Androgen Insensitivity Syndrome and Mullerian Agenesis are two distinct but related medical conditions that affect individuals’ reproductive and sexual development. While both conditions involve variations in the development of sexual organs and may pose unique challenges, they differ in their genetic origins, hormonal effects, physical characteristics, diagnosis, and treatment approaches.
We will explore the key differences and similarities between AIS and Mullerian Agenesis, shedding light on these conditions to promote better understanding and support for affected individuals.
What is Androgen Insensitivity Syndrome?
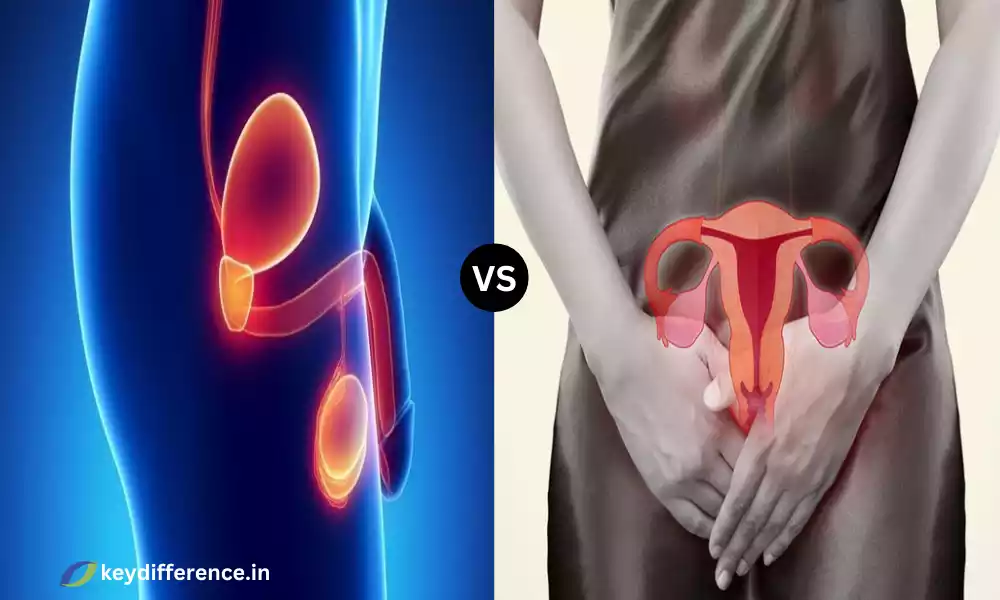
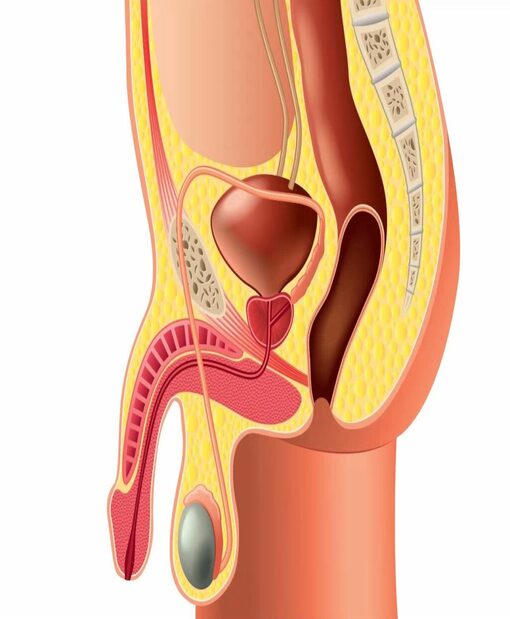
Androgen Insensitivity Syndrome (AIS) is a rare genetic disorder that limits an individual’s capacity to react to male sexual hormones known as androgens. Individuals who suffer from AIS tend to be genetically male (having one X chromosome as well as one Y) however, their bodies aren’t able to entirely develop the male traits externally as well as internally because of an insensitivity, either complete or partial, to androgens.
This means that people who suffer from AIS may exhibit physical characteristics that are normally related to females like female breasts, external genitalia, and lack of male-specific sexual traits such as facial hair and the deep voice.
AIS is an endocrine disease with different levels of androgen sensitivity and can affect an individual’s physical, psychological, and mental well-being. The exact presentation and management of AIS will vary greatly among affected people.
What is Mullerian Agenesis?
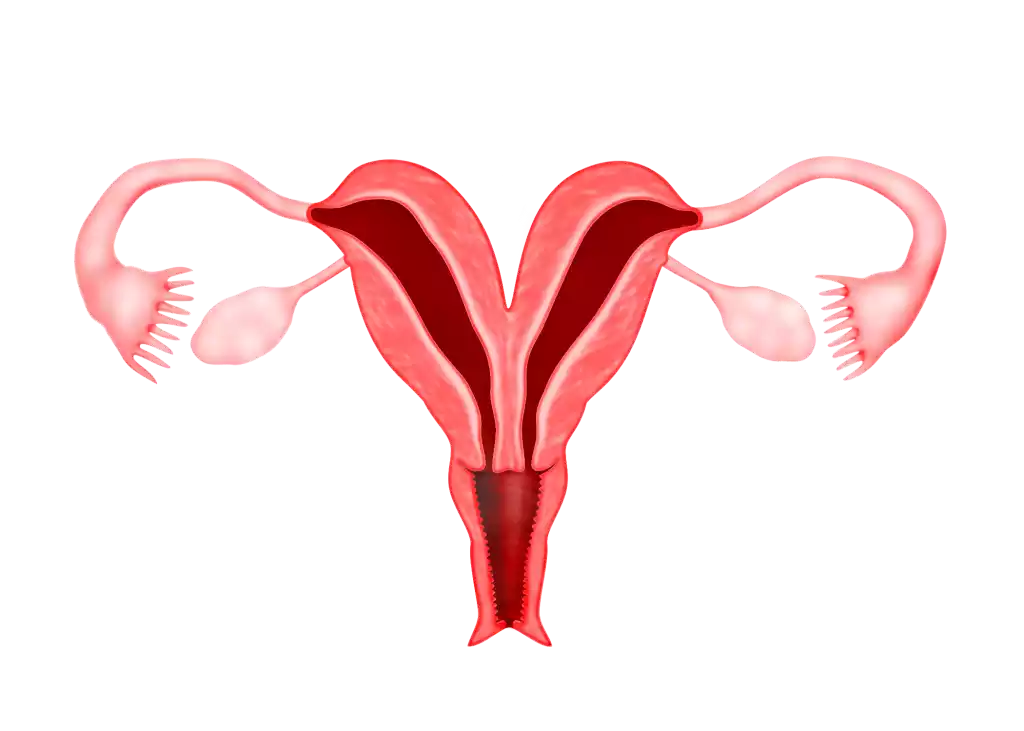
Mullerian Agenesis, also known as Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome, is a congenital disorder characterized by the incomplete or absent development of the female reproductive tract, including the uterus (womb) and upper part of the vagina. Women who suffer from Mullerian Agenesis typically have normal external genitalia but don’t have a uterus that is fully developed or a cervix. The condition can be seen at birth and is evident in adolescence when the affected don’t menstruate.
Mullerian Agenesis may have major consequences for fertility since those suffering from this condition typically are not able to carry a pregnancy because of the absence of a uterus that is functional. But, it doesn’t alter other aspects of women’s health. People with the condition generally possess normal secondary reproductive characteristics and hormone production. The diagnosis is usually made during the time when a girl does not menstruate and it is confirmed by ultrasound and pelvic exams.
Treatment options for Mullerian Agenesis could involve surgical procedures that create a neovagina or in certain cases the possibility of uterine transplantation for women who are interested in having a baby. Support for emotional and psychological well-being is a crucial element of coping with this condition since it could have a significant influence on one’s confidence in themselves and their appearance.
Comparison Table of Androgen Insensitivity Syndrome and Mullerian Agenesis
Here is a comparison table of Androgen Insensitivity Syndrome (AIS) and Mullerian Agenesis (Mayer-Rokitansky-Küster-Hauser syndrome) to highlight their key differences and similarities:
| Aspect | Androgen Insensitivity Syndrome (AIS) | Mullerian Agenesis (MRKH Syndrome) |
|---|---|---|
| Genetic Basis | XY chromosomal pattern (typically) | Typically XX chromosomal pattern |
| Hormonal Effects | Partial or complete insensitivity to androgens, leading to feminization of external genitalia and breasts | Normal response to hormones, except for the absence of a uterus and upper part of the vagina |
| External Genitalia | Typically feminine in appearance, with female external genitalia (clitoris, labia, and vaginal introitus) | Typically normal female external genitalia |
| Internal Reproductive Organs | Testes are present instead of ovaries, and the internal male reproductive structures (seminal vesicles, vas deferens) may develop | Absence or underdevelopment of the uterus, cervix, and upper part of the vagina |
| Secondary Sexual Characteristics | Lack of male secondary sexual characteristics like facial hair, deep voice, and male pattern body hair | Normal female secondary sexual characteristics (breast development, feminine body contours) |
| Menstruation and Fertility | Absent menstruation; infertility due to the lack of functional female reproductive organs | Absent menstruation; infertility due to the absence of a uterus |
| Diagnosis | Based on genetic testing, hormone levels, and physical examination | Based on clinical evaluation, pelvic imaging, and medical history |
| Management and Treatment | Hormone replacement therapy (HRT) to induce feminization; surgical options for gonadectomy and potential neovaginal construction | Surgical options for neovaginal construction; psychological support and counseling |
| Psychological and Emotional Considerations | May face gender identity and body image issues; require psychosocial support | May experience emotional distress related to infertility; may need psychological support |
It’s important to note that both AIS and Mullerian Agenesis are complex conditions with variations in presentation and management. The experiences and needs of individuals with these conditions can differ, so personalized care and support are crucial.
Physical characteristics and development
Here, we will delve deeper into the physical characteristics and development of individuals with Androgen Insensitivity Syndrome (AIS) and Mullerian Agenesis (Mayer-Rokitansky-Kuster-Hauser syndrome).
Androgen Insensitivity Syndrome (AIS):
- External Genitals: Individuals with AIS typically have female external Genitalia. This may include a clitoris, labia majora and labia minora. The appearance is usually feminine, and it can be difficult to distinguish cisgender females from them just by looking at their external appearance.
- The development of breasts: Due to the body’s inability to respond to androgens. Those who suffer from AIS typically experience breast growth in puberty. This process can be similar to gender-neutral females.
- The absence of male secondary sexual Specifications: AIS individuals lack the usual male secondary sexual traits, for example, growing facial hairs, having a strong voice, and male-pattern body hair.
- Internal Reproductive Organs: Inside, AIS individuals have testes instead of Ovaries. Testes typically result in the production of male hormones that are normal (testosterone). However, they do not produce the typical masculinizing effects because of the insensitivity to androgens.
Mullerian Agenesis (MRKH Syndrome):
- External Genitalia: In general, patients who suffer from MRKH syndrome have normal female external male genitalia. This includes a clitoris labia majora and labia minora. There are typically no obvious signs that the condition is present.
- The development of breasts: The development of breasts in those with MRKH syndrome develops as it does in transgender females in puberty.
- Standard Female Sexual Characteristics: The MRKH syndrome doesn’t influence the normal development of female secondary sexual traits such as breast size female body contours as well as the lack of masculine-pattern male secondary characteristics.
- Internal Organs for Reproduction: One of the hallmarks of MRKH disorder is the lack of development or absence of internal female reproductive organs. This includes the uterus, cervix, and the upper portion of the vagina. Ovaries are generally present and functioning.
Those who suffer from AIS might have female external genitalia as well as breast growth, even though they have male-specific hormonal and genetic traits. They don’t have male sexual secondary traits.
However people with MRKH are female with typical external characteristics and development, but they do not have an active uterus and the vagina’s upper portion internally. Both disorders can have profound physical and psychological consequences and the treatment usually involves taking care of the particular demands and issues of each person.
Genetic Factors in Mullerian Agenesis
Mullerian Agenesis, also known as Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome, is a congenital disorder primarily characterized by the absence or underdevelopment of the uterus and upper part of the vagina in individuals with typically female external genitalia. Although the reason for MRKH syndrome is not completely known there is evidence to suggest a genetic cause and multifactorial causes.
Here are some genetic causes and facets of MRKH syndrome:
- Multifactorial Inheritance: MRKH disorder is believed to be the result of an intricate interplay between environmental and genetic influences. It is regarded as a multifactorial disorder, meaning that genetic susceptibility as well as environmental influences are involved in the development of this condition.
- Familial Occurrence: MRKH syndrome can be found in families, indicating that there is a genetic predisposition. However, it doesn’t necessarily follow a strict Mendelian inheritance pattern where one gene mutation can cause the disorder. More likely, a variety of genetic factors may influence the susceptibility to MRKH syndrome.
- Candidate Genes: A variety of potential genes have been investigated in relation to MRKH-related syndrome, however, no single causal gene has been discovered. The candidate genes are WNT4, WNT7A, LHX1 and others. The mutations or variations that occur in these genes could affect the normal development of embryos and lead to a lack or insufficient development of the female reproductive tract.
- Chromosomal Anomalies: In some instances, those with MRKH disorder may suffer chromosomal anomalies, like deletions or translocations, which influence genes that are involved in the development of the reproductive tract. These chromosomal mutations can cause disruption to the normal development of the vagina and uterus.
- Epigenetic Factors: epigenetic modifications such as DNA methylation and histone modification can affect the expression of genes in the development of embryos. Epigenetic changes could cause the formation of MRKH syndrome.
- Research in progress: The genetic basis of the MRKH syndrome remains an active field of study and ongoing studies seek to determine the specific genetic causes and mechanisms that are responsible for the disorder. The advancements in molecular and genomic methods may result in an understanding of its genetic roots in the near future.
It is important to remember it is important to note that MRKH syndrome can be a varied condition. Those suffering from MRKH could have different medical and genetic characteristics. Furthermore, not all cases of MRKH syndrome can be correlated with genetic mutations that are known or variants.
Genetic counseling and comprehensive genetic tests may be suggested for those suffering from MRKH syndrome as well as their family members to know the genetic causes and provide details on the risk of inheritance and patterns.
Similarities Between Androgen Insensitivity Syndrome and Mullerian Agenesis
While Androgen Insensitivity Syndrome (AIS) and Mullerian Agenesis (Mayer-Rokitansky-Kuster-Hauser syndrome) are distinct conditions that primarily affect individuals with different chromosomal and hormonal backgrounds, there are a few similarities between them:
- External Genitalia: The two conditions AIS as well as Mullerian Agenesis may result in people with typically female external Genitalia. In AIS those with complete androgen insensitivity can have totally female external genitalia. people with Mullerian Agenesis generally have female external genitalia that are normal.
- The development of breasts: In both conditions, the majority of people have normal development of their breasts in puberty. This is in line with the typical female secondary sexual characteristics.
- normal female secondary sexual Specifications: AIS and Mullerian Agenesis are not usually associated with the development of typical female sexual secondary traits like breast growth and female body contours as well as the lack of masculine-pattern secondary characteristics.
- Menstrual absence: Individuals with both AIS and Mullerian Agenesis usually do not menstruate. In AIS the reason is that those affected don’t have a functioning uterus. However, in Mullerian Agenesis, the uterus is absent or not developed.
- Fertility: These two conditions can be caused by infertility. In AIS the cause of infertility is the lack of a functioning female reproductive tract. In contrast, Mullerian Agenesis is due to the lack or insufficient development of the uterus.
- Psychological and emotional impact: Individuals with AIS and Mullerian Agenesis can have emotional and psychological issues due to their condition like issues with body image, worries regarding fertility, and gender concerns about identity. Counseling and support may be necessary to tackle these issues that affect their health.
It’s important to recognize that, despite the similarities, AIS as well as Mullerian Agenesis both have distinct causes and consequences for those affected. AIS is mostly related to androgen receptor insensitivity, which has a direct impact on people with XY chromosomes.
Mullerian Agenesis is characterized by the absence or lack of development that affects the female reproductive tract and predominantly affects people who have XX chromosomes. Both disorders require different ways of diagnosing and different approaches to managing the specific issues.
Counseling and support for individuals with AIS and Mullerian Agenesis
Counseling and support for individuals with Androgen Insensitivity Syndrome (AIS) and Mullerian Agenesis (Mayer-Rokitansky-Kuster-Hauser syndrome) are essential aspects of their overall care. These disorders can have significant physical as well as psychological impact on those affected and providing the appropriate assistance is vital.
Here are some important considerations to consider when seeking counseling and support:
- Multidisciplinary Care Teams:
- Establishing multidisciplinary teams of care which include gynecologists, endocrinologists psychologists, genetic counselors, psychologists and social workers will provide a full range of support to patients who suffer from AIS as well as Mullerian Agenesis.
- Information and Education:
- Inform the public in a clear and concise manner regarding the disease, its causes, consequences and treatments. Making sure that patients and their families have a clear knowledge of the condition could aid in reducing the anxiety, confusion and stress.
- Emotional Support:
- Provide emotional support to deal with the psychological effects of the disorder. Some people may experience feelings of anxiety, body image concerns and issues related to their sexuality and gender identity. Counseling can be an open and safe environment to talk about and deal with these emotions.
- Coping Strategies:
- Learn coping strategies and resilience strategies to help individuals deal with the challenges unique to AIS or Mullerian Agenesis. This may include stress management strategies and strategies to build self-confidence and acceptance.
- Peer Support Groups:
- Connect individuals suffering from AIS and Mullerian Agenesis group support or communities online that allow them to connect with other people with similar experiences. Sharing your experiences and tips among peers is extremely helpful.
- Fertility Counseling:
- For those who wish for biological babies offer fertility counseling and talk about the options available, including assisted reproductive technology (e.g. surrogacy, surrogacy, and in vitro fertilization) adoption or uterine transplantation (in certain instances in the case of The Mullerian Angenesis).
- Gender Identity Exploration:
- For people who suffer from AIS and especially those with partial androgen insensitivity, encourage their inquiry into how gender identities and their expression. Certain people may consider themselves females but others may be able to have a different identity. Be respectful of their preferences and offer services that are gender-neutral should they wish.
- Informed Decision-Making:
- Let patients make informed decisions regarding their surgical and medical choices. Talk about the risks, benefits and long-term potential of various treatment options.
- Long-Term Care Planning:
- Plan a long-term health plan which addresses the ongoing medical requirements such as hormonal replacement treatment (in AIS) or neovaginal treatment (in The Mullerian Angiogenesis).
- Privacy and Confidentiality:
- Be sure that medical and counseling information is kept private in order to protect the privacy of the patient.
Support and counseling must be tailored to meet the individual needs and preferences of every person. It is essential to provide an unprejudiced and safe environment that allows individuals to freely talk about the issues they face and make decisions that reflect their beliefs and objectives.
Staying abreast of the most recent treatments and research can aid healthcare professionals in providing the most current advice and assistance to those who suffer from AIS and Mullerian Agenesis.
Reference Books
Certainly! Here is a list of reference books on various topics that you might find informative and useful:
General Reference:
- “The Encyclopedia of Science” by David Darling – A comprehensive reference covering various scientific topics.
Medicine and Health:
- “Gray’s Anatomy for Students” by Richard Drake and A. Wayne Vogl – A widely-used anatomy reference for medical students and healthcare professionals.
- “Harrison’s Principles of Internal Medicine” edited by Dennis L. Kasper et al. – A renowned textbook on internal medicine.
- “Robbins and Cotran Pathologic Basis of Disease” by Vinay Kumar et al. – A comprehensive text on the pathology of diseases.
- “The Merck Manual of Diagnosis and Therapy” edited by Robert S. Porter and Justin L. Kaplan – A valuable medical reference for diagnosis and treatment.
Psychology and Mental Health:
- “Abnormal Psychology” by Ronald J. Comer – A textbook providing an overview of abnormal psychology.
- “Diagnostic and Statistical Manual of Mental Disorders (DSM-5)” by American Psychiatric Association – The official diagnostic manual for mental health professionals.
Conclusion
Reference books are valuable resources that provide deep knowledge and insight into a broad range of topics. If you’re a student a professional, or an avid reader These books provide an abundance of information to enhance your knowledge and knowledge.
If you’re interested in the fields of science, medicine, history, or philosophy, these reference books are reliable guides on your journey of discovery and knowledge with a wide array of information that continues to inform our understanding of the world.