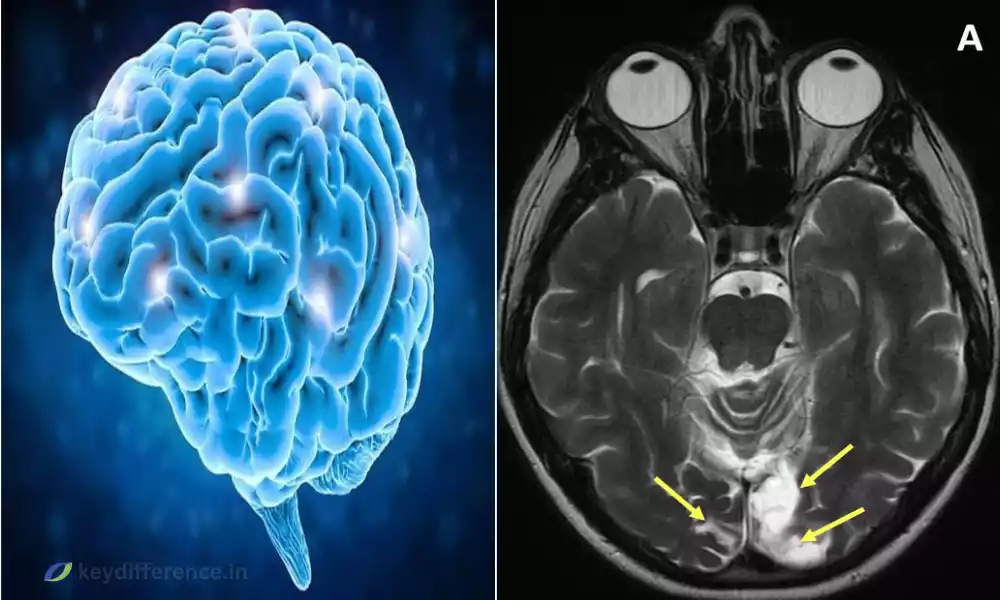
Gliosis and Encephalomalacia are two neurological conditions often caused by brain injuries or diseases, each with its own set of distinctive symptoms and implications for treatment.
Gliosis refers to glial cells responding by producing scar tissue, Encephalomalacia involves softening or loss of brain tissue due to ischemia or trauma.
This article seeks to explore their differences and similarities as well as shed light on causes, symptoms, and management strategies for each.”
Definition of Gliosis
Gliosis is a biological process that occurs in the central nervous system as a response to injuries, infections, or diseases that involve inflammation. Gliosis involves the activation and proliferation of non-neuronal glial cells that provide support and protection for neurons, their proliferation results in dense fibrous networks of tissue called “glial scars.”
Scarring can have both positive and negative ramifications on surrounding neural tissue. On one hand, it helps seal off damaged areas from infection or harmful substances, but excessive scarring could interfere with neural communication and regeneration resulting in long-term functional impairment.
Gliosis remains an active area of research within neurobiology and medicine.

Definition of Encephalomalacia
Encephalomalacia is the medical term for softening or degeneration of brain tissue. This condition may result from various causes, including lack of blood supply (ischemia), bleeding (hemorrhage), infection, or trauma to the head. Softening occurs due to necrosis or death of brain cells in affected regions resulting in decreased function in those areas.
Encephalomalacia can be divided into various subcategories depending on its cause or location within the brain. Polioencephalomalacia affects only grey matter while Leukoencephalomalacia involves white matter structures.
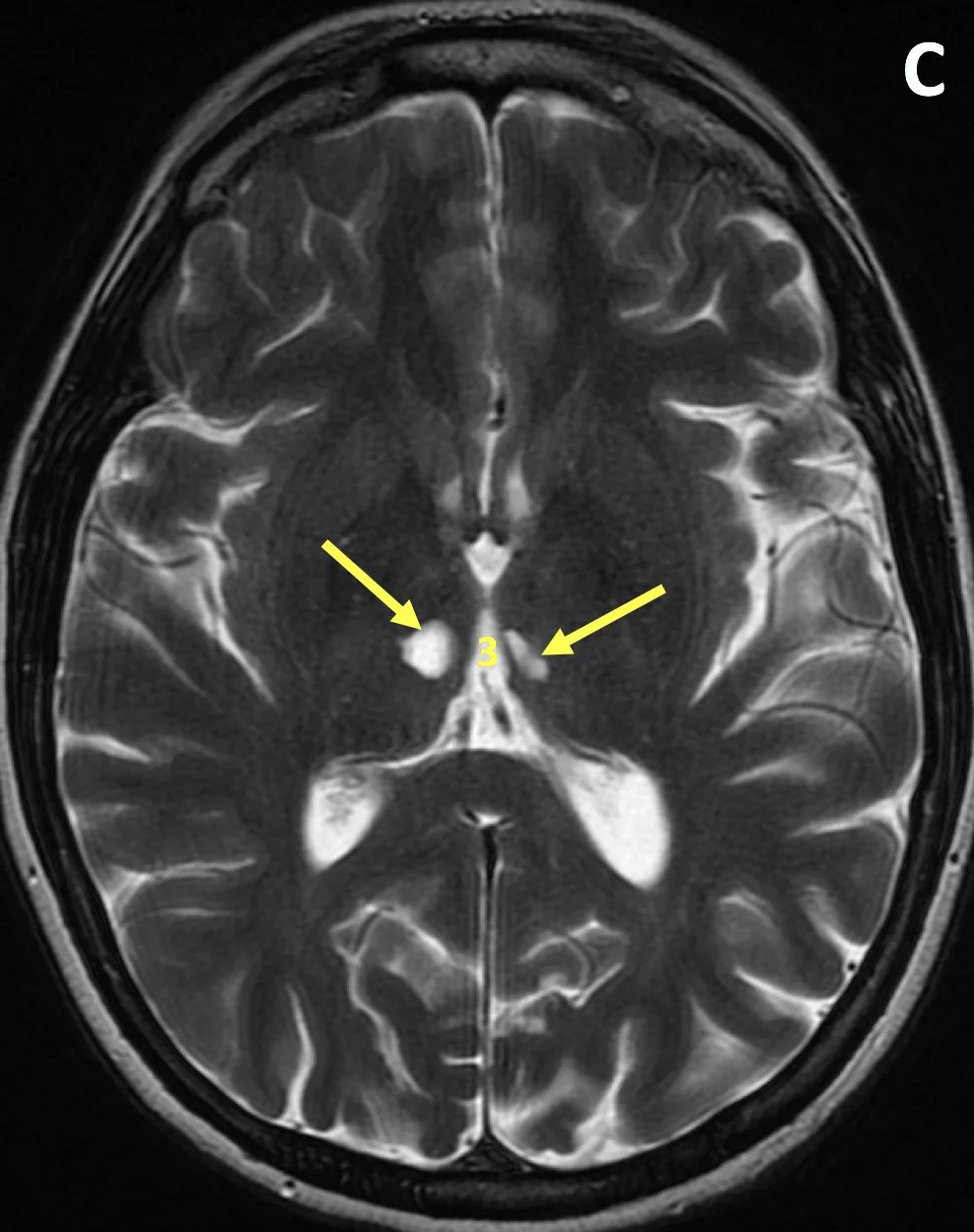
Encephalomalacia may present with various symptoms depending on its location, including cognitive impairments, motor dysfunction, or seizures. Diagnosis often requires imaging techniques like MRI or CT scans.
While treatment attempts to address both its underlying cause as well as any resultant neurological deficits.
Understanding encephalomalacia is vital in neurology, as its proper diagnosis and management can have profound effects on the quality of life and long-term prognosis of affected patients.
Comparison Table of Gliosis and Encephalomalacia
Certainly! Below is a comparison table that outlines the differences and similarities between Gliosis and Encephalomalacia:
| Aspect | Gliosis | Encephalomalacia |
|---|---|---|
| Definition | Reactive response of glial cells leading to scar formation. | Softening or degeneration of brain tissue due to various causes. |
| Causes | Injury, infection, disease, neurodegeneration. | Ischemia, hemorrhage, infection, trauma. |
| Affected Cells | Glial cells (astrocytes, microglia, etc.). | Neuronal cells and surrounding tissue. |
| Symptoms | May be asymptomatic or contribute to neurological dysfunction. | Cognitive impairments, motor dysfunction, seizures. |
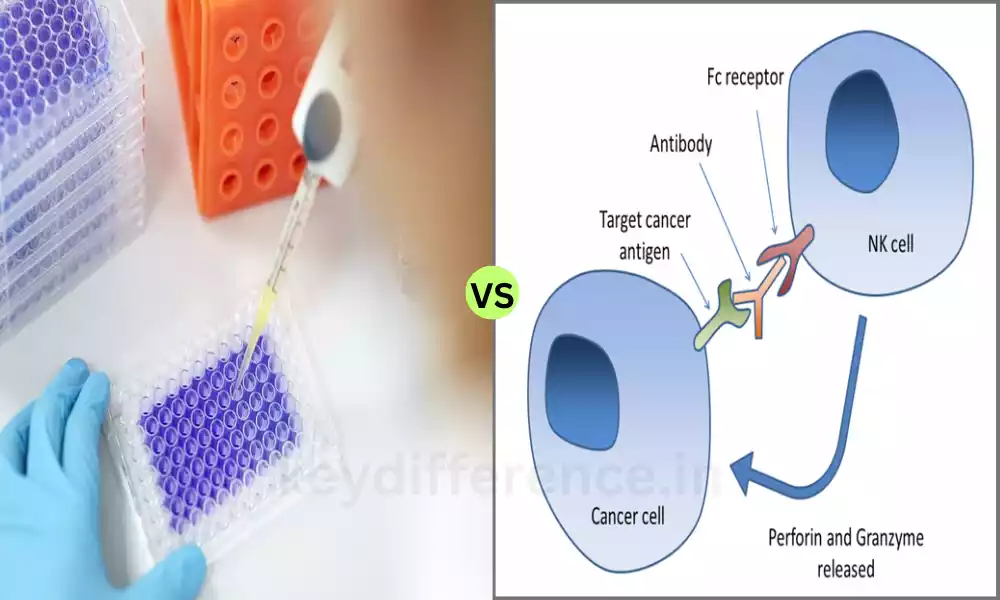
| Diagnostic Tools | MRI, CT scan, histological examination. | MRI, CT scan, clinical evaluation. |
| Treatment | Addressing underlying cause, symptomatic treatment. | Treatment of underlying cause, management of symptoms. |
| Long-term Effects | Can lead to chronic inflammation and hinder neural regeneration. | Permanent loss of function in affected areas, disability. |
This table offers a concise overview of the key aspects of Gliosis and Encephalomalacia, enabling readers to quickly understand the main differences and similarities between the two conditions.
It covers aspects such as definition, causes, affected cells, symptoms, diagnostic tools, treatment, and long-term effects.
Common diseases associated with Gliosis
Gliosis is a reaction of the central nervous system to various forms of injury, disease, or abnormality; it may occur as a result of several diseases:
Multiple Sclerosis (MS): MS is characterized by inflammation leading to demyelination and subsequent gliosis that leads to plaques or scars on nerve fibers, leading to damage and eventually disability in some victims.
Alzheimer’s Disease: Gliosis can often be observed in Alzheimer’s patients’ brains, particularly near amyloid plaques, reflecting an ongoing inflammatory response.
Stroke: After experiencing an ischemic stroke, gliosis is often part of the recovery and scarring process for affected brain tissues.
Traumatic Brain Injury (TBI): After trauma to the brain, gliosis may develop as part of the body’s response to repair damaged tissues and isolate injuries.
Epilepsy: Gliosis may play a part in the pathophysiology of some forms of epilepsy by appearing near where seizures originate, potentially adding another element to its causes and progression.
Gliomas and Brain Tumors: Gliosis can often be observed surrounding gliomas, reflecting their body’s reaction to abnormal cell growth.
Parkinson’s Disease: Parkinson’s disease has been linked with gliosis occurring in specific parts of the brain and contributing to neurodegeneration processes.
Gliosis in Response to Infections of the Central Nervous System: Gliosis is often observed after infection with viruses such as HIV, neurosyphilis, or viral encephalitis as the body attempts to combat and contain it.
Metabolic Disorders: Leigh’s disease and other metabolic conditions that impact the brain may lead to gliosis.
Developmental Disorders: Gliosis may be linked with developmental conditions like cerebral palsy or congenital malformations.
Gliosis should not be treated as an illness in itself but as an outcome of various underlying conditions, and understanding its patterns and implications may provide insights into their nature and severity.
Common diseases associated with Encephalomalacia
Encephalomalacia refers to the softening or degeneration of brain tissue and can be caused by various diseases or conditions, including:
Stroke: An ischemic stroke may reduce blood flow to certain regions of the brain, resulting in softening or necrosis of its tissues – known as Encephalomalacia.
Traumatic Brain Injury (TBI): Trauma to the head can result in bleeding and damage to brain tissue, potentially leading to Encephalomalacia in affected areas.
Brain Infections: Abscesses, encephalitis, or meningitis infections can result in localized softening and damage to brain tissue caused by inflammation and damage.
Brain Tumors: Tumor growth or its treatment may cause Encephalomalacia in surrounding tissues.
Cerebral Hemorrhage: Bleeding within the brain can result in damage and softening of its surrounding tissue.
Hypoxic-Ischemic Injury: Conditions that reduce oxygen and blood supply, such as birth injuries or cardiac arrest, can result in Encephalomalacia.
Chronic Hydrocephalus: When left untreated, hydrocephalus’ increased pressure can cause the brain tissue to soften over time and necessitate softening treatments to soften it further.
Metabolic Disorders: Hepatic Encephalopathy can lead to degenerative changes in the brain that eventually result in Encephalomalacia.
Toxic Exposure: Carbon monoxide poisoning, for instance, can lead to Encephalomalacia.
Degenerative Diseases of the Brain: Certain degenerative conditions affecting the brain may result in softening of brain tissue, leading to softening.
Encephalomalacia is often the result of various underlying conditions, depending on which areas are affected and their degree, its manifestations, and treatment may vary accordingly. Understanding what causes Encephalomalacia is key to effective care for those affected.
How they can both be linked to brain injury or disease
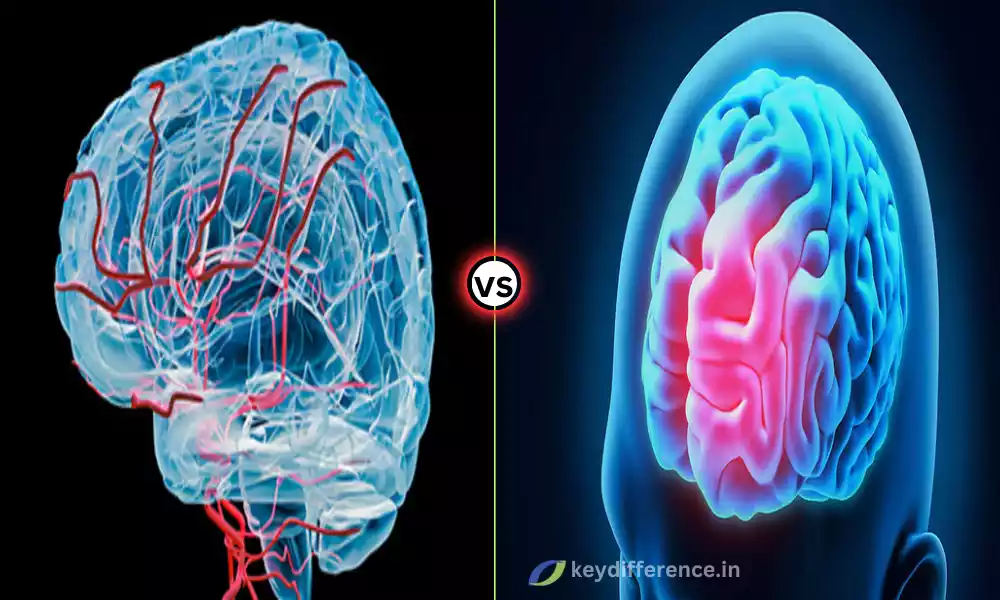
Gliosis and Encephalomalacia can both be caused by brain injury or disease, representing distinct pathologies within the central nervous system.
Here’s how these conditions relate:
Gliosis:
Brain Injury: Following traumatic brain injury (TBI), glial cells proliferate to form scar tissue around injured tissues, providing protection and contributing to healing processes. This action serves to isolate injured tissues while at the same time contributing to healing efforts.
Neurodegenerative Disorders: Prolonged neurodegenerative illnesses like Alzheimer’s or Multiple Sclerosis may result in the brain responding by producing more gliosis as a way of protecting itself against damage or inflammation.
Gliosis Can Occur in Response to Infection or Inflammation in the Brain: Gliosis may form in response to infections or inflammation within the brain when glial cells act to seal off affected areas using their protective barrier function.
Encephalomalacia:
Brain Injuries: Encephalomalacia can occur after severe brain trauma, where physical damage leads to softening or degeneration of brain tissue. This may happen following trauma, stroke, or hemorrhage.
Chronic Conditions: Long-term diseases, like brain tumors or hydrocephalus, can put pressure on or disrupt the flow of blood through regions affected by them and soften affected regions over time.
Infections: Brain infections can also contribute to Encephalomalacia as inflammation occurs within its tissues before degeneration occurs over time.
Common Elements:
Underlying Causes: Both conditions may result from trauma, stroke, or infections that lead to softening and loss of brain tissue – with Gliosis acting as a reactive process and Encephalomalacia marking actual softening and loss.
Gliosis and Encephalomalacia: Gliosis and Encephalomalacia both present as responses to brain damage, however, each manifests differently. Gliosis forms scars that impede neural communication while Encephalomalacia leads to functional decline within affected areas.
Therapeutic Considerations: Understanding both conditions in relation to an underlying brain injury or disease is vital in order to provide accurate diagnosis, treatment, and management for those affected.
Gliosis and Encephalomalacia are two interrelated responses to brain injury or disease, offering insight into its nature and extent. A proper understanding of them is central to effective therapy treatment plans.
Implications for patient care and clinical practice
Gliosis and Encephalomalacia have far-reaching ramifications for patient care. Their management is crucial in providing care to those affected by brain injuries or diseases, here’s how these conditions impact care:
1. Diagnosis and Evaluation:
Imaging: Imaging can provide invaluable information about Gliosis or Encephalomalacia, whether the cause lies within trauma, infection, stroke, or another chronic condition.
Clinical Assessment: Symptoms will differ depending on the location and extent of Gliosis or Encephalomalacia, thus requiring comprehensive neurological exams.
2. Treatment and Management:
Addressing the Underlying Cause: Treatment plans must address the underlying cause, whether that means controlling infection, managing inflammation, or treating tumors.
Rehabilitative Therapies: If Encephalomalacia results in functional decline, rehabilitation therapies such as physical, occupational, or speech therapy may be required for rehabilitation purposes.
Monitoring: To detect changes or progression of this chronic condition, regular monitoring may be necessary.
3. Prognosis and Long-Term Care:
Understanding the Prognosis: Both conditions can have significant ramifications on prognosis, both patients and caregivers should be informed about the potential outcomes of any treatments they undergo.
Long-Term Assistance: Chronic conditions often necessitate long-term support, from assistance with daily living activities to professional nursing services.
4. Preventive Measures:
Secondary Complications: It is essential that steps be taken to prevent secondary complications that might worsen your conditions, such as further injuries or managing coexisting medical issues.
Lifestyle and Medication Management: In some instances, lifestyle or medication changes can help in the prevention or management of conditions or ailments.
5. Psychosocial Considerations:
Its Emotional Support: Gliosis and Encephalomalacia may have serious repercussions for their patients and their loved ones, necessitating psychological support both from outside sources as well as those inside.
Education: Education is of vital importance in managing medical conditions. Healthcare providers must remain up-to-date on current research findings and best practices related to such conditions in order to remain up-to-date with the latest research findings and practices related to them.
6. Collaboration for Comprehensive Care: Partnering between neurologists, therapists, surgeons, and other specialists can offer holistic solutions.
Gliosis and Encephalomalacia are complex conditions with far-reaching implications for patient care and clinical practice.
A multidisciplinary approach, with emphasis on accurate diagnosis, tailored therapy plans, and compassionate care is required in order to manage them successfully.
Reference Books
Certainly! Here are some reference books that might be useful for those looking to understand more about Gliosis, Encephalomalacia, and their implications in patient care:
For General Neurology:
- “Adams and Victor’s Principles of Neurology” by Allan H. Ropper, Martin A. Samuels, Joshua Klein
- “Bradley’s Neurology in Clinical Practice” by Robert B. Daroff, Joseph Jankovic, John C. Mazziotta, Scott L. Pomeroy
For Neuropathology:
- “Greenfield’s Neuropathology” by Seth Love, Arie Perry
- “Neuropathology: A Volume in the Series: Foundations in Diagnostic Pathology” by Richard A. Prayson
For Neuroimaging:
- “Osborn’s Brain: Imaging, Pathology, and Anatomy” by Anne G. Osborn
- “Textbook of Clinical Neurology” by Christopher G. Goetz
Conclusion
Gliosis and Encephalomalacia are distinct yet interrelated neurological phenomena that manifest themselves after experiencing various forms of brain injury or disease. Gliosis represents a protective, scarring response while Encephalomalacia indicates softening and degeneration of brain tissue.
Both conditions demonstrate how complex brain injury reactions can be, both conditions may result from trauma, stroke, infection, or chronic degenerative conditions as potential sources for these neurological phenomena.