine. These exercises can improve your cardiovascular health and reduce the impact on your knees.
- Utilize Proper Techniques: When engaging in physical or sporting activities ensure that you employ the proper techniques and follow the guidelines for movement and form.
- Orthotic Devices: When advised by a medical professional, think about the use of orthotic devices or shoe inserts to correct any alignment issues and lessen stress on the knees.
Keep in mind that preventive measures will be most effective when tailored to your individual needs and situation. Speak with your healthcare professional or physical therapist to get advice on implementing these strategies based on your personal health and risk factors.
Lifestyle modifications
Lifestyle changes are a key factor in the prevention and management of knee disorders like Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS).
Here are some changes to your lifestyle that may help ease symptoms and decrease the likelihood of developing these diseases:
- Maintain a healthy weight: Excess body weight can put more stress on your knees. If you’re obese or overweight you can lose weight by following eating a balanced diet and consistent exercise can ease the pressure on the knee joints.
- Keep active and engaged in regular exercise: A regular exercise routine, which includes low-impact activities like cycling, swimming as well and water aerobics can assist in keeping knee joints healthy. Talk to a doctor or physical therapist to create an effective and safe workout routine.
- Warm-up and Cool Down: Prior to exercise or any physical activity, do a thorough warm-up that prepares your joints and muscles. Then, follow cooling down routines to slowly lower your heart rate and avoid stiffness of muscles.
- Flexibility and stretching: Include regular stretching exercises into your workout routine, with a focus on the muscles surrounding the knee, like the quadriceps, hamstrings, and the calf muscles. Flexibility can help reduce tension in your knee joint.
- Increase the strength of the Quadriceps as well as Hamstrings: A strong muscle support system surrounding the knee can aid in stabilizing the joint and decrease the chance of injury. Incorporate strength-training exercises targeting the muscles.
- Cross-training: Change your routines of exercise to avoid injuries from overuse. Cross-training is the process of engaging in various activities to spread the burden over different joints and muscle groups.
- Proper footwear: Invest in well-fitting and supportive shoes that are suitable for your specific physical activity. The right shoes will help you maintain the proper alignment of your knee and decrease strain.
- Orthotic Equipment: If you have problems with alignment or biomechanical you should consult a healthcare specialist to design custom orthotic devices or shoe inserts to address these problems.
- Pacing and rest: Be mindful of your level of physical activity and pay attention to your body. Do not overwork yourself, make breaks between physical activities, and make sure you have enough time off between workouts.
- Modify High-Impact Activities: If you are a fan of intense sports or activities, you should consider altering them to minimize the strain to your knees. For example, consider choosing soft surfaces for running or change to less-impact types of exercise.
- Utilize Proper Techniques: When participating in physical activities or sports make sure you employ appropriate techniques and adhere to established guidelines regarding form and movement.
- Avoid prolonged sitting with knees bent: If your job or routine requires sitting for long periods, you should regularly break to get up, stretch, or stroll around. The knees that are bent for prolonged periods may result in knee pain.
- Control Stress: Stress levels that are high can cause muscle tension that can increase knee pain. Utilize stress management strategies like relaxation exercises, meditation, or mindfulness.
- Get a Health Professional’s advice: If you experience chronic knee pain or previous knee issues seek out a medical professional or orthopedic expert for advice on lifestyle changes and preventive strategies that are tailored to your specific needs.
Make sure that any lifestyle changes you make are adapted to your individual circumstances and any existing conditions you might have. A consultation with a healthcare expert or physical therapist may provide you with individualized advice and suggestions to prevent and treat knee-related issues.
Similarities Between Chondromalacia Patella and Patellofemoral Pain Syndrome
Chondromalacia Patella as well as Patellofemoral Pain Syndrome (PFPS) are knee disorders that have a number of similarities:
- The Anterior Knee Pain: The majority of both conditions manifest as pain on the knee’s front particularly on the patella (kneecap).
- Aggravation caused by activities: Pain in both conditions is likely to increase during activities that require bent knees like climbing the stairs or running, jumping, or sitting down.
- Overlapping causes and risk factors: Although the primary causes are different, certain risk factors are common for both of the conditions. They include excessive use in the knee joint imbalances in the muscles (especially that of the quadriceps muscles) as well as actions that put stress on the knee.
- Alternatives for Conservative Treatment: Both Chondromalacia Patella as well as PFPS may generally be treated with a conservative approach. Treatment options could include physical therapy, rest as well as treatment for pain (e.g., NSAIDs) as well as lifestyle modifications.
- Strengthening and rehabilitation: Exercises and physical therapy to strengthen the muscles surrounding the knee are vital components of the treatment plan for both of the conditions. These exercises will help improve knee stability and ease pain.
- Bracing or taping: In some instances, bracing or taping techniques are used in both conditions in order to assist and reduce stress on the patella.
- Injections: Corticosteroid injections, or other injections (e.g. hyaluronic acids) could be considered an element of treatment for each Chondromalacia Patella and PFPS to decrease pain and inflammation.
- Surgery (in severe cases): Although rare in both cases surgery may be considered if conservative treatments are not effective or when there is intense chronic pain. Surgery options be used to treat cartilage injury (Chondromalacia Patella) or realignment of the patella (PFPS).
- Focus on Lifestyle Modifications: These two conditions usually require patients to modify their lifestyle including avoidance of activities that can cause discomfort and ensuring an appropriate weight to lessen strain on the knee joint.
Although Chondromalacia Patella as well as PFPS are distinct in their diagnoses and causes They share some common characteristics that include an anterior knee ache, the possibility for conservative treatment, and the significance of rehabilitation and strengthening the muscles in their treatment.
It is essential for healthcare professionals to be able to pinpoint the specific disease to provide the most effective treatment.
Reference Books
Certainly! Here are some reference books on knee conditions, including Chondromalacia Patella and Patellofemoral Pain Syndrome (PFPS), as well as related topics in orthopedics and physical therapy:
- “Current Concepts of Orthopedic Physical Therapy” by Daniel S. Thigpen, Joshua Cleland, Robert C. Manske, and Mark Dutton
- This comprehensive book covers various orthopedic conditions, including knee-related issues, and provides insights into assessment, treatment, and rehabilitation strategies.
- “Knee Surgery: Complications, Pitfalls, and Salvage” by Giles R. Scuderi and Alfred J. Tria Jr.
- Focusing on surgical aspects of knee problems, this book delves into complications, pitfalls, and salvage procedures associated with knee surgery.
- “Knee Arthroscopy: A Masterclass” by David Barrett and Justin Cobb
- This book offers an in-depth exploration of knee arthroscopy, a common surgical procedure for various knee conditions.
- “Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation” by Walter R. Frontera, Julie K. Silver, and Thomas D. Rizzo
- A comprehensive resource on musculoskeletal disorders, this book covers knee conditions, rehabilitation techniques, and pain management.
- “Physical Rehabilitation of the Injured Athlete” by James R. Andrews, Gary L. Harrelson, and Kevin E. Wilk
- Targeting sports-related injuries, this book provides insights into the rehabilitation of athletes, including those with knee injuries.
- “The Knee: Clinical Applications” by David McAllister, Nicholas Sgaglione, and Russell F. Warren
- This clinical resource offers a detailed examination of various knee conditions and their management, with a focus on surgical approaches.
Conclusion
The distinction between Chondromalacia patella in addition to Patellofemoral Pain Syndrome (PFPS) is crucial for a clear diagnosis and individualized treatment. Although both knee conditions have some commonalities, including anterior knee pain, and have similar treatments, they each have distinct causes that require specific treatments.
Correct diagnosis by health specialists, as well as lifestyle changes along with preventive strategies, will significantly improve the management and treatment of the ailments and improve knee health and overall well-being.