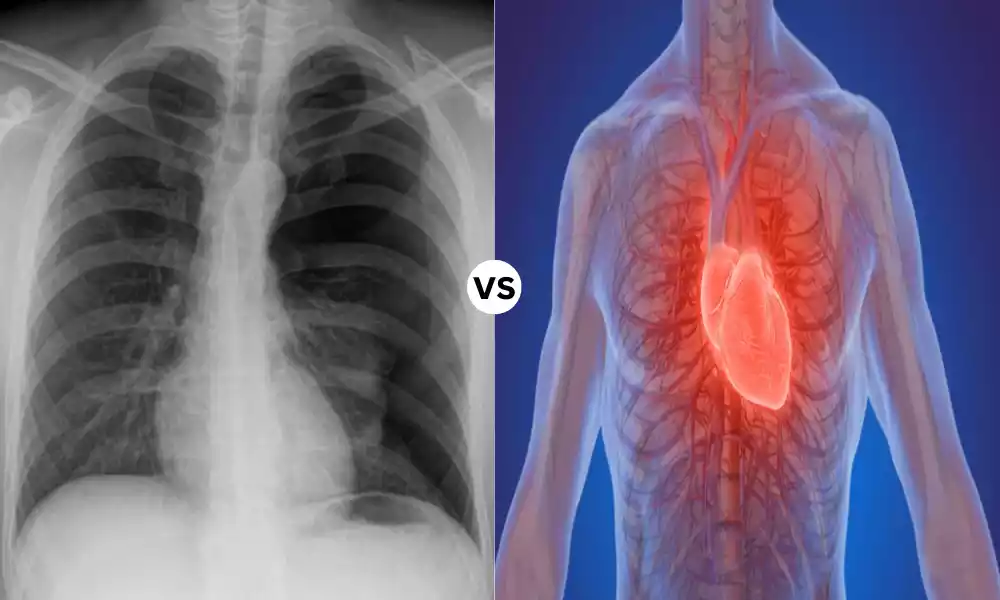
Tension Pneumothorax, as well as Cardiac Tamponade, are two critical medical emergencies that require immediate attention and an accurate diagnosis. This article will explore the unique characteristics of these conditions, which include the anatomy of these conditions, their clinical presentations as well as diagnostic strategies, management strategies, and results.
Understanding the distinctions between Tension Pneumothorax as well as Cardiac Tamponade is vital for health professionals to provide the right and life-saving treatment.
Definition of Tension Pneumothorax
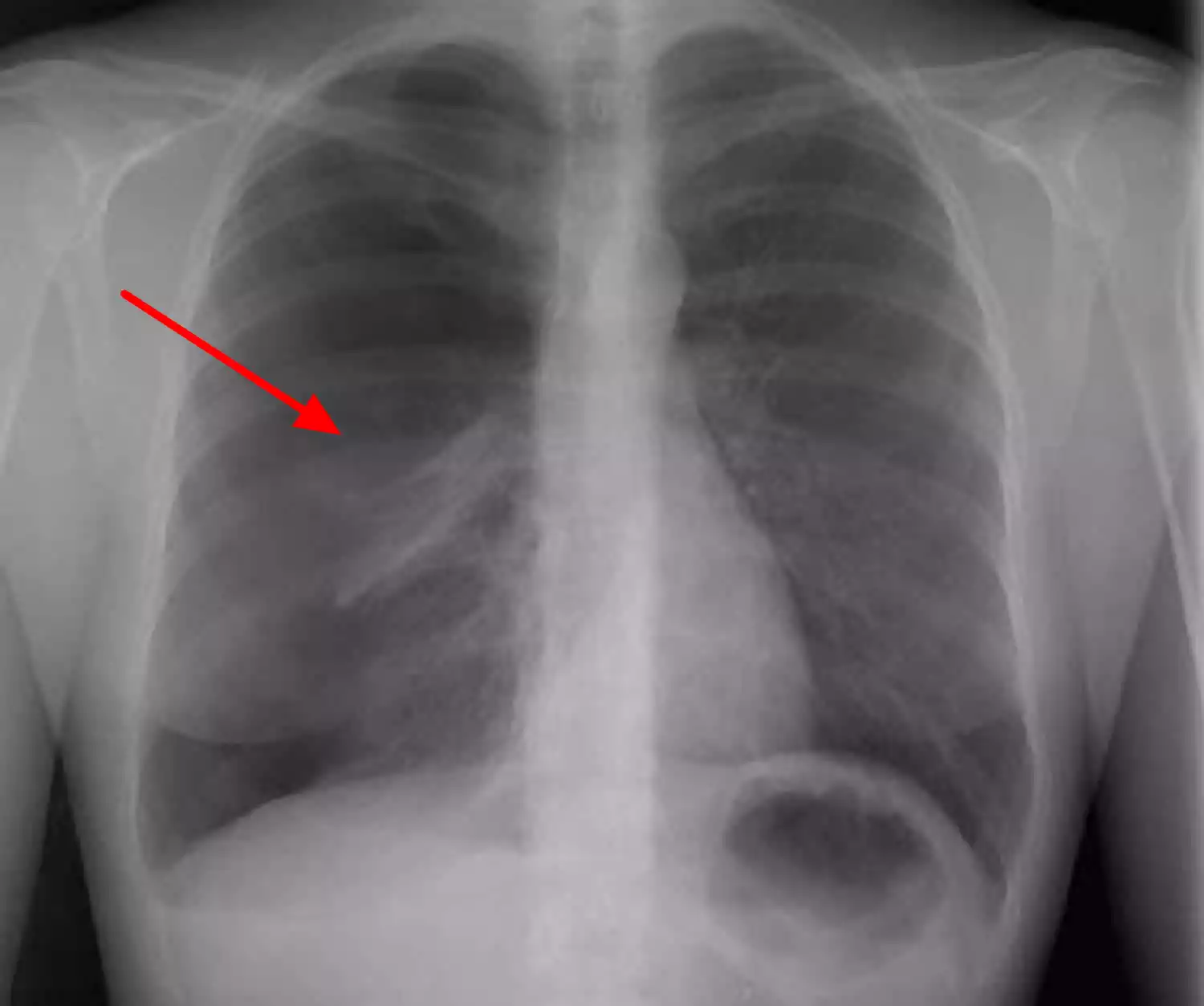
Tension Pneumothorax is a health emergency that is characterized by the buildup of air inside the pleural cavity, which is the space between the chest and lung. Contrary to a typical pneumothorax tension pneumothorax causes a steady increase in air pressure inside the pleural cavity, causing compression of the affected lung, and moving the mediastinum (the central region of the chest, which houses vital structures) towards the side that is not affected that is the side of chest. This can lead to decreased lung function, lower the output of cardiac muscle, as well as even death if it is not properly treated.
Definition of Cardiac Tamponade
Cardiac Tamponade is a serious medical condition characterized by the accumulation of fluids including blood and other bodily fluids, inside the pericardial sac. It is the thin membrane that surrounds the heart.
As the fluid dries up in the pericardial sac, it causes pressure on the heart, which can affect its capacity to function. This could result in decreased heart output and diminished function, eventually leading to an emergency situation that could be life-threatening.
Cardiac tamponade can be viewed as an emergency medical situation and immediate intervention is needed to ease the stress on the heart and restore normal functioning of the heart.

Importance of distinguishing between Tension Pneumothorax and Cardiac Tamponade
The distinction between Tension Pneumothorax and Cardiac Tamponade is of paramount importance in the clinical setting for many important reasons:
- Emergency Interventions Each of them are dangerous medical emergency, however, they require different approaches. Incorrect diagnosis or confusion between these two can result in unsuitable interventions that can aggravate the patient’s illness. The prompt and accurate diagnosis is essential to provide the right treatment.
- Different Pathophysiology: Tension Pneumothorax causes the pressure of the lung as well as mediastinal shifting while Cardiac Tamponade is characterized by tension in the heart. Understanding the pathophysiological causes helps in a more targeted treatment.
- Different Clinical Presentations: Tension Pneumothorax is a condition that manifests with breathing distress, absent breath sounds, and chest asymmetry while Cardiac Tamponade manifests with signs of cardiac impairment, including hypertension, increased jugular venous pressure, and a muffled heart sound. The recognition of these differences aids in the clinical evaluation.
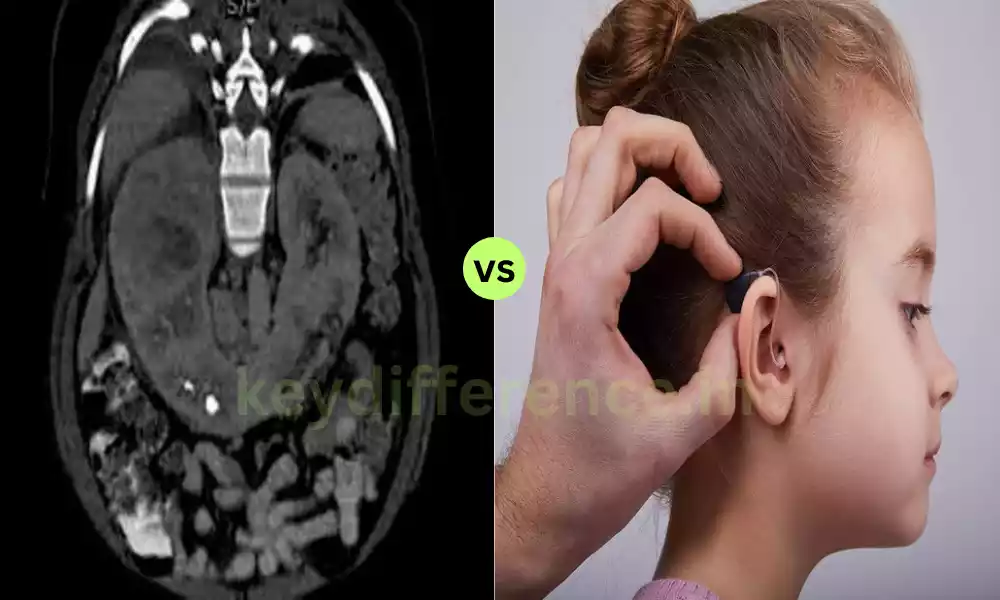
- Quality of Diagnostics: Tests and diagnostic instruments used to determine these conditions aren’t interchangeable. The accuracy of diagnosis is dependent on selecting the most appropriate method of diagnosis (e.g. echocardiography for Cardiac Tamponade, chest X-ray for Tension Pneumothorax).
- Treatment Modalities: Tension Pneumothorax calls for chest tube or needle placement to liberate trapped air trapped in the area of the pleural cavity. However, Cardiac Tamponade requires pericardiocentesis to eliminate the accumulation of fluid surrounding the heart. Confusion between these treatments could result in serious delays.
- Prognosis and Outcome: Both conditions have distinct prognostic implications. Interventions that are prompt can result in positive outcomes, while untreated or delayed treatment could cause severe morbidity and even death. Accurate differentiation helps improve patient outcomes.
- Resource Allocation: Within a medical setting, resources such as equipment, personnel, and facilities have to be efficiently allocated. Knowing the particular requirements for managing each illness makes sure that the proper resources are readily available in the event of need.
- Educational and Training: Healthcare professionals need to be educated and trained on the specifics of these conditions in order to make quick and informed choices in situations of high pressure.
Knowing the difference between Tension Pneumothorax from Cardiac Tamponade is a critical expertise for healthcare professionals because it has a direct impact on the treatment of patients, their care, and the outcomes of the life-threatening emergency.
Comparison Table of Tension Pneumothorax and Cardiac Tamponade
Here’s a comparison table highlighting the key differences between Tension Pneumothorax and Cardiac Tamponade:
| Characteristic | Tension Pneumothorax | Cardiac Tamponade |
|---|---|---|
| Definition | Accumulation of air in pleural space, leading to lung compression and mediastinal shift | Accumulation of fluid (e.g., blood) in the pericardial sac, compressing the heart |
| Etiology | Trauma, lung disease, medical procedures | Trauma, pericarditis, malignancy, aortic dissection, or other pericardial diseases |
| Anatomy Affected | Pleural space (around the lung) | Pericardial sac (around the heart) |
| Pathophysiology | Air enters pleural space, causing lung collapse and mediastinal shift | Fluid accumulates in the pericardial sac, compressing the heart chambers |
| Clinical Presentation | Respiratory distress, decreased breath sounds, hyper resonance on percussion, chest asymmetry | Hypotension, elevated jugular venous pressure, muffled heart sounds, pulsus paradoxus |
| Diagnostic Evaluation | Chest X-ray, CT scan, arterial blood gas analysis | Echocardiography (echo), ECG, pericardiocentesis |
| Immediate Intervention | Needle decompression or chest tube insertion to release trapped air | Pericardiocentesis to remove pericardial fluid |
| Surgical Options | Rarely required for severe cases (e.g., thoracotomy) | Pericardial window or surgical drainage |
| Medications | Not a primary treatment | Diuretics or medications addressing the underlying cause |
| Potential Complications | Hypoxia, tension physiology, shock | Cardiac arrest, decreased cardiac output, shock |
| Prognosis | Favorable with prompt treatment | Favorable with prompt treatment, but severe cases can be life-threatening |
Please note that accurate diagnosis and differentiation between these conditions are essential for appropriate treatment and patient outcomes. This table provides a concise overview of the key distinctions between Tension Pneumothorax and Cardiac Tamponade.
Pathophysiological mechanisms
The pathophysiologic mechanisms that are involved in Tension Pneumothorax as well as Cardiac Tamponade are distinct, and understanding the underlying mechanisms is vital for the proper diagnostics and treatments.
Here’s a brief overview of the pathophysiology that is associated with each of the conditions:
Tension Pneumothorax:
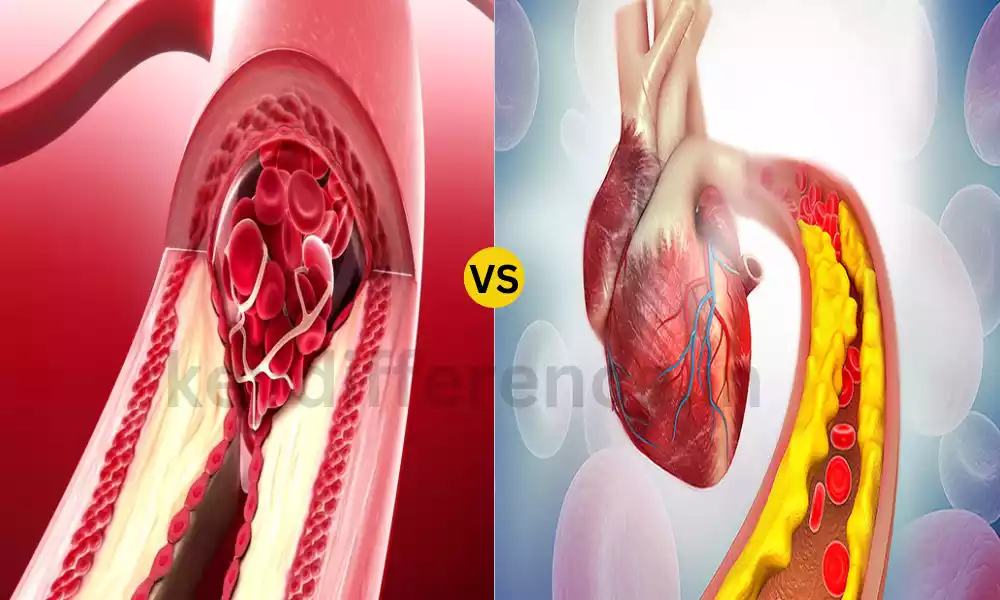
- Air entry in the Pleural Space: Tension Pneumothorax typically is caused by trauma or other lung conditions. It happens when air gets into the pleural space, which is the space that lies between lung tissue and the chest wall. It can be caused by the lung being punctured due to an injury to the ribs or a medical procedure.
- Progressive air accumulation: Contrary to a typical pneumothorax in which air is injected and escapes naturally tension pneumothorax has a one-way valve mechanism. Air can be able to enter the pleural cavity, but it can’t easily leave. As air builds up the pressure increases within the Pleural cavity.
- Lung Compression: Air that is accumulated gradually compresses the lung affected and causes it to shrink. The lung’s capacity is diminished. for expansion and to function which can lead to respiratory discomfort.
- Mediastinal Shift: The increasing pressure inside the pleural cavity also pushes the mediastinum (the middle part of the chest that houses vital structures such as the great vessels and heart) out of the side that is affected and towards the side that is not affected that is the opposite side of the chest. This could affect the flow of blood back to the heart and can hinder the function of the heart.
Cardiac Tamponade:
- Fluid accumulation within the Pericardial Sac: Cardiac Tamponade occurs when blood-like fluid, which is typically it could also be various bodily fluids builds up within the pericardial sac that surrounds the heart.
- The increase in Pericardial Pressure: As the fluid builds and expands, it puts pressure on your heart’s chambers. The increased pressure inside the pericardial sac pressures the myocardium (heart muscle) and impairs the ability of the heart to pump and fill effectively.
- Impairment in Cardiac Function: A compression of the heart caused by the pericardial fluid decreases the output of the heart. This may result in a decrease in heart rate and strokes, as well as cardiac arrest in the most severe cases.
- Hemodynamic Effects: The increased pericardial pressure affects the ability of the heart to fill in diastole which results in a decrease in cardiac output and hypotension throughout the system. Furthermore, the pressure can affect the relaxation of heart chambers, leading to an increase in central venous pressure, as well as the pulsus paradoxus (an abnormally lower blood pressure systolic during the period of inspiration).
Tension Pneumothorax primarily involves the accumulation of air inside the pleural cavity, which leads to mediastinal and lung pressure. Contrarily, Cardiac Tamponade involves the formation of fluids in the pericardial sac that compresses the heart and affects its functions. Understanding the distinct pathophysiological causes is essential for a precise diagnosis and prompt intervention.
Physical examination findings
Physical examination results to determine Tension Pneumothorax as well as Cardiac Tamponade differ due to the distinct anatomical structures as well as the pathophysiological mechanism associated with each condition.
Here are the most important physical exam results for both conditions:
Tension Pneumothorax:
- Respiratory Distress: Patients suffering from Tension Pneumothorax typically experience severe respiratory distress. They could experience short, shallow breathing as well as an increased effort to breathe.
- Absent or Decreased Breath sounds: On auscultation, you might hear decreased and absent sounds from one side of your chest. This is caused by the lung’s collapse.
- Hyperresonance of Percussion: A percussion (tapping on the chest) on the side affected could produce a hyperresonant sound because of an air pocket within the space between pleural and aural.
- Chest Asymmetry: The visual inspection can show chest asymmetry, one side appearing bigger and broader than the side that is not affected.
- Tracheal Deviation: In the most severe instances it is possible to have a divergence of the trachea from the side affected due to the shift in the mediastinal axis caused by the accumulation of air.
Cardiac Tamponade:
- Hypotension: People with Cardiac Tamponade frequently have the symptoms of low blood pressure (hypotension) because of impaired cardiac output. This is a crucial characteristic and an important finding.
- High Jugular Venous Pressure (JVP): On physical examination, it is possible to detect an elevated jugular venous pressure, which indicates an increase in central venous pressure as a result of pressure on the atrium of the right due to the fluid pericardial.
- Heart Sounds that are muffled: Auscultation of the lungs can reveal distant or muffled heart sounds. This happens due to the fact that pericardial fluid reduces any transmission from heart sounds to the chest wall.
- Pulsus paradoxus: Pulsus paradoxus refers to an unusual decrease in the systolic blood pressure in inspiration. It is evident during Cardiac Tamponade and is indicative of the fluctuation in the cardiac output throughout breathing.
- narrowing of the pulse pressure: The contrast between diastolic and systolic blood pressure (pulse pressure) decreases in Cardiac Tamponade because of impaired diastole ventricular filling.
- Beck’s Triad (in extreme situations): Beck’s Triad comprises three of the most well-known symptoms of Cardiac Tamponade.
- Hypertension (low blood pressure)
- Elevated JVP
- The heartbeats are muffled
It is important to remember that the clinical signs and symptoms can differ in their severity and all patients are afflicted with all of these symptoms and signs. In addition, early recognition of these symptoms and their relationship to the root cause is essential for prompt diagnosis and treatment.
Complications and Prognosis
The prognosis and complications of Tension Pneumothorax as well as Cardiac Tamponade could differ according to how severe the problem is and the timeframe for treatment.
Here’s a brief overview of the possible complications, as well as the prognosis of each of the conditions:
Tension Pneumothorax:
Complications:
- Hypoxia: The condition of tension pneumothorax may cause serious hypoxia (low levels of oxygen) due to impaired lung function and decreased ventilation for the affected lungs.
- Tension Physiology: When the condition gets worse it may cause tension physiology, which can result in the heart becoming unstable, a decrease in the return of venous blood, and even shock.
- Shock: If the situation is serious untreated tension Pneumothorax can cause shock, which could be life-threatening.
Prognosis:
- With prompt diagnosis and the proper treatments (needle decompression or placement of a chest tube) to free trapped air and improve breathing function outlook of Tension Pneumothorax can be good. The majority of patients heal without long-term complications.
- If it is not immediately treated, particularly in instances of shock or tension physiology or shock, tension Pneumothorax may cause extreme morbidity or even death.
Cardiac Tamponade:
Complications:
- Cardiac Affliction: Untreated or severe Cardiac Tamponade could cause cardiac arrest because of being compressed in heart chambers, which prevents the heart from producing the required amount of blood.
- Increased Cardiac Output: The decreased filling and pumping of the heart can result in reduced cardiac output. This could cause organ dysfunction throughout the body.
- shock: Cardiac Tamponade could cause shock because of a decrease in blood pressure as well as inadequate perfusion of the tissue.
Prognosis:
- The outlook for Cardiac Tamponade largely depends on the speed of diagnosis and treatment. The early recognition of the condition and the pericardiocentesis (or other treatments that are appropriate) can result in an improved outcome.
- In the event that treatment is not given promptly the Cardiac Tamponade may turn life-threatening. The mortality rate can be very high with no intervention.
The prognosis of both the tension Pneumothorax and Cardiac Tamponade is significantly improved by a quick and precise diagnosis followed by the appropriate treatment.
Early treatment can avoid severe complications and improve the chances of a positive outcome. However, delays in the diagnosis and treatment process could lead to serious complications and worse prognoses for both conditions.
Prognosis with prompt treatment
If treated quickly and properly, the prognosis for Tension Pneumothorax and Cardiac Tamponade may be drastically improved.
Here’s a brief summary of the potential outcomes for each condition that are treated promptly:
Tension Pneumothorax and prompt treatment:
- When Tension Pneumothorax is discovered at an early stage and treated immediately, the prognosis is likely to be positive.
- In the chest, needles or a tube are used to release the air trapped in the pleural cavity. This allows the affected lung to expand, and then get back to normal function.
- A majority of patients notice an immediate improvement in their breathing and oxygen levels after intervention.
- The root causes of hypoxia and tension are capable of being reversed swiftly by rapid treatment.
- If they receive the proper treatment, patients can recover without having to deal with concerns for the future. The risk of dying is significantly decreased.
Cardiac Tamponade is accompanied by Prompt Treatment:
- The ability to recognize and intervene quickly is vital when dealing with Cardiac Tamponade to achieve a favorable prognosis.
- Pericardiocentesis is the procedure of getting rid of the pericardial fluid that accumulates and is the principal treatment.
- Pericardiocentesis done early may aid in reducing the strain on the heart, as well as help improve the functioning that the heart.
- The future outlook for treating Cardiac Tamponade promptly is generally positive. Many patients recover with no lasting negative effects.
- The risk of shock and heart attack is preventable through prompt intervention.
- The most important factor in achieving a positive outcome is to have a quick diagnosis and a prompt start of treatment.
The prompt detection of symptoms that indicate a problem with the patient and the right diagnosis and rapid intervention are vital to ensure the highest possible prognosis.
An early intervention could help reduce the risk of serious complications and increase the chances of a complete recovery for patients with Tension Pneumothorax and Cardiac Tamponade.
Similarities Between Tension Pneumothorax and Cardiac Tamponade
Although Tension Pneumothorax, as well as Cardiac Tamponade, are distinct medical emergency situations with distinct reasons and anatomical sites.
There are some similarities between them which include:
- Life-threatening Emergencies: The Tension Pneumothorax and Cardiac Tamponade are serious medical emergencies that require immediate attention and treatment. If treatment is delayed or not received properly, it can result in serious complications and could be fatal in both.
- impaired cardiac function: In both conditions, the impairment of cardiac function could be observed. In Tension Pneumothorax, the compressing of lung tissue and the mediastinal shift may, in turn, affect cardiac function, through a decrease in venous return towards the heart. For Cardiac Tamponade, the accumulation of pericardial fluid directly presses the heart, affecting the ability of the heart to pump efficiently.
- Hemodynamic Effects: Both conditions can result in hemodynamic effects such as the condition of hypotension (low blood pressure) as well as diminished cardiac output, as well as the potential for shock. The hemodynamic changes are a result of impaired cardiac function during Cardiac Tamponade, as well as the mediastinal change that occurs in Tension Pneumothorax.
- Clinical signs of shock: People suffering from both tension Pneumothorax or Cardiac Tamponade can display clinical signs of shock like diminished mental status as well as pallor, cold and clammy skin, and rapid breathing. These signs indicate insufficient tissue perfusion.
- Respiratory Distress: While the main problem with Cardiac Tamponade is cardiac compromise patients can suffer from respiratory distress as a result of the stress on the heart. In Tension Pneumothorax respiratory distress is a common condition since it directly affects the lung’s function.
- Physical Examination Findings: Both of these conditions may show an elevated jugular vasopressor (JVP) upon physical exam. When there is Tension Pneumothorax JVP could be high because of a lower return of venous blood and, when it is Cardiac Tamponade, it is increased due to a lack of filling of the heart.
Although there are some similarities, it is important to note that the root reasons, the anatomical location, and the primary pathophysiological mechanism for Tension Pneumothorax as well as Cardiac Tamponade are distinct.
A precise distinction between these two conditions is vital in order to determine the best treatment since the strategies used to manage them are vastly different.
Reference Books
Certainly! Here are some reference books related to medical topics, as well as a few general reference books that cover a wide range of subjects:
Medical Reference Books:
- Harrison’s Principles of Internal Medicine by Dan L. Longo et al. – A comprehensive textbook covering various aspects of internal medicine.
- Current Medical Diagnosis and Treatment by Maxine A. Papadakis and Stephen J. McPhee – A practical guide to the diagnosis and management of medical conditions.
- Robbins and Cotran Pathologic Basis of Disease by Vinay Kumar et al. – A fundamental resource for understanding the pathophysiology of diseases.
- Clinical Guidelines in Primary Care by Amelie Hollier – Offers evidence-based guidelines for primary care practitioners.
- The Washington Manual of Medical Therapeutics by Hemant Godara and Pavan Bhat – A concise guide to medical diagnosis and treatment.
General Reference Books:
- The Merck Manual of Diagnosis and Therapy – A well-respected medical reference guide with information on various medical conditions.
- The Oxford Companion to Medicine edited by Stephen Lock et al. – Provides insights into the history, science, and practice of medicine.
- The Cambridge Encyclopedia of Human Evolution edited by Steve Jones et al. – A comprehensive resource on human evolution and anthropology.
- The Encyclopedia of Popular Music edited by Colin Larkin – An extensive reference for music enthusiasts covering various genres and artists.
- The World Atlas of Wine by Hugh Johnson and Jancis Robinson – A renowned reference for wine enthusiasts, offering information on wine regions, grape varieties, and more.
- The Oxford English Dictionary – The definitive reference work on the English language, tracing the history and development of words and meanings.
- The Elements: A Visual Exploration of Every Known Atom in the Universe by Theodore Gray – A visually stunning reference book that explores the periodic table and the elements.
Conclusion
Rapid and accurate diagnosis of medical issues such as Tension Pneumothorax or Cardiac Tamponade is crucial for successful treatment and improved outcomes.
Knowing the primary distinctions, recognizing the clinical signs, and implementing timely interventions can mean a crucial difference in the outcome of these situations.
Comprising definitions, pathophysiology, clinical findings, and prognosis, are excellent sources for healthcare professionals as well as anyone who wants to improve their knowledge about these potentially fatal illnesses.