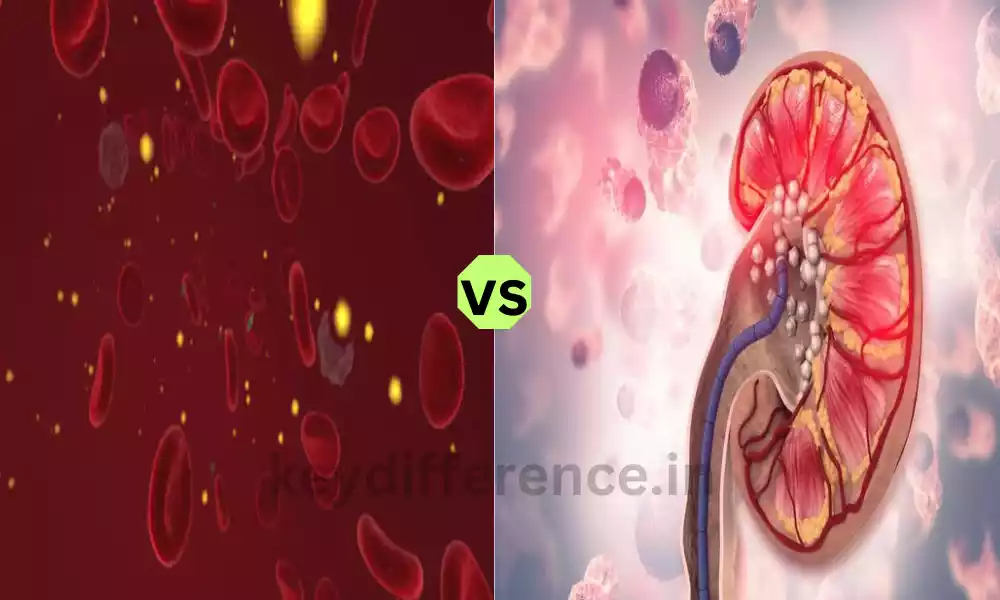
The two medical disorders are that are characterized by elevated amounts of calcium or oxalate within the body as well as in the blood. Although they have similar signs and symptoms, understanding the differences between them is essential for a correct diagnosis and effective treatment.
The differences between Hypercalcemia and Hyperoxaluria in terms of their causes as well as clinical manifestations diagnosis methods, and treatment options, stressing the importance of accurate identification and treatment for each of the conditions.
Hypercalcemia
The medical term “hypercalcemia” refers to an issue that is characterized by high levels of calcium in the bloodstream over what is normal. The normal range of blood calcium levels ranges from 8.5 to 10.2 milligrams per deciliter (mg/dL) or 2.12 to 2.55 millimoles per liter (mmol/L).
Hypercalcemia could be the result of a myriad of reasons, including hyperparathyroidism which is a secondary and primary malignancy, a high intake of calcium, and other health conditions that impact the metabolism of calcium.
This condition may cause various signs and symptoms, which can affect different organ systems of the body. These conditions might require specific tests and treatments in order to identify the root cause of the problem and to manage the increased levels of calcium.

Hyperoxaluria
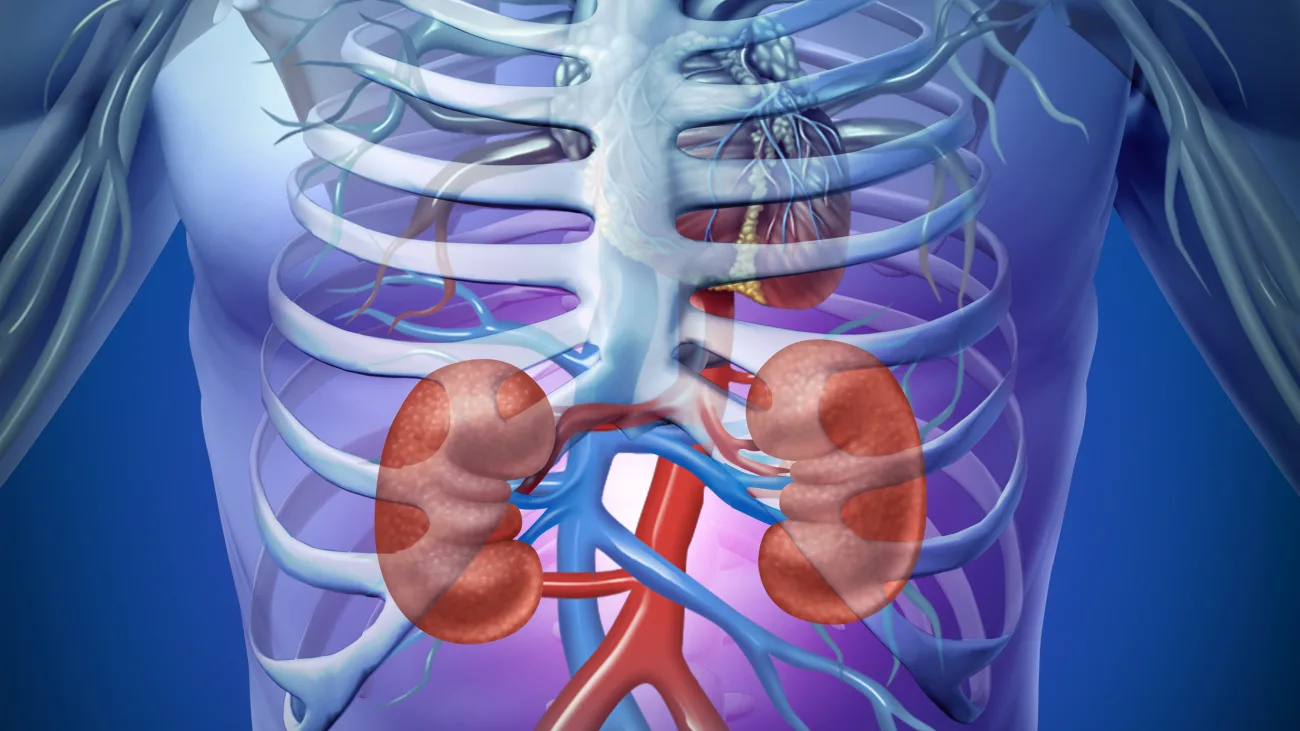
Hyperoxaluria is a condition caused by an excess accumulation of oxalate in urine, resulting in elevated levels of oxalate within the body. Oxalate is an organic waste product, which is cleared from your body via the kidneys.
There is an increase in the amount the oxalate that is excreted from the urine. The condition is classified as secondary and primary hyperoxaluria. The former is an uncommon genetic disorder, and secondary hyperoxaluria is correlated with many underlying causes like dietary causes or a medical condition.
The high levels of oxalate present in urine can lead to kidney stones. They could be painful and result in kidney damage if not controlled. The treatment of hyperoxaluria usually involves diet changes, increased intake of fluids, and, in some instances, medicines that reduce the absorption of oxalate or boost the excretion.
Finding and treating the cause of the problem, if necessary, is essential in addressing the issue of hyperoxaluria.
Importance of distinguishing between Hypercalcemia and Hyperoxaluria
Differentiating between hypercalcemia and hyperoxaluria is essential for many reasons:
- Accurate diagnosis and treatment: Both hypercalcemia and hyperoxaluria have different reasons, symptoms, and treatment options. Incorrect diagnosis or confusion among the two conditions could lead to unsuitable or ineffective treatments and may lead to a worsening of the underlying problems.
- Different causes underlying it: Hypercalcemia often results from problems with calcium metabolism, including hyperparathyroidism, or cancers of a certain kind while hyperoxaluria can be genetically based or caused by diet or other factors. The identification of the root source is vital for proper treatment.
- Symptomatic Variations: Hypercalcemia primarily presents with symptoms relating to calcium imbalance, which can affect nerves, the gastrointestinal system, and kidneys. Hyperoxaluria on the other side, is linked to kidney stones, as well as damage to the kidneys. Understanding these differences can aid in managing symptoms.
- Methods of Treatment: Hypercalcemia treatment involves treating the root reason, the medication, and lifestyle adjustments while management of hyperoxaluria focuses on diet changes, increasing fluid intake, and medicines to lower the absorption of oxalate. An accurate diagnosis can ensure that the correct treatments are implemented.
- Preventing Complications: Both of these conditions could result in complications if untreated. Hypercalcemia could lead to bone and kidney stones as well and hyperoxaluria could cause damage to the kidneys. A prompt diagnosis and proper management can prevent the occurrence of these problems.
- Prognosis: The distinction between hyperoxaluria and hypercalcemia is crucial to know the long-term prognosis. An accurate diagnosis enables healthcare professionals to give patients realistic expectations regarding the prognosis and lifestyle adjustments.
Knowing the difference between hypercalcemia as well as hyperoxaluria is crucial to providing the appropriate medical treatment, avoiding complications, and providing an improved quality of life for those suffering from these ailments.
Comparison Table of Hypercalcemia and Hyperoxaluria
Here’s a comparison table highlighting the key differences between hypercalcemia and hyperoxaluria:
| Aspect | Hypercalcemia | Hyperoxaluria |
|---|---|---|
| Definition | Elevated blood calcium levels | Excessive oxalate in urine |
| Normal Range (Adults) | 8.5 to 10.2 mg/dL | Varies, but typically less than 40 mg/day |
| Underlying Causes | – Primary hyperparathyroidism – Secondary hyperparathyroidism – Malignancies – Excessive calcium intake – Certain medical conditions | – Primary hyperoxaluria (genetic) – Secondary hyperoxaluria (dietary factors, medical conditions) |
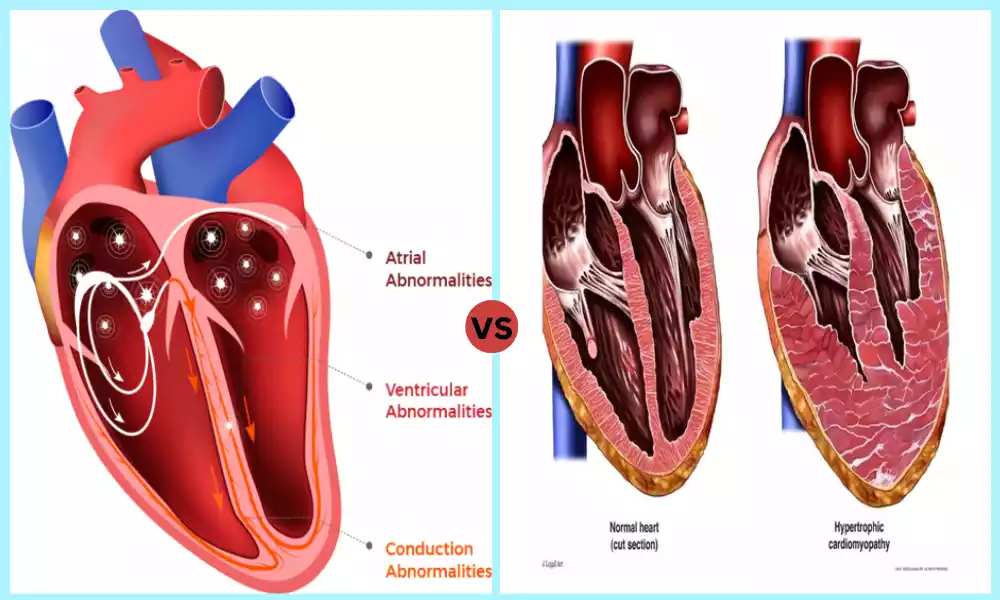
| Clinical Symptoms | Nervous system and muscular manifestations, gastrointestinal symptoms, kidney-related symptoms | Kidney stone formation, renal damage |
| Common Complications | Kidney stones, bone issues | Kidney damage, nephrocalcinosis |
| Diagnostic Methods | Blood tests to measure calcium levels, identification of underlying causes | Urinalysis for oxalate levels, genetic testing for primary hyperoxaluria |
| Treatment Strategies | Address underlying causes, medications, and lifestyle modifications | Dietary modifications, increased fluid intake, medications to reduce oxalate absorption |
| Prognosis and Management | Depending on the underlying cause and early intervention; long-term management may be required | Genetic and dietary factors play a significant role; ongoing management is essential |
This comparison table summarizes the key distinctions between hypercalcemia and hyperoxaluria, including their definitions, causes, clinical symptoms, complications, diagnostic methods, treatment strategies, and the importance of long-term management.
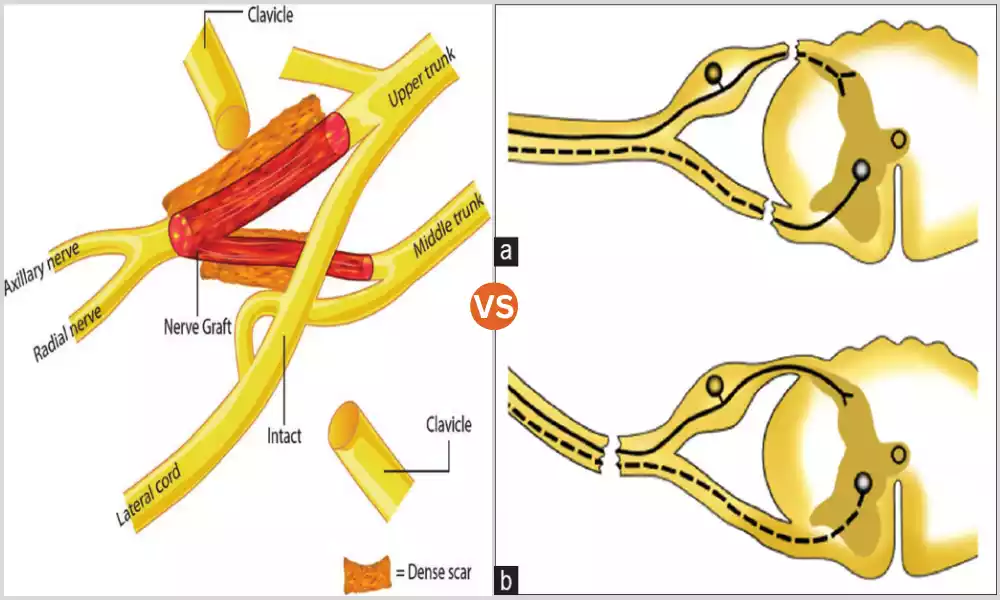
Nervous system and muscular manifestations
The muscular and nervous systems are the symptoms and their effects on the musculoskeletal and nervous systems that are common in people suffering from hypercalcemia, a medical condition that manifests itself as increased levels of calcium within the bloodstream. The symptoms are caused by the effect of excessive calcium on a variety of biological processes. The muscle and nervous system manifestations of hypercalcemia are:
- Neuromuscular Irritability: The elevated levels of calcium can cause increased excitability in muscles and nerves. This can cause symptoms like muscle cramping, twitching, and spasms.
- Muscle Weakness: In the most severe circumstances of hypercalcemia, weakness in the muscles can be observed, which can affect a person’s ability to move and carry out everyday activities.
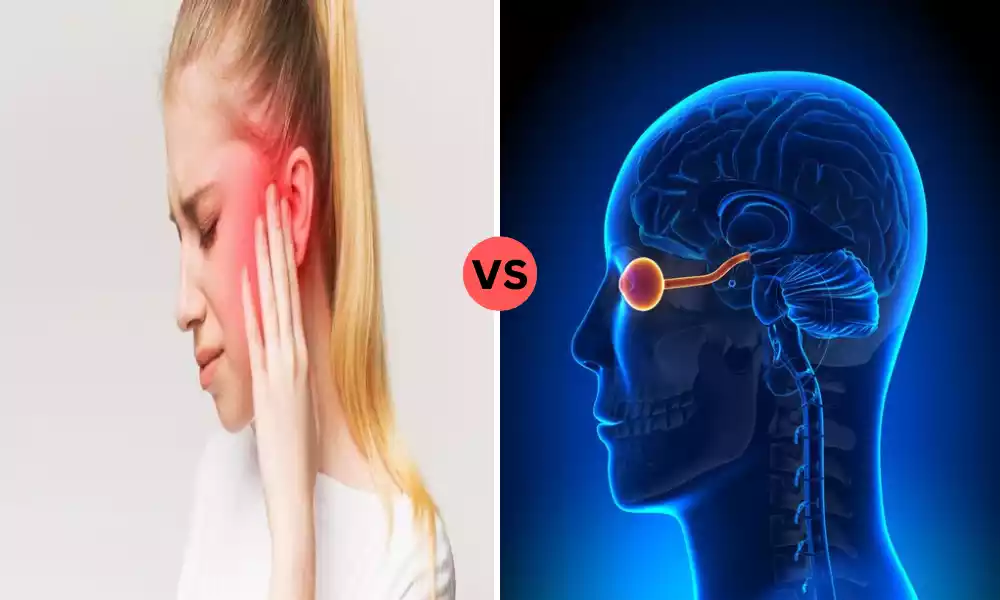
- Cognitive and Confusion: High calcium levels may affect brain function, causing confusion, memory issues, and changes in cognitive abilities.
- Depression and Changes in Emotion: Some individuals with hypercalcemia can experience mood changes which include depression as well as emotional instability.
- Nerve-related Symptoms: Increased levels of calcium cause peripheral nerves to be affected and cause symptoms like tingling, the sensation of numbness, and more severe neurological symptoms such as seizures.
- Coma: When there are severe hypercalcemia cases this can cause an uncontrollable neurological impairment.
It’s crucial for healthcare professionals to be aware of these muscle and nervous system signs in people suffering from hypercalcemia for proper treatment and control of the root causes which could include issues like primary hyperparathyroidism as well as certain cancers.
Treatment generally involves addressing elevated calcium levels, typically with medications, as well as addressing the condition that is causing it.
Medications and lifestyle modifications
Lifestyle and medication are crucial to treatment and treatment of a variety of medical conditions, such as hypercalcemia and hyperoxaluria.
Below, I’ll discuss the common medication and lifestyle changes that are that are associated with each of the conditions:
Medications for Hypercalcemia:
- Bisphosphonates: These are drugs like alendronate or zoledronic acid that help to reduce bone calcium release, thus dropping the level of blood calcium. They are frequently utilized to treat hypercalcemia that is caused by conditions such as primary hyperparathyroidism.
- Calcitonin: Calcitonin helps reduce blood calcium levels by reducing the resorption of bone. However, its effects last only a few hours and are less potent than bisphosphonates.
- Hydration: Intravenous (IV) fluids, including solutions containing saline, are given to stimulate diuresis and remove excess calcium from the body.
- Corticosteroids: Sometimes corticosteroid medication can be prescribed to decrease inflammation and decrease calcium levels.
- Parathyroid Hormone (PTH) Analogs: These medications can be used to treat specific forms of hypercalcemia, by replicating the actions of PTH which regulates calcium levels.
Lifestyle Modifications for Hypercalcemia:
- Dietary Changes: Limiting the consumption of foods with high calcium content including dairy products and the consumption of calcium supplements is generally suggested.
- Hydration: Consuming plenty of fluids specifically water, can aid in increasing the excretion of calcium from the urinary tract.
- Weight-Bearing Training: Engaging in exercises that require weight will help maintain bones’ health and help counteract the negative effects of hypercalcemia on bones.
- Limit sun exposure: In the case of the granulomatous disease (e.g. sarcoidosis) that is associated with hypercalcemia the reduction of sun exposure may lower the chance of the production of calcium through the skin.
Medications for Hyperoxaluria:
- Therapeutic Pharmacology: Based on the nature and the cause of the hyperoxaluria, medicines may be prescribed to decrease the absorption rate of oxalate into the intestinal tract. This may include drugs such as calcium citrate that binds the oxalate and decreases the absorption of it.
- Vitamin B6 (Pyridoxine): Vitamin B6 supplementation can be beneficial in the treatment of certain forms of primary hyperoxaluria.
- Dietary Supplements Calcium supplements can help bind Oxalate within digestion, thus reducing the absorption of calcium. But, this should only be carried out under the supervision of a medical professional.
Lifestyle Modifications for Hyperoxaluria:
- Dietary Changes: Limiting or avoiding the consumption of foods that contain oxalates, like rhubarb, spinach beets, beets, and some nuts, is vital. The diet changes should be adapted to the specific type of hyperoxaluria.
- Hydration: drinking plenty of fluids will help dilute the Oxalate in urine and lower the chance of kidney stones forming.
- Restricting vitamin C supplements: Vitamin C supplements may be converted to Oxalate within the body. Avoiding or reducing the intake of excessive vitamin C supplements may be required.
- Monitors Regularly: Patients suffering from hyperoxaluria may require regular monitoring of the levels of oxalate in the urine as well as kidney function.
These medications and lifestyle adjustments are specifically designed to meet the requirements of patients suffering from hypercalcemia or hyperoxaluria. These medications must be prescribed as well as administered by medical professionals based on specific cases and their underlying causes.
High levels of oxalate in the urine
Oxalate levels that are high in urine, also known as hyperoxaluria can cause a variety of health issues specifically related to kidney health as well as the creation of renal stones. Oxalate is a natural chemical found in numerous foods and is also created as waste from the body. For people suffering from hyperoxaluria, the level of oxalate found in urine exceeds the norm.
This can cause a number of health issues:
- Kidney Stone Formation: The most common consequence of hyperprolactinuria is the development of kidney stones. Oxalate may be mixed with calcium in urine to form calcium oxalate crystals. These may aggregate to form kidney stones. They can cause pain and could hinder the flow of urine which can cause various signs.
- The damage to the kidneys: Repeated kidney stone formation and the presence of calcium oxalate crystals inside the kidneys could cause damage to kidney tissues as time passes. This could result in impairment of kidney function, decreased efficiency of filtration, and may result in chronic kidney disease.
- Nephrocalcinosis: In the most severe cases of hyperoxaluria, calcium oxide crystals can build up inside the renal tubules. This condition is called Nephrocalcinosis. This can affect the normal function of kidneys and can lead to renal damage.
- Recurrent Urinary Tract Infections: Kidney stones resulting from hyperoxaluria could be used as a Nidus (starting location) for persistent urinary tract infections which can complicate the clinical picture.
The treatment of hyperoxaluria usually requires dietary changes to decrease the intake of oxalate and increase fluid intake in order to dilute oxalate in the urine, and in some instances, medicines that can decrease oxalate absorption or boost its excretion.
It is essential for those suffering from hyperoxaluria, to work in conjunction with medical professionals to create an individual treatment plan and be monitored regularly to avoid any complications and protect kidney health.
Genetic testing for primary hyperoxaluria
Genetic testing for primary hyperoxaluria is a crucial diagnostic tool to find specific genetic mutations that are associated with the rare disorder. Primary hyperoxaluria is one of the groups of metabolic disorders inherited from the ancestors, that are characterized by the excessive production of oxalate that results in increased levels of oxalate in the body. There are three major types of primary hyperoxaluria namely PH1, PH2, and PH3 which are all caused by mutations in various genes.
Here’s the way genetic testing for primary hyperoxaluria functions:
- Genetic Counseling: In advance of undergoing genetic testing people who suspect they have primary hyperoxaluria or who have an ancestral background of the disorder can receive genetic counseling. This helps both individuals and their families comprehend the ramifications of genetic testing, and help them make an informed decision.
- Sampling: A blood sample or, in some instances the saliva sample is taken from the person who will be examined.
- DNA Isolation: This DNA has been separated from the sample that was collected. It contains genetic information that is required to determine the primary hyperoxaluria-related mutations.
- Genetic Sequencing Genetic testing usually involves DNA sequencing which is the process of determining the exact sequence of DNA’s building blocks (nucleotides) within the genes involved in primary hyperoxaluria.
- Analysis: Once the DNA sequence is established and analyzed, it is then analyzed for specific mutations within genes believed to be linked with primary hyperoxaluria. Genetic tests will determine if there are any disease-causing or pathogenic mutations.
- Interpretation: A genetic counselor or geneticist interprets test results and provides information regarding the mutations that were identified their effects on the health of an individual and the risk of developing primary hyperoxaluria.
- Planning and Counseling: Based on the results, patients as well as their healthcare professionals can develop suitable treatment and management strategies. For primary hyperoxaluria, the treatment plan can include changes in diet, medication, and preventive measures.
Genetic testing is crucial for cases of primary hyperoxaluria since it not only confirms the diagnosis but aids in determining the precise kind of hyperoxaluria primary (PH1, PH2, or PH3).
This information is vital in determining the best treatment and methods to tackle the genetic causes of the condition. It could also provide the family members who are at risk of having the same mutation.
Similarities Between Hypercalcemia and Hyperoxaluria
The two medical disorders are different, each with distinct causes and primary physiological issues. However, there are a few similarities between them:
- Both affect kidney health: Both hypercalcemia and hyperoxaluria affect kidney health. Hypercalcemia could result in kidney stone formation while hyperoxaluria is an immediate risk factor for kidney stone formation. Kidneys are involved in the removal and processing of the substances (calcium and oxalate) that play a part in the formation of stones.
- Risque of Kidney Stones: There is an increase in the chance of developing kidney stones. Hypercalcemia could cause the formation of kidney stones containing calcium while hyperoxaluria could cause the formation of oxalate-containing kidney stones. Kidney stones may cause similar symptoms, such as flank pain, and hematuria (blood found in urine).
- Kidney damage: If not managed appropriately, both hypercalcemia and hyperoxaluria may cause kidney damage. The repeated development of kidney stones could cause damage to the renal tissue, alter kidney function, and could result in chronic kidney illness in the future.
- Dietary Modifications: To manage both diseases, diet modifications are usually suggested. People with hypercalcemia might need to limit their intake of calcium and those suffering from hyperoxaluria are advised to avoid food items that are high in the mineral oxalate. Both diet changes are designed to decrease the amount of components (calcium and oxalate) that are responsible for stone formation.
- A higher intake of fluid: It is usually recommended to reduce the amount of substances that cause stone formation. Regular hydration can help reduce the likelihood of developing kidney stones in people suffering from hypercalcemia as well as hyperhyperroxaluria.
- Medical Monitoring: Regular monitoring of medical conditions is essential for both conditions to determine the effectiveness of treatment, treat symptoms, and avoid complications. It may include blood and urine tests to measure the levels of calcium and oxalate, as well as other parameters.
While there are some similarities it’s important to recognize that hyperoxaluria and hypercalcemia have distinct causes that are at the root of both, and their primary physiological causes differ.
So, the diagnostic and treatment strategies for these conditions are different. It is crucial to correctly discern between these two conditions in order to provide the appropriate treatment.
Conclusion
Although hypercalcemia and hyperoxaluria do share some commonalities, like their effect on kidney health as well as the risk of developing kidney stones. However, these are separate medical conditions that have different root factors and primary physiological imbalances.
An accurate diagnosis and customized treatment are essential to treat these disorders effectively and avoid complications. Knowing the differences is essential for health professionals as well as those suffering from these diseases to ensure appropriate management and better health.