Cardiovascular disease is the leading reason for mortality across the globe and a thorough understanding of the distinctions between atherosclerosis and arteriosclerosis is vital in ensuring effective prevention and treatment.
We’ll explore the primary distinctions between these two closely related diseases, and provide a better understanding of their causes, symptoms, and treatment strategies.
Definition of Arteriosclerosis
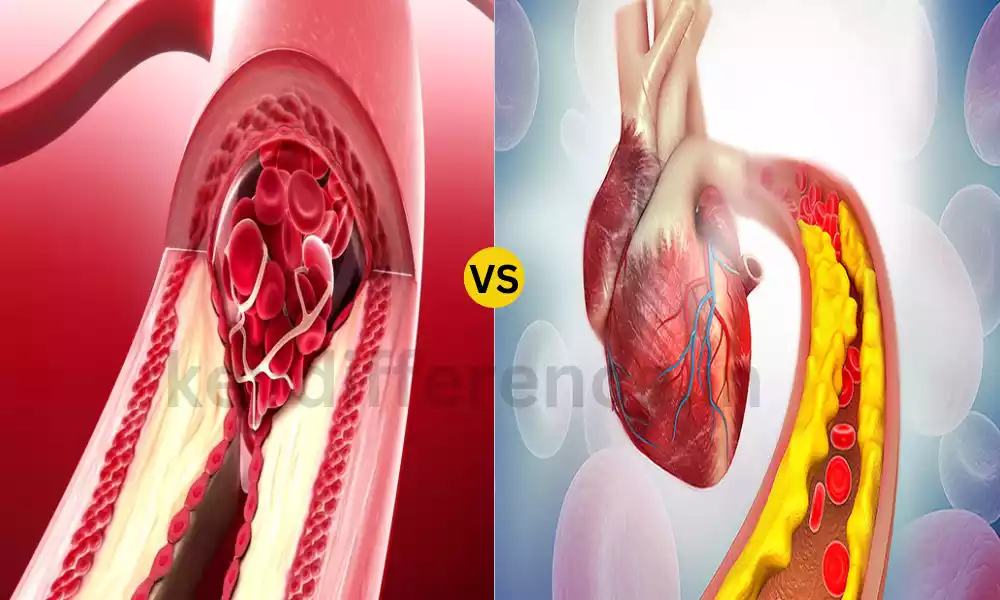
Arteriosclerosis is a term used in medicine that refers to a general thickening and hardening of arteries. It is a condition that progresses and causes the arteries’ walls are weaken, become rigid, and are often surrounded by calcium deposits.
Arteriosclerosis is an umbrella term that includes different types of arterial hardening and thickening and atherosclerosis is one of the most frequent subtypes. This can cause a blockage to circulation and result in numerous cardiovascular issues.
Definition of Atherosclerosis
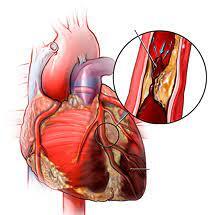
Atherosclerosis is one of the forms of arteriosclerosis, characterized by the gradual accumulation of plaque (atherosclerotic plaque) composed of fatty substances, cholesterol as well as cellular waste products calcium, and various other substances in the inner walls of the arteries.
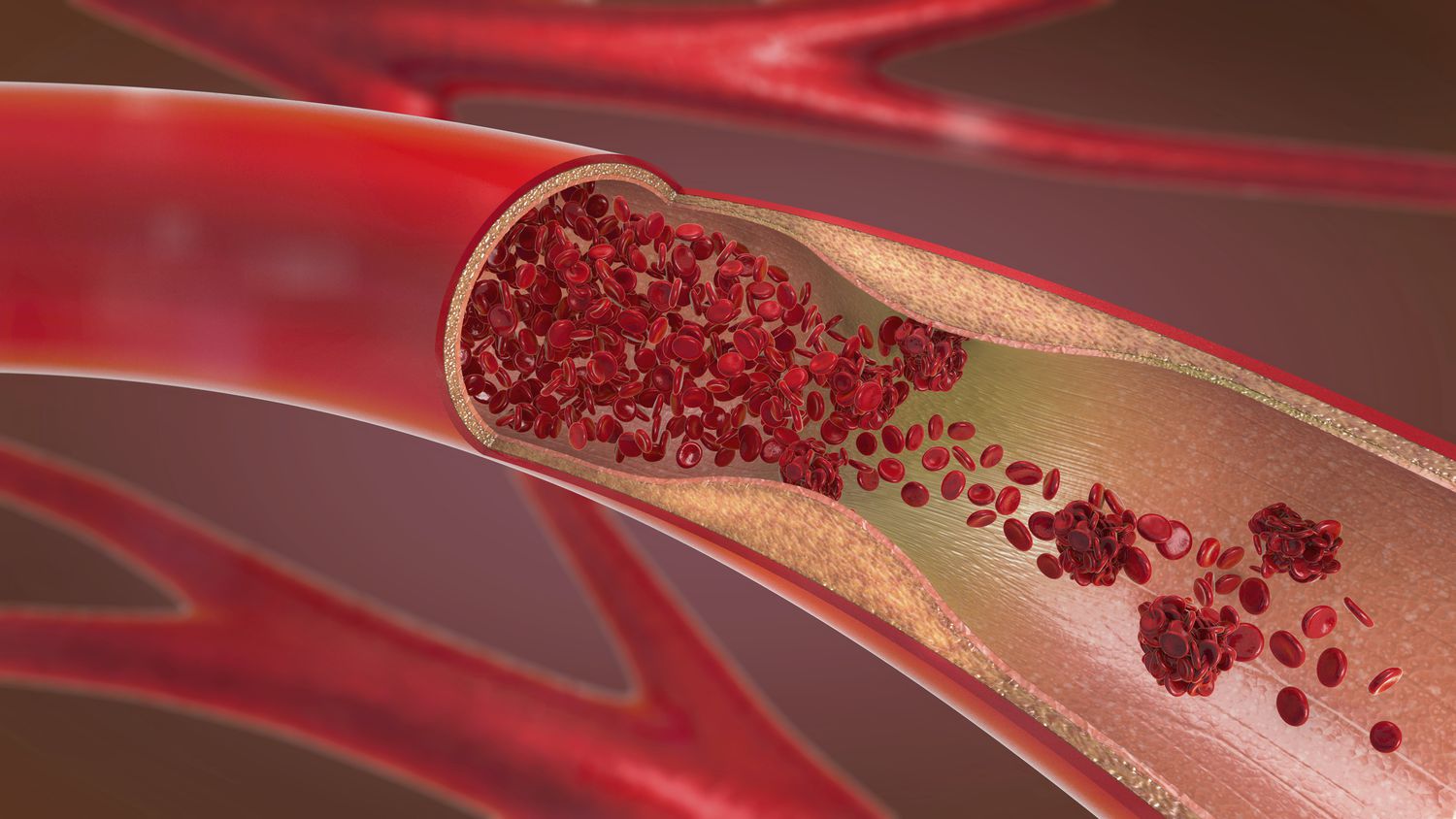
The plaque narrows and hardens the arteries, which reduces the flow of blood and makes them more rigid. In time, atherosclerosis could cause a variety of cardiovascular issues which include stroke, heart disease, and peripheral artery diseases, since it could impede blood flow and cause blood clots to form in affected arteries. It’s a major cause of cardiovascular diseases, which are the leading cause of death in the world.
Importance of understanding arteriosclerosis and atherosclerosis
Understanding the causes of arteriosclerosis and atherosclerosis is vital for a variety of reasons:
- Prevention: Knowing about the conditions can help people take action to change their lifestyles and adopt risk-reduction strategies before they become a problem, which helps to delay or prevent their development. This includes controlling risk factors like hypertension, high cholesterol, smoking, and diabetes.
- Early detection: Recognizing symptoms and signs of atherosclerosis and arteriosclerosis could result in early diagnosis and treatment. This is crucial to stopping serious cardiovascular events like strokes and heart attacks.
- Treatment: Healthcare professionals are able to provide the appropriate treatment options when arteriosclerosis or atherosclerosis is identified. It could involve medications as well as lifestyle changes, and, in some instances surgery. Knowing these conditions will ensure that patients receive the proper treatment.
- Education: Patients who know that arteriosclerosis is a part of atherosclerosis will be more likely to follow their treatment regimens and implement the necessary lifestyle changes. The education of patients allows them to manage their cardiovascular condition.
- Reducing mortality: Cardiovascular disorders such as those relating to atherosclerosis and arteriosclerosis, are the most common cause of death in the world. Knowing about these conditions can aid in reducing mortality through promoting healthy lifestyles and prompt medical intervention.
- Public health impact: The widespread knowledge of arteriosclerosis and atherosclerosis can have a positive effect on the health of the population. This can result in initiatives to promote heart-healthy habits including regular exercise and healthy eating and lower the impact of cardiovascular diseases in healthcare facilities.
- Research and Innovation: An understanding of these conditions can lead to continuous research and development in the area of cardiovascular medicine. This may lead to the advancement of new and more efficient treatments as well as prevention strategies.
Understanding that arteriosclerosis can be a cause of atherosclerosis or arteriosclerosis is vital for both public and individual health. It helps in the early detection, prevention, and treatment of these conditions which ultimately lowers the chance of suffering from cardiovascular illnesses and the complications they bring.
Comparison Table of Arteriosclerosis and Atherosclerosis
Here’s a comparison table highlighting the key differences between arteriosclerosis and atherosclerosis:
| Aspect | Arteriosclerosis | Atherosclerosis |
|---|---|---|
| Definition | Generic term for arterial thickening | Specific type involving plaque formation |
| Types | Various types (e.g., atherosclerosis) | A subtype of arteriosclerosis |
| Primary Cause | Thickening and hardening of arterial walls | Formation of atheromatous plaques |
| Key Risk Factors | Age, hypertension, diabetes, smoking | High cholesterol, smoking, hypertension, diabetes |
| Pathophysiology | Accumulation of calcium deposits, loss of arterial elasticity | Accumulation of cholesterol and fatty deposits, inflammation |
| Symptoms and Effects | Reduced blood flow, increased blood pressure | Narrowing of arteries, increased risk of blood clots |
| Diagnosis | Medical history, physical examination | Lipid profile tests, angiography |
| Treatment Options | Lifestyle changes, medications, surgical interventions | Medications (e.g., statins), lifestyle modifications, surgical procedures (e.g., angioplasty) |
This table summarizes the primary distinctions between these two related conditions, emphasizing their definitions, causes, pathophysiology, symptoms, diagnosis, and treatment options.
Diagnosis and treatment options
Diagnosis of Arteriosclerosis:
- Medical Physical and History Examinations: Healthcare providers assess the risk factors such as age and family background, hypertension, and diabetes. They also monitor for typical symptoms such as a reduced pulse in the joints.
- Imaging techniques: Numerous imaging procedures like angiography, ultrasound, and computed tomography (CT) scans allow you to visualize the walls of arterial vessels and detect areas that are thickening.
Treatment Options for Arteriosclerosis:
- lifestyle changes: The patients are advised to take heart-healthy dietary habits into consideration which include a balanced and healthy diet regular exercising smoking cessation, and the management of stress.
- Medicines: Depending on the root causes and symptoms medication such as antihypertensives or antiplatelet drugs can be prescribed to control blood pressure and to prevent the formation of blood clots.
- Surgical interventions: In severe cases where an arterial blockage may compromise organ function, surgical procedures such as bypass or angioplasty could be needed.
Diagnosis of Atherosclerosis:
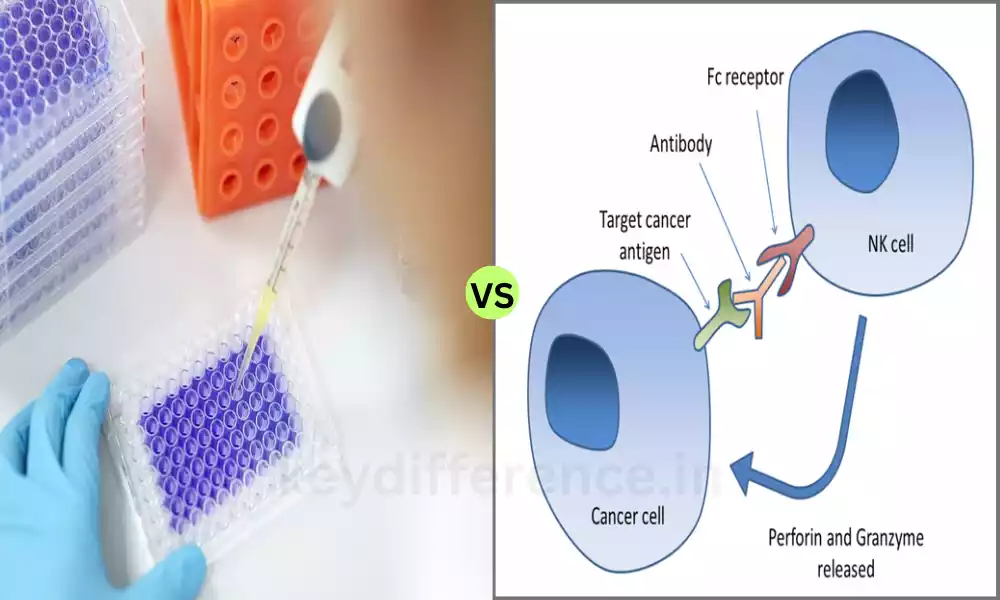
- Testing of Lipid Profile: Blood tests determine cholesterol levels, such as LDL (low-density lipoprotein) and HDL (high-density lipoprotein) that help determine the likelihood of developing atherosclerosis.
- Image Techniques: Techniques such as coronary angiography and carotid ultrasound can reveal the amount of plaque buildup in the arteries.
Treatment Options for Atherosclerosis:
- Medical Treatments (Statins): Statin medications are typically prescribed to reduce cholesterol levels and to slow down the development of atherosclerosis. Other medicines can be prescribed to control blood pressure or to prevent blood clots.
- Lifestyle modifications: The patients are urged to adopt heart-healthy lifestyle modifications which include diet adjustments as well as exercise, weight management smoking cessation, and the reduction of stress.
- Surgery Procedures: Interventional procedures such as angioplasty using stents or coronary bypass grafting (CABG) could be carried out to widen arteries to restore circulation.
- Antiplatelet Therapy: Medications like aspirin or clopidogrel are used to decrease the chance of strokes caused by blood clots.
It is important to remember that the treatment plans for atherosclerosis and arteriosclerosis should be customized based on the individual’s situation, risk factors, and general health. Regularly checking in with your healthcare provider is crucial to keep track of the progress of treatment and modify it according to the need.
Medical history and physical examination
Medical History:
- Data on the Patient: Gather basic demographic information, such as gender, age, as well as the history of your family members with cardiovascular illnesses.
- Previous Medical Histories: Inquire about the medical history of the patient, including any prior heart-related issues and surgeries or hospitalizations.
- Medical Information: Document the current medication, which includes prescription medications, over-the-counter medicines and supplements, because they can affect your cardiovascular health.
- Risk factors: evaluate the risk factors for cardiovascular disease, including smoking habits and alcohol consumption, diet habits, and exercise levels.
- Signs and symptoms: Ask about specific symptoms such as chest pain, breathing problems, shortness of breath dizziness, palpitations and fatigue.
- Family History: Discover the family background of heart disease stroke, heart disease, or other conditions that affect the cardiovascular system, since genetics may play a major part.
- Lifestyle Factors: Consider lifestyle aspects such as diet, exercise routine Stress levels, diet, and sleep patterns to assess their effects on your cardiovascular health.
Physical Examination:
- Blood Pressure: Check the blood pressure of the person to determine hypertension, a risk factor for heart disease.
- Heart Rate and Rhythm: Examine the heart rhythm and rate of the patient in order to find irregularities or arrhythmias.
- Heart Sounds: Pay attention to heart sounds with a stethoscope to detect irregular heart murmurs and sounds that could indicate issues with valvular.
- Peripheral Pulses: Check peripheral pulses like carotid, radial, and femoral pulses to assess the flow of blood through various areas of the body.
- The rate of breathing: Monitor the patient’s respiration rate and effort to look for indications of heart disease or pulmonary problems.
- Edema: Look for swelling (swelling) on the lower extremities. This may be a sign of fluid retention that is related to heart issues.
- Chest Examining: Inspect the chest for any deformities, mass, or indications of injury, and look for signs of chest tenderness or discomfort.
- Abdominal Exam: Palpate the abdomen to look for an increased or tender liver, and also for abdominal aortic aortic aorta aneurysm.
- Neck Exam: Examine the neck for signs of jugular vein venous dilation which could be an indicator of heart insufficiency.
- Brain Assessment: Conduct a short neurological exam to determine any signs of stroke, or neurological problems.
Accumulation of cholesterol and fatty deposits
The build-up of cholesterol and deposits of fatty substances in the arteries is an important element in the development of atherosclerosis, which is a particular kind of arteriosclerosis. This plays a major role in the pathophysiology behind atherosclerosis and may have profound consequences for the health of your cardiovascular system.
Let’s take a closer review of this process:
- Cholesterol and Fatty Deposits:
- Cholesterol is a fatty waxy substance that is necessary for a variety of physiological functions within the body. If there is a high level of cholesterol in the bloodstream it could cause issues.
- Fat deposits, such as cholesterol, as well as other lipids, can build up on the inner liner (endothelium) of arterial blood vessels over time.
- Inflammatory Response:
- As these deposits accumulate they may create an inflammatory reaction within the arterial wall.
- Cells of white blood (macrophages) are redirected to the location of the deposits to try to engulf and break down fats and cholesterol.
- When this happens, immune cells can be overwhelmed and turn into foam cells. They aid in the formation of atherosclerotic plaques.
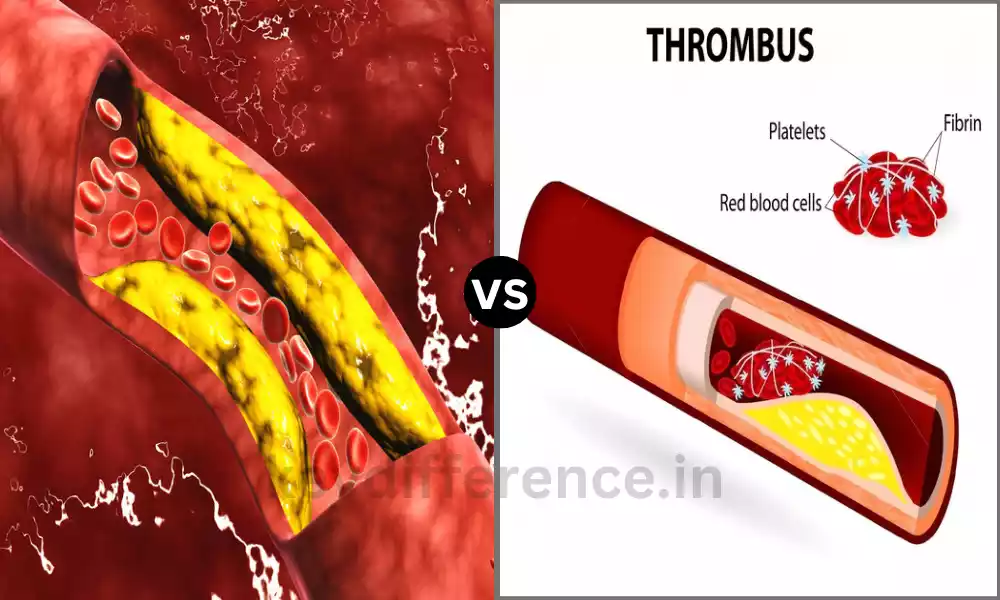
- Plaque Formation:
- As time passes, more cholesterol, fatty substances, and foam cells build up and form fibrous and fatty plaque inside the wall of an arterial.
- The plaque could expand and extend in the lumen (the inside within the arterial artery) which narrows the diameter of the artery and hinders the flow of blood.
- Consequences:
- Atherosclerotic plaques may cause many complications, which include:
- The blood flow is reduced to vital organs could lead to Angina (chest pain) myocardial infarction (heart attack) or stroke.
- Plaques are prone to fragility and vulnerability that may rupture and cause blood clot formation (thrombosis) which can lead to sudden heart attacks.
- The arteries are narrowed over time which causes hypertension and contributes to the overall burden of cardiovascular disease.
- Risk Factors:
- A variety of factors can contribute to the risk of cholesterol and the accumulation of fatty deposits in the arteries. These include high levels of low-density lipoprotein (LDL) cholesterol smoking, smoking high blood pressure diabetes, and a diet high in trans and saturated fats.
- Prevention and Treatment:
- Prevention and treatment options for atherosclerosis usually are focused on reducing the levels of cholesterol, decreasing inflammation, and controlling risk factors. These may be done through lifestyle adjustments (e.g. changes to diet and exercises) as well as medication (e.g. statins, cholesterol-lowering drugs) as well as interventions (e.g. the procedure of angioplasty or the placement of stents) in more severe cases.
Understanding the mechanism behind cholesterol and the accumulation of fatty deposits in arteries is vital to stopping and controlling atherosclerosis, a condition that is significant in contributing to cardiovascular disorders including stroke and coronary artery disease.
Diagnosis through medical history, lifestyle changes, medications
“Diagnosis through medical history, lifestyle changes, medications” seems to encompass a variety of aspects of health care:
Let’s look at these elements:
- Diagnostics: Diagnosis typically involves a healthcare professional looking into the medical condition of a patient or illness. The process is typically done with the use of a variety of techniques that include physical examination, medical history as well as laboratory tests, and imaging studies. Identifying atherosclerosis could include analyzing cholesterol levels, performing an angiography procedure, or using ultrasound to detect the blockages in the arterial system.
- Medical history: A medical history is an important component of diagnosing and assessing a patient’s health. It is the process of gathering information on the patient’s previous illnesses and medical history of family members as well as current symptoms and other lifestyle elements. A thorough medical history can help medical professionals identify risks and identify the right tests to diagnose the patient.
- Lifestyle changes: Changes in lifestyle are typically part of the treatment plans for a variety of health conditions, such as ones related to cardiovascular health. Lifestyle modifications may include modifications to diet, exercise routines smoking quitting, stress management, and weight control. These modifications can help to combat or treat conditions such as atherosclerosis.
- Medicines: Medications are prescribed by healthcare professionals for the treatment or management of different ailments. When it comes to heart health, drugs such as statins are often prescribed to reduce cholesterol levels for those suffering from atherosclerosis. These medications may also include blood pressure medication or antiplatelet drugs to decrease the likelihood of cardiovascular events.
If you can provide more specific details or context for your question I’d be glad to provide more specific details or provide clarification on any particular aspects that relate to the diagnosis, lifestyle changes, or medicines with respect to cardiovascular health.
Similarities Between Arteriosclerosis and Atherosclerosis
Atherosclerosis and arteriosclerosis are both connected conditions that are both caused by changes in the arteries and share some commonalities and features, such as:
- Arterial Changes: Both arteriosclerosis and atherosclerosis are characterized by structural changes to the walls of the arteries. In both instances, the arterial walls get thicker and lose some elasticity.
- Risk Factors: A lot of risk factors that contribute to arteriosclerosis and atherosclerosis are overlapping. Risk factors include hypertension (high blood pressure) as well as high cholesterol levels smoking and diabetes, obesity, and an ancestor history of cardiovascular disease.
- Cardiovascular Consequences: Both of these conditions can cause serious cardiovascular problems. Both of them can decrease the circulation of blood through arteries which could lead to heart attacks, angina (chest pain), and heart attacks and strokes.
- Progressive nature: Atherosclerosis as well as arteriosclerosis tend to be progressive diseases. They are more likely to get worse as time passes, particularly when risk factors aren’t addressed or when lifestyle changes and treatments are not taken into consideration.
- Lifestyle Modifications: Lifestyle changes, like dietary modifications as well as smoking cessation, exercise, and managing stress are crucial elements of the prevention and management of both arteriosclerosis as well as atherosclerosis.
- Medical Use: The use of medications, like statins that lower blood pressure and cholesterol medicines, can be prescribed for patients with any condition to manage the risk factors and to slow the development of changes in arterial blood.
It is important to keep in mind that atherosclerosis can be a particular type of arteriosclerosis which is defined through the accumulation of plaque inside the arteries. Arteriosclerosis is a term that includes a variety of arterial hardening and thickening. While there are similarities in cause, causes of disease and certain aspects of diagnosis and treatment may vary between the two conditions.
Reference Books
Certainly! Here are some reference books on the topics of arteriosclerosis, atherosclerosis, and cardiovascular health:
- “Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine” by Douglas P. Zipes, Peter Libby, and Robert O. Bonow
- This comprehensive textbook provides an in-depth understanding of various cardiovascular diseases, including arteriosclerosis and atherosclerosis. It covers their pathophysiology, diagnosis, and management.
- “Pathophysiology of Heart Disease: A Collaborative Project of Medical Students and Faculty” by Leonard S. Lilly
- This book offers a concise overview of cardiovascular diseases, including arteriosclerosis and atherosclerosis. It is written in a way that is accessible to medical students and healthcare professionals.
- “Atherosclerosis: Risk Factors, Prevention, and Treatment” by Peter Libby, Valentin Fuster, and Russell Ross
- Focused specifically on atherosclerosis, this book explores the mechanisms, risk factors, and preventive strategies for this condition. It is an excellent resource for those interested in atherosclerosis research.
- “Hurst’s the Heart” by Valentin Fuster, Robert A. Harrington, and Richard Walsh
- This renowned cardiology textbook covers a wide range of cardiovascular topics, including arteriosclerosis and atherosclerosis. It is an authoritative reference in the field.
- “Atherosclerosis: Diet and Drugs” by Arnold von Eckardstein and Dimitris N. Kiortsis
- This book delves into the dietary and pharmacological aspects of managing atherosclerosis. It provides insights into the role of nutrition and medications in preventing and treating this condition.
- “Vascular Medicine: A Companion to Braunwald’s Heart Disease” by Mark Creager and Joseph Loscalzo
- Focusing on vascular health, this book discusses various aspects of arterial diseases, including arteriosclerosis and atherosclerosis, from a clinical and research perspective.
Conclusion
Atherosclerosis and arteriosclerosis are both complex conditions that have distinct features, but they have commonalities in terms of risks, consequences for cardiovascular health as well as the importance of lifestyle adjustments and medication for their prevention and treatment.
Understanding the causes of these conditions is crucial for improving cardiovascular health, reducing risk, and enhancing overall cardiovascular health. Being aware and adopting healthy practices can play an important role in the prevention and management of these ailments, eventually leading to better outcomes as well as an improved quality of life.