Thermopoid and thrombus are two distinct but interconnected elements that play an important role in the health of your cardiovascular system. Understanding the fundamental distinctions between them is essential in identifying and managing heart diseases efficiently.
We will explore the definitions, development, and characteristics, the consequences for clinical practice, as well as diagnostic methods for thrombus and atheroma, with a focus on their distinctive characteristics and consequences.
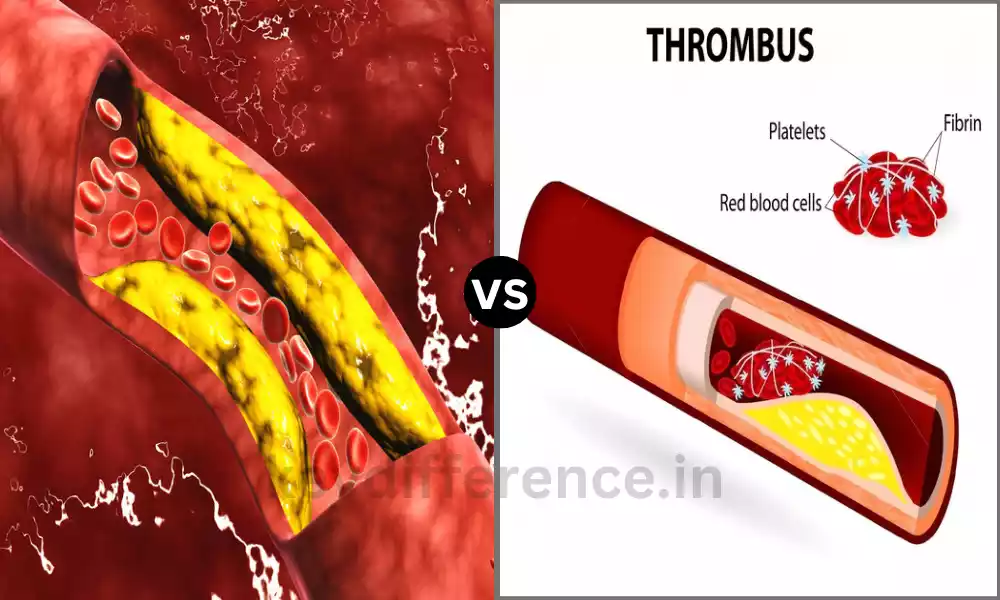
Explanation of Atheroma
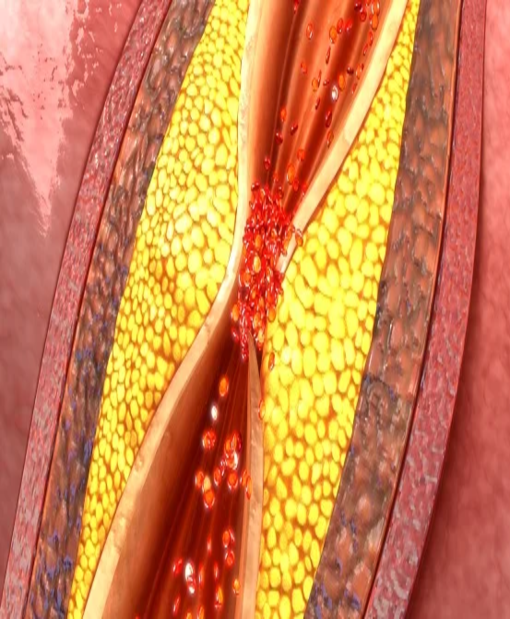
Atheroma refers to the accumulation of fat deposits, particularly cholesterol and lipids, in the lining of arteries. The deposits slowly build up and then form plaques that may cause a narrowing and stiffening of arterial walls.
Atheroma is the most important element of atherosclerosis, which is a progressive and chronic cardiovascular disease that can cause serious health problems, such as strokes and heart attacks.
Atheromas within arterial blood vessels can hinder circulation and raise the chance of clot formation, which contributes to the onset of cardiovascular diseases.
Explanation of Thrombus
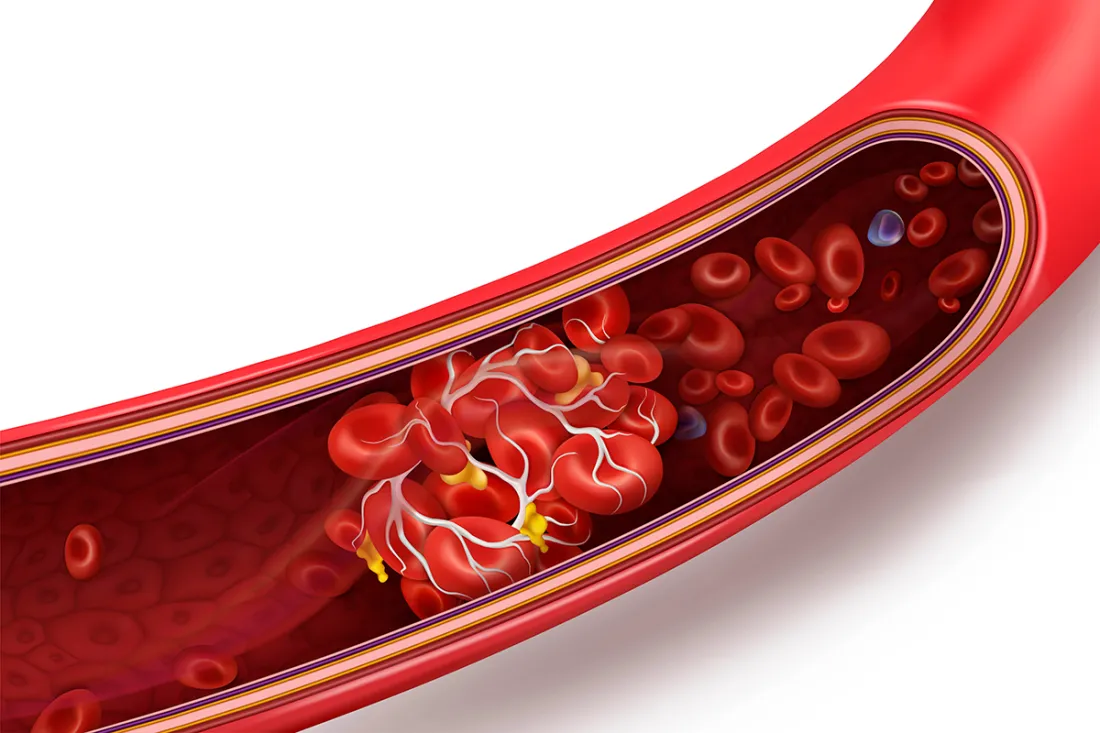
A thrombus can be described as a solid blood clot or mass that develops within blood vessels, which blocks the circulation of blood. Thrombi usually consist of fibrin, platelets, and blood cells that have been trapped They can form in veins or arteries.
The formation of thrombi is a natural reaction to injury and helps reduce excessive bleeding. If thrombi form in blood vessels that are not properly formed, without an underlying injury they could cause serious medical issues, like thrombosis, that may result in blockages or reduced circulation, possibly causing organ dysfunction or damage to the tissue.
Importance of understanding the differences between Atheroma and Thrombus
Understanding the distinction between thrombus and atheroma is vital for a variety of reasons:
- Accurate Diagnosis: Differentiating between atheroma and thrombus is crucial for a precise medical diagnosis. Atheroma is a condition that can last for a long time due to the gradual accumulation of fatty deposits within arteries while a thrombus can be described as an unexpected blood clot that forms. Incorrect diagnosis can result in inappropriate treatment and treatment.
- Treatment selection: Treatment approaches for atheroma and thrombus differ. Atheroma is often treated with long-term care which includes lifestyle changes as well as medication to lower inflammation and cholesterol. Thrombus could require immediate intervention through anticoagulants or thrombolytic drugs. Knowing these distinctions can help health professionals select the most effective treatment.
- Preventive: Knowledge of the root risks and causes of atheroma (atherosclerosis) and the formation of thrombus allows individuals and healthcare professionals to take preventive steps. Lifestyle changes like exercise and diet will reduce risk. Likewise, for thrombus, strategies such as blood thinners could be suggested.
- Complications: Both atheroma and thrombus can cause serious complications if not treated. The atheroma condition can lead to cardiovascular conditions like strokes and heart attacks, while thrombus could create acute blockages in blood vessels, which could lead to injuries to organs or limbs. Knowing the difference helps with the early detection of these complications.
- Educational for Patients: Educating patients about the difference between atheroma and thrombus allows patients to be more aware of their medical conditions as well as treatment options and possible results. This information could lead to greater acceptance of prescribed treatments as well as lifestyle modifications.
- Research and development: A clear distinction between atheroma and thrombus helps researchers to study the mechanisms behind these conditions. This knowledge is vital to creating new treatments, medications as well and interventions to improve the outcomes of patients.
- The Public Health Initiatives: Health campaigns for the public and strategies aimed at reducing the incidence of cardiovascular diseases are based on accurate information regarding atheroma and thrombus. Knowing the distinctions and the underlying causes, policymakers can develop targeted interventions and education programs.
Understanding the difference between atheroma as well as thrombus is crucial to ensure a correct diagnosis, effective treatments, preventative education as well as research and health initiatives aimed towards reducing the effects of cardiovascular disease on people as well as society.
Comparison Table of Atheroma and Thrombus
Here’s a comparison table highlighting the key differences between atheroma and thrombus:
| Aspect | Atheroma | Thrombus |
|---|---|---|
| Definition | Accumulation of fatty deposits in arteries | Solid mass or blood clot within a blood vessel |
| Formation | Gradual buildup over time | Sudden formation, often in response to injury |
| Composition | Cholesterol, lipids, inflammatory cells | Platelets, fibrin, trapped blood cells |
| Location | Typically within arterial walls | Can occur in arteries or veins |
| Characteristics | Plaque buildup, calcification | Solid mass, potential for embolization |
| Clinical Implications | Associated with atherosclerosis and cardiovascular diseases | Can lead to thrombosis and acute ischemic events |
| Diagnosis | Imaging techniques (angiography, ultrasound), blood tests (lipid profiles) | Imaging techniques (CT scan, MRI), blood tests (D-dimer, coagulation studies) |
| Management | Lifestyle changes, medications (statins, anti-inflammatory drugs), invasive procedures (angioplasty, stent placement) | Anticoagulant therapy (heparin, warfarin), thrombolytic therapy, surgery (thrombectomy) |
This table provides a concise overview of the key differences between atheroma and thrombus, including their definitions, formation processes, composition, locations, characteristics, clinical implications, diagnostic methods, and management approaches.
Activation of coagulation factors
The activation of the coagulation factor is an essential process during the blood clotting process Also called hemostasis. These are proteins present in blood that combine to create an unbreakable blood clot after there’s an accident or injury to the blood vessel. This process stops bleeding and aids in wound healing.
Here’s a brief outline of how the coagulation factors work:
- Intrinsic Pathway: This pathway begins when there is damage within blood vessels like endothelial damage. The intrinsic pathway is comprised of several coagulation factors such as IX, XII, and VIII. This sequence comprises an activation process of the factors in the form of a cascade that eventually leads to the activation and release of factor X.
- Extrinsic pathway: It is activated through external injury or trauma that exposes blood vessels to tissue factor (TF) which is a protein that is found outside of the blood vessels. The tissue factor triggers the extrinsic path, which triggers an activation process of factor VII. Factor VII is then associated with tissue factor and stimulates factor X.
- Common Pathway: Extrinsic and intrinsic pathways join at factor X which is the primary element in the pathway common to all. Factor X which is activated (Xa) is combined with factor V as well as other cofactors to form the thrombinase complex. This complex transforms prothrombin (factor II) into the thrombin (factor IIa).
- Thrombin Formation: The Thrombin protein plays a key part in the process of blood clotting. It converts fibrinogen soluble into fibrin strands that are insoluble. The fibrin strands form a web that encases blood cells, forming an unbreakable blood clot.
- Fibrinolysis Regulation: When the clotting process begins the mechanisms to control the formation of clots and stop excessive clotting (thrombosis) are also put into the equation. Anticoagulant substances, such as antithrombin and protein C, regulate coagulation processes to keep a proper balance between the formation of clots and the dissolution of the clot.
- Clot Dissolution: In the end, the clot must dissolve to allow the normal flow of blood. This can be accomplished through the process known as fibrinolysis where plasminogen is transformed into plasmin, an enzyme that breaks down fibrin, which dissolves the clot.
It is important to note that the activation of these factors is closely controlled so that the clotting happens only when there is an injury, and doesn’t lead to unintentional blood vessel clots (thrombosis).
Infections to the coagulation system may cause bleeding problems (hemorrhagic circumstances) or an overly large clot formation (thrombotic conditions) Both of which can be very harmful to health.
Clinical Consequences
The activation of coagulation-related factors in the creation of blood clots can have profound clinical effects, which could be beneficial in stopping excessive bleeding or cause harm if blood clotting is performed in an inappropriate manner. The consequences of this depend on circumstances and the balance between the anticoagulant and procoagulant elements in the body.
Here are the most important medical consequences:
- Hemostasis: One of the most beneficial results of coagulation occurs through hemostasis it is a body’s normal process to stop bleeding whenever blood vessels are damaged. The formation of blood clots stops excessive bleeding and aids in wound healing, which reduces the chance of hemorrhage after an injury or surgical procedure.
- Thrombosis: Excessive or inappropriate activation of coagulation factor can cause thrombosis, which is that is, the creation of blood clots inside blood vessels. It can happen within the arteries (arterial blood clots) as well as veins (venous thrombosis) and can cause various medical conditions, such as:
- Deep Vein Thrombosis (DVT): Clot formation in deep veins, usually in the legs. It may cause swelling and pain, and, if it is dislodged the embolism can cause embolisms in the pulmonary system.
- Pulmonary Embolism (PE): Occurs when a clot that has formed from a DVT or anywhere else in the body moves to the lungs, creating chest discomfort, breath shortness, and, in extreme instances, even death.
- Myocardial infarction (Heart Heart Attack): Arterial thrombosis in coronary arteries could cause a decrease in circulation to heart muscles, which can result in an attack on the heart.
- Ischemic Stroke: Arterial thrombosis within cerebral arteries could cause the blood supply to be cut off into the brain which leads to stroke.
- Arterial Thrombosis: It can cause peripheral artery disease (PAD) or blockages in other arteries, which result in decreased blood flow to organs or limbs.
- Bleeding disorders: The presence of abnormalities or alterations in their regulation may result in bleeding disorders such as hemophilia, von Willebrand’s disease, or thrombocytopenia. These conditions can trigger unintentional bleeding, prolonged bleeding following minor injuries, and bruising that is easy to heal.
- Disseminated intravascular Coagulation (DIC): DIC is a serious condition in which the coagulation system gets overactive, resulting in large-scale clotting throughout your body. The paradox is that this overly clotting can cause the depletion of clotting factors and platelets, leading to bleeding throughout the body and possibly leading to organ failure.
- Anticoagulant Therapy: The clinically-based use of anticoagulants (e.g. Heparin, heparin warfarin, or in-oral anticoagulants) is recommended for patients who are at risk of developing thrombosis. They interfere with the coagulation pathway to stop blood clots from forming, which reduces the chance of heart attack, stroke, and venous blood bleeding.
- Thrombolytic Therapy: In some cases like acute myocardial infarction, or stroke that is ischemic, thrombolytic medicines are prescribed to break down blood clots that are already present and to improve blood flow.
- Diagnostics and Monitoring: Assays for coagulation factors such as prothrombin time (PT) and activated partial thromboplastin times (aPTT) and the International normalized ratio (INR) are essential diagnostic tools that can help determine the status of coagulation and aid in medical decision-making.
Understanding the medical implications of coagulation is vital for healthcare professionals to recognize and treat bleeding disorders and thrombotic diseases efficiently. Achieving a balance in the coagulation system is crucial to ensuring good health and avoiding complications arising from bleeding and bleeding disorders.
Atheroma assessment
Atheroma testing involves a variety of tests and diagnostic methods to assess the extent and presence of plaque atherosclerotic (atheromas) within the arteries. These tests are essential to diagnose cardiovascular disorders and determine the best treatment strategy.
Here are a few common techniques and tests that are used to assess atheroma:
- Health History, and Physical Exam: Healthcare providers start with a comprehensive medical history, which includes the risk factors that can cause problems, such as smoking or having a relative with a history of heart problems as well as high blood pressure as well as high cholesterol. Physical examinations can identify signs of atherosclerosis, for example, peripheral artery diseases (PAD) and carotid artery diseases.
- Lipid Profile: The blood test known as a lipid profile evaluates cholesterol levels, such as high-density lipoprotein (LDL) cholesterol as well as high-density Lipoprotein (HDL) cholesterol and triglycerides. The presence of elevated LDL cholesterol is a major risk factor in atherosclerosis.
- Electrocardiogram (ECG or EKG): An ECG monitors the heart’s electrical activity and detects symptoms of heart ischemia or attack that is caused by atherosclerosis within the coronary arteries.
- Tests for Stress: Stress tests, like exercise stress tests or psychopharmacological stress tests (e.g. with adenosine or dobutamine) are a way to determine any blockages within the coronary arteries, and also test the function of the heart during physical stress.
- Coronary Angiography: This procedure is invasive and involves injecting an anti-inflammatory dye into the coronary arteries, and then taking X-ray pictures (angiograms) to detect any narrowing or blockages in the arteries. It is considered to be the best method to determine coronary atheroma.
- Carotid Ultrasound: It is a non-invasive test for imaging. utilizes high-frequency sound waves to see the carotid veins in the neck. It is able to detect atherosclerotic plaques and evaluate their size and structure.
- CT Angiography (CTA): Computed tomography angiography (CTA) is a non-invasive imaging method that offers precise images of coronary arteries. It allows the evaluation of atherosclerotic plaques as well as the extent of stenosis.
- MRI Angiography: The technique of magnetic resonance makes use of radio waves and magnetic fields to produce photographs of blood vessels. It is able to provide information on atheromas that are found in various arteries which include the carotid as well as renal arterial.
- Scores for Calcium: A coronary calcium scan, also referred to as coronary arterial calcium (CAC) scoring, utilizes the CT scan to determine the presence of calcium within coronary arteries. A high score on calcium is linked to a higher risk of cardiovascular and atherosclerosis events.
- Ankle-Brachial Index (ABI): ABI is a non-invasive test that examines blood pressure levels between the ankles and the arms to evaluate peripheral arterial diseases (PAD) in addition to the possibility of atherosclerosis in the lower extremities.
- Intravascular Ultrasound (IVUS): IVUS is an invasive process used in coronary angiography for obtaining precise images of the interior of the coronary arteries. It gives information on the nature and extent of the atherosclerotic plaques.
- Fractional Flow Reserve (FFR): FFR is a diagnostic test utilized during coronary angiography. It is used to determine the difference in pressure across a narrowing of the coronary artery. It aids in determining the importance of atherosclerotic plaques.
A combination of these evaluation methods, based on clinical indications and risk factors, can help healthcare professionals diagnose atheroma, determine the severity of the condition, and decide on the best treatment option that could include changes in lifestyle, medication, or surgical procedures such as the angioplasty procedure or stent placement.
Treatment and Management
The treatment and treatment of the disease atheroma (atherosclerosis) are focused on reducing the chance for complications as well as improving the health of cardiovascular. The approach to treatment is based upon the degree of condition and the overall health of the patient as well as individual risk factors.
These are the key elements for treatment as well as management:
- Lifestyle Modifications:
- The diet: Encourage a heart-healthy diet that is free of trans and saturated fats and cholesterol as well as sodium. Focus on fruits, vegetables whole grains, protein-rich lean foods, and fish high in omega-3 fats.
- Physical Activity: Encourage regular physical activity and aim for a minimum of 150 minutes of moderate-intensity aerobic exercise and 75 minutes of vigorous-intensity aerobic activity each week, in addition to exercises for strengthening muscles.
- Smoking cessation: Inspire smoking-free living since smoking cigarettes is a major contributor to atherosclerosis as well as cardiovascular disease.
- Controlling Weight: Achieve and maintain a healthy weight with an appropriate diet and regular physical exercise.
- Medications:
- Statins: Statins are prescribed to reduce LDL cholesterol and to reduce inflammation of the arteries.
- Antiplatelet Therapy: Sometimes aspirin or other antiplatelet drugs may be suggested to decrease the chance of blood clots.
- Antihypertensive Drugs: If a patient suffers from elevated blood pressure they should be prescribed antihypertensive medication to lower the blood pressure.
- Diabetic Management: When a person is suffering from diabetes, improve blood glucose control with lifestyle modifications and medication.
- Anti-Inflammatory Medicines: For patients suffering from severe inflammation, you should consider taking medications like anti-inflammatory medications (e.g. aspirin, for example) or other anti-inflammatory medications that are more recent.
- Invasive Procedures: If you have a severe atheroma, with significant arterial shrinkage (stenosis) or plaques that are unstable Invasive procedures are needed:
- Stent and Angioplasty: This procedure involves inflating a balloon within the artery that is narrowed to expand it. Usually, this is followed by the placing of a stent in order to keep the artery open.
- Atherectomy The procedure involves removing plaque from the artery with specialized instruments.
- Coronary Artery Bypass Grafting (CABG): for coronary artery diseases CABG surgery is used to clear blocked arteries by grafting them from blood vessels other than the ones in which they originate.
- Carotid Endarterectomy: If there is a severe carotid artery disease the carotid endarterectomy is a possibility to remove plaques from carotid veins, which reduces the chance of suffering a stroke.
- Second Prevention: Concentrate on prevention of complications, recurrence, and repeat incidences
- Anticoagulants and antiplatelet therapy are prescribed when appropriate to avoid thrombosis.
- Manage and monitor comorbid conditions such as diabetes and hypertension.
- Keep regular appointments for follow-up visits as well as diagnostic tests to evaluate the progress of treatment and evaluate its effectiveness.
- Patient education: Provide education on the importance of following medication, lifestyle changes, and the symptoms of heart disease like chest pain and stroke-related symptoms.
- Cardiac Rehabilitation: For those suffering from significant heart disease cardiac rehabilitation programs may help in improving cardiovascular health, reducing risk factors, as well as providing aid and guidance.
- Psychosocial support: Address psychological factors like anxiety, stress, and depression, since they may increase your risk of developing cardiovascular disease.
The treatment of atheroma is usually long-term and requires an integrated strategy that incorporates the use of medical therapies, lifestyle changes, and, in certain instances, interventional procedures.
Individualized treatment plans need to be designed in conjunction with healthcare professionals to satisfy the needs of the patient and minimize the chance of heart attacks that are associated with atherosclerosis.
Similarities Between Atheroma and Thrombus
Although atheroma (atherosclerosis) and the thrombus are distinct entities, with distinct mechanisms and implications for clinical care, however, they share certain characteristics and impacts on the cardiovascular system.
Here are some of the key differences between thrombus and atheroma:
- Arterial Involvement: Both thrombus and atheroma may occur in the arteries. The most common cause of atheroma is the gradual building up of fat deposits (plaques) inside the arterial wall, whereas thrombus is an abrupt blood clot development that can cause blockage of an artery.
- Blood flow impairment: Both of them can cause impairment to the flow of blood within arteries, though via different mechanisms. Atheroma narrows arteries, limiting blood flow because of plaque accumulation and thrombus blocks the flow of blood when it forms a clot.
- Risque for Ischemia: Atheroma and thrombus may cause an ischemic event. Thermopoiesis can cause long-term reductions in the flow of blood to tissues, resulting in ischemia that develops over time. Thrombus development can lead to sudden ischemic events, like cardiac attacks (coronary blood clots) and strokes (cerebral thrombosis).
- complications: Both conditions have the potential to cause grave complications if not addressed. The progression of the disease can lead to heart diseases, such as coronary artery disease which can cause heart or angina attacks. The thrombosis can cause embolism, infarction, or thrombosis according to the site of its.
- Diagnostic Techniques: Different diagnostic techniques employed to determine the presence of atheroma like angiography, ultrasound as well and CT scans, can be used to determine the formation of thrombuses. These methods can help determine the location, presence, and size of both thrombus and atheroma.
- Therapy Goals: One of the main goals in managing both atheroma as well as thrombus is the prevention of complications and keeping a healthy flow of blood. Although treatment strategies differ, they have an objective that is similar: improving the health of your cardiovascular system.
- Anticoagulation: The use of anticoagulants can prove beneficial in both instances. Although it is typically used to manage thrombus and keep clots from forming Anticoagulants can also be employed in specific situations to decrease the chance of clot formation on atherosclerotic plaques.
It’s important to understand that atheroma and the thrombus are distinct in their reasons, mechanisms, and time frames for development. Atheroma is a chronic disease that is characterized by the gradual build-up of plaques.
While thrombus formation is an instant process that involves the sudden blood components coagulating. Understanding the differences between the two is crucial to ensure a correct diagnosis and proper treatment.
Reference Books
Certainly! Here are some reference books across various genres and topics that cover a wide range of subjects:
Science and Medicine:
- “The Selfish Gene” by Richard Dawkins
- “The Emperor of All Maladies: A Biography of Cancer” by Siddhartha Mukherjee
- “A Short History of Nearly Everything” by Bill Bryson
- “The Immortal Life of Henrietta Lacks” by Rebecca Skloot
- “Sapiens: A Brief History of Humankind” by Yuval Noah Harari
History: 6. “A People’s History of the United States” by Howard Zinn
- “Guns, Germs, and Steel: The Fates of Human Societies” by Jared Diamond
- “The Origins of Political Order” by Francis Fukuyama
- “The Rise and Fall of the Third Reich” by William L. Shirer
- “1491: New Revelations of the Americas Before Columbus” by Charles C. Mann
Literature and Fiction: 11. “To Kill a Mockingbird” by Harper Lee
- “1984” by George Orwell
- “Pride and Prejudice” by Jane Austen
- “One Hundred Years of Solitude” by Gabriel García Márquez
- “The Great Gatsby” by F. Scott Fitzgerald
Philosophy: 16. “Meditations” by Marcus Aurelius
- “The Republic” by Plato
- “The Genealogy of Morals” by Friedrich Nietzsche
- “A History of Western Philosophy” by Bertrand Russell
- “Being and Time” by Martin Heidegger
Conclusion
A carefully selected selection of reference books that span a variety of themes and genres is an asset to both personal development and professional growth. These books provide insight as well as perspectives that aid in our understanding and appreciation of our world. its history and literature, science, and much more.
If you’re looking for intellectual stimulation practical advice, or simply a fascinating tale, the appropriate reference book could be an entry point to a world of inspiration and learning. Start your journey of reading and let these books become your guide in your quest for understanding and personal growth.