Plantar fasciitis and bony spurs are Bone Spurs and Plantar Fasciitis orthopedic issues that can trigger heel pain and discomfort. Although they have some similarities in terms of symptoms, they also differ in origins as well as their locations and treatment options.
The differences and similarities between these conditions help you be aware of the conditions and make an informed decision about seeking medical treatment.
Definition of Bone Spurs
Bone spurs also referred to as osteophytes, are bony growths or projections that form around the edges of existing bones. These tend to develop as a result of ongoing stress or pressure within joints or along the bone’s surface.
Bone spurs may develop throughout the body, such as joints, the spine, and around the heel. they can be linked to ailments like osteoarthritis and degenerative joint diseases.
These bony growths can trigger discomfort, limit joint motion, and could need medical attention, particularly when they cause pain to nearby nerves or tissues.

Definition of Plantar Fasciitis
Plantar fasciitis is a common orthopedic disorder that is characterized by pain and swelling of the fascia an extensive connective tissue that extends along the lower part of our feet, extending from the bone of our heel (calcaneus) and up the top of our toes.
The plantar fascia plays a vital role in maintaining the arches of your foot as well as absorbing the shock of running and walking. If it is inflamed or damaged it could cause acute or stabbing pains in the heel. It is evident in the early morning, or following periods of rest.
Plantar fasciitis can be due to overuse, insufficient footwear, and weight gain, as well as other factors that place tension on the fascia of the plantar. It is the most frequent cause of heel pain and can affect people of all ages, however, it is more common in middle-aged adults.
An accurate diagnosis and proper management such as stretching exercises, rest as well as orthotic devices, and physical therapy, are vital in treating plantar fasciitis and easing the discomfort and pain.
Comparison Table of Bone Spurs and Plantar Fasciitis
Here’s a comparison table highlighting the key differences and similarities between bone spurs and plantar fasciitis:
| Aspect | Bone Spurs | Plantar Fasciitis |
|---|---|---|
| Definition | Bony outgrowths on existing bones | Inflammation of the plantar fascia |
| Common Locations | Joints (e.g., spine, knee), heel | Primarily affects the heel |
| Primary Cause | Ongoing stress, pressure, inflammation | Overuse, improper footwear, obesity |
| Symptoms | Limited joint movement, sharp pain | Heel pain, especially in the morning |
| Diagnosis | Imaging (X-rays, MRI), clinical evaluation | Clinical examination, imaging (X-rays, ultrasound) |
| Treatment | Surgical removal (in severe cases) | Conservative (rest, orthotics, therapy) |
| Shared Symptoms | Heel pain | Heel pain |
| Imaging Techniques | X-rays, MRI | X-rays, ultrasound |
| Risk Factors | Age, obesity, joint stress | Age, obesity, overuse, improper footwear |
| Importance of Early Intervention | Necessary to prevent complications | Important to prevent chronic pain and further injury |
Please note that while there are similarities in symptoms (heel pain) and diagnostic methods (imaging), the causes, locations, and treatment approaches for bone spurs and plantar fasciitis differ significantly.
Consulting a healthcare professional is crucial for an accurate diagnosis and appropriate treatment for either condition.
The importance of distinguishing between Bone Spurs and Plantar Fasciitis
Differentiating between plantar fasciitis and bone spurs is vital for a variety of reasons:
- Treatment Options: The treatment approaches for both conditions are very different. Bone spurs might require surgery to remove them in extreme instances, while plantar fasciitis is generally treated through stretching, rest orthotics, and stretching therapy. A misdiagnosis could lead to ineffective treatment and a prolonged period of discomfort.
- Preventing Complications: Plantar fasciitis can cause pain and restrict mobility. If left untreated, they could result in more serious complications. Bone spurs can encroach on blood vessels or nerves nearby and cause greater pain and joint injury. Plantar fasciitis that is not treated properly can cause persistent heel pain and changes in gait. This could lead to other muscular and skeletal problems.
- Educational for Patients: Accurate diagnosis helps patients better understand their condition. It helps them decide on the best course of action to treat and resolve the root cause. Patients are also able to make informed decisions about treatment options and lifestyle changes.
- Economic impact: Misdiagnosis can lead to unneeded medical expenses as well as incorrect treatments and prescriptions. An accurate diagnosis can reduce the additional expenses and make sure that resources are used effectively.
- Qualitative of Life: A prompt and accurate diagnosis enhances the quality of people suffering from these diseases. Treatment that is effective can ease the pain, improve mobility, and allow patients to resume their regular routine.
- Preventing needless procedures: Correctly distinguishing between plantar fasciitis and bone spurs helps avoid unnecessary surgery. Surgery comes with inherent risks therefore it is only recommended to consider it only when it is the best method of treatment.
Knowing the difference between plantar fasciitis and bone spurs is vital to ensure the most appropriate and effective treatment to reduce the risk of complications and enhance the overall health of those suffering from these ailments.
Consult a medical professional for an accurate diagnosis is the initial step towards getting the best results for patients.
Inflammation of the plantar fascia
Inflammation of the fascia plantar also known as plantar fasciitis is a very common orthopedic condition that manifests as swelling, irritation, and pain in the plantar fascia, a stretch of connective tissue running across the foot’s bottom and connects with the heel bone (calcaneus) with the toes’ bases.
The inflammation is usually caused by injuries, overuse, or repetitive strain upon the fascia of the plantar. Here are some important information regarding inflammation of the plantar fascia
- The causes are: Plantar fasciitis typically is caused by repeated tension upon the plantar fascia which may cause tiny tears in the tissue.|The most common causes are:
- Running or walking too much, particularly when on surfaces that are hard.
- Shoes that are not supportive or that do not provide adequate arch support.
- Increases in physical activity suddenly or a change in routines for exercise.
- Being overweight can make it harder over the fascia plantar.
- The symptoms: Inflammation of the plantar fascia is often accompanied by these symptoms:
- Stabbing or sharp pain in the heel area, especially when you awake or after a long time of rest.
- It is a condition that gets better with exercise but can return after prolonged durations of walking or standing.
- An increase in discomfort after physical exercise.
- Diagnostics: Healthcare professionals typically identify plantar fasciitis using an examination that is clinical, where they assess the patient’s symptoms and conduct specific tests. Imaging studies like ultrasound or X-rays can be performed to rule out other ailments or determine the severity of inflammation.
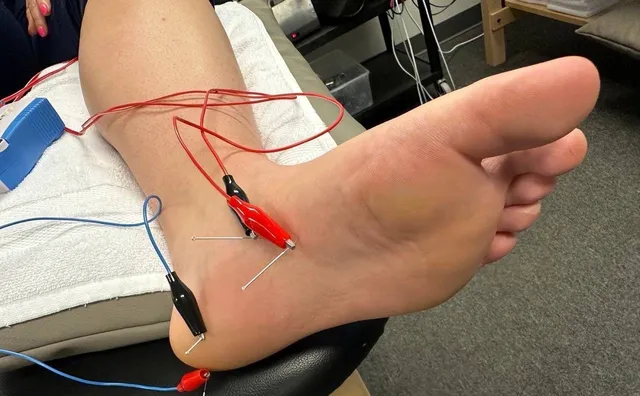
- Therapy: The primary goal of treatment for plantar fasciitis is reducing swelling and relieving discomfort. Treatment options for plantar fasciitis include:
- Avoiding activities that can aggravate the symptoms.
- Exercises to stretch your muscles and ease stress on the plantar fascia.
- Ice application to ease inflammation.
- Wearing supportive shoes and orthotic inserts to give arch support.
- Physical therapy to build the muscles of the foot and calf.
- Prescription or over-the-counter medications are available to treat inflammation and pain.
- In some rare instances, when conventional measures do not work, more aggressive treatments such as corticosteroid injections or shockwave therapy could be contemplated.
- prevention: Preventing plantar fasciitis is about taking measures to minimize the chance of excessive use or strain on the fascia plantar. This involves wearing the right shoes as well as keeping a healthy weight, making gradual adjustments in your physical activity, and regular stretching and strengthening of the foot and lower leg muscles.
Inflammation of the plantar facia can cause pain and debilitating conditions, however, with the right treatment and care patients can experience relief and resume their regular activities.
It is essential to speak with an expert in healthcare to get a correct diagnosis and a customized treatment plan when you suspect that you may have plantar fasciitis.
In severe cases, surgical intervention
In cases of serious plantar fasciitis, surgery could become a treatment option, if conventional methods have proved ineffective to alleviate pain and improve the condition of the patient. It is important to remember that surgery is usually considered to be a last resort and it’s not the first-line treatment for all cases of plantar fasciitis.
Here are a few key aspects to know about surgical treatment for plantar fasciitis that is severe:
- The indications to undergo surgery: The procedure for plantar fasciitis is generally thought of when these criteria are satisfied:
- The patient suffers from persistent and intense heel pain that affects their daily life and restricts their ability to carry out everyday tasks.
- Treatments that are conservative, like rest or orthotic devices, physical therapy, and medication do not provide enough relief over a prolonged period (usually between 6 and 12 months).).
- Image studies (e.g. imaging studies, X-rays, or MRI) provide evidence of structural anomalies within the plantar fascia like thickening or chronic degeneration.
- Surgery Procedures: There are several surgical procedures that are used to treat plantar fasciitis. The procedure chosen will be based on the preference of surgeons as well as the individual patient’s situation, and the extent to which the patient is suffering from plantar fasciitis. The most common surgical options are:
- Plantar Fascia Releasing: This involves partially cutting the plantar fascia in order to alleviate tension and decrease inflammation.
- Gastrocnemius Recession: In certain cases, tight calf muscles (gastrocnemius) could cause plantar fasciitis. Strengthening these muscles can ease tension in the fascia of the plantar.
- Tenex Treatment: This minimally invasive procedure utilizes ultrasound to detect and eliminate damaged tissue within the fascia plantar.
- Risks and considerations: As with any procedure, there are some hazards and pitfalls associated with surgery for plantar fasciitis such as:
- Infection
- Nerve damage
- Scarring
- Longer recovery time
- There is no guarantee of pain relief
- Postoperative Treatment: Following surgery, patients usually have a rest period and rehabilitation. Exercises for mobility and physical therapy can be prescribed to speed recovery and avoid complications. Patients should follow the surgeon’s instructions following surgery to maximize healing.
- Alternate Treatments: Prior to deciding on surgery, sufferers must consider the various options for treatment alternatives, and seeking an additional opinion from a physician might be beneficial. Many patients with plantar fasciitis have significant relief with non-surgical methods.
It is essential for those contemplating surgery for serious plantar fasciitis to engage in an extensive conversation with their physician as well as an orthopedic specialist.
They must weigh the advantages and risks of surgery, and also consider alternative treatment options in order in order to make an informed decision regarding the most appropriate option for their particular condition.
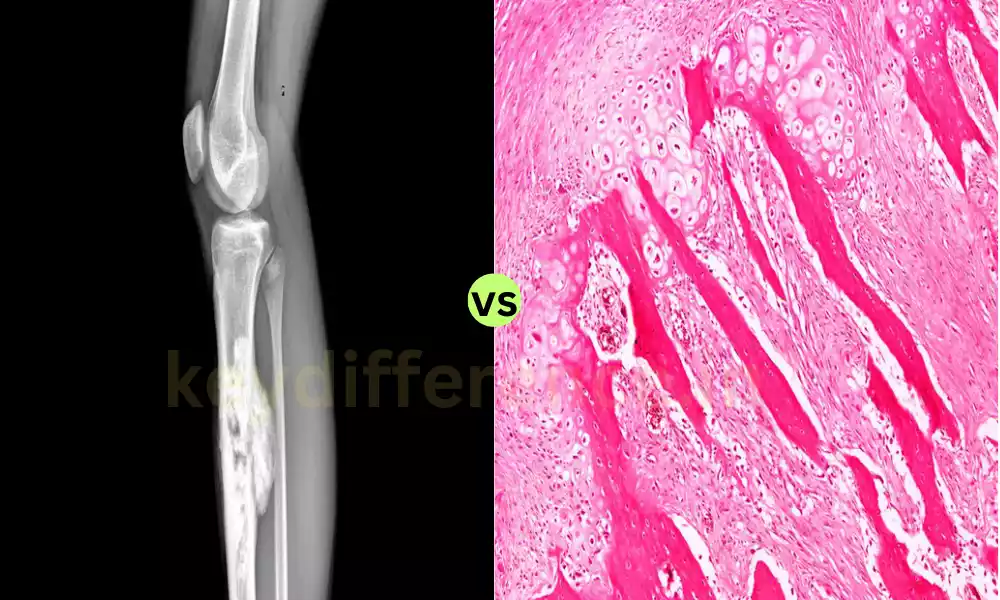
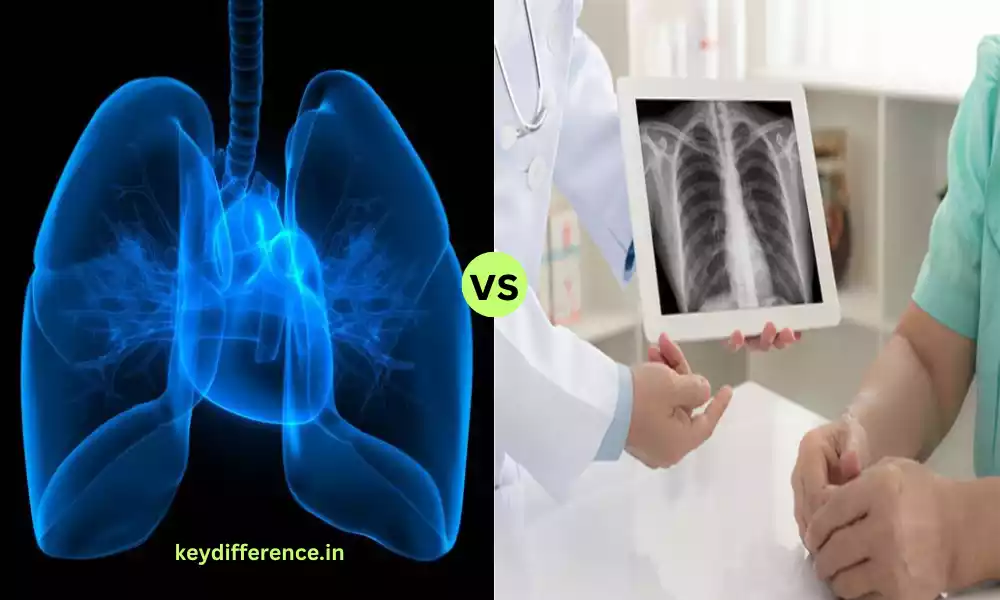
Imaging techniques used for diagnosis in both conditions
Imaging techniques play an important part in identifying bone spurs as well as plantar fasciitis. The imaging techniques aid medical professionals in seeing these affected regions, evaluating the severity of the problem, and differentiating them from other causes of discomfort or pain.
Here are some common imaging techniques that are used to diagnose both of these conditions:
- X-rays (Radiography):
- Bone Spurs: X-rays can be particularly useful in finding bone spurs. They are able to reveal the existence of, the size, and the place of bone spurs within joints and around joints as well as on bones.
- Plantar Fasciitis: X-rays are not frequently utilized to diagnose plantar fasciitis specifically because they mostly affect soft tissues, such as that of the plantar fascia. However, they could be used to rule out any other foot ailments or to determine the alignment of the bones of the foot.
- Magnetic Resonance Imaging (MRI):
- Bone spurs: MRI examinations provide specific pictures of the soft tissue including ligaments and tendons, which help to identify related soft tissue issues or the damage due to bone spurs.
- Plantar Fasciitis: MRIs can be useful for diagnosing plantar fasciitis because they may reveal inflammation, thickening, and tears within the fascia of the plantar. They can be particularly helpful when the diagnosis is not clear or when additional soft tissue issues are suspected.
- Ultrasound:
- Bone Spurs: Ultrasound is not usually used to detect bone spurs.
- Plantar Fasciitis: Ultrasound is an excellent method to diagnose plantar fasciitis. It offers real-time images of the fascia plantar which allows healthcare professionals to evaluate the thickness of the fascia and identify the signs of inflammation or tears.
Though X-rays or MRIs can be utilized in some instances for both of these conditions however ultrasound is a specialized and reliable imaging technique to diagnose plantar fasciitis due because it can directly visualize the fascia plantar.
The method of imaging chosen is based on the particular symptoms of the patient, their clinical evaluation, and the judgment of a healthcare professional.
It is possible to combine the imaging methods that can be employed to get an accurate evaluation of the problem and identify other possible causes of discomfort or pain within the affected region.
Similarities Between Bone Spurs and Plantar Fasciitis
While bone spurs and fasciitis are distinct orthopedic ailments that have different causes and treatments they share a few similarities, mostly in relation to their symptoms and risk factors.
Here are the main similarities between plantar fasciitis and bone spurs:
- Heel pain: Both conditions can cause severe heel pain, which is typically the most prominent sign. The pain can be intense stabbing, aching, or stabbing in nature. In all cases, the pain may be felt more intensely when a person is carrying a weight, such as sitting or walking.
- Morning Discomfort: Patients suffering from both plantar fasciitis and bone spurs frequently experience more stiffness and pain in the heel that is affected, particularly in the mornings or following intervals of rest. This is a characteristic of these ailments.
- Risk Factors: Some risk-related factors can be related to both bone spurs as well as plantar fasciitis. These include:
- Age: The two conditions can be found more prevalent among older people but they are also affecting everyone of any age.
- Obesity: A high body mass can increase the stress on the feet and may contribute to the development or worsening of both conditions.
- Strain and overuse: Activities that place repeated stress on feet, including long-distance jogging or standing for prolonged periods could cause an increase in the likelihood of plantar fasciitis and bone spurs.
- Diagnostic Imaging: For both types of conditions diagnostic imaging techniques, like X-rays or in certain cases, MRI or ultrasound, could be utilized in order to establish the cause and determine whether the condition is serious. illness.
- Therapy for Conservatives: Initially, both plantar fasciitis and bone spurs are usually treated with traditional techniques. This may mean rest or orthotic devices, physical therapy or anti-inflammatory drugs, as well as lifestyle changes.
It is important to remember that although these conditions have certain similarities, their root causes and the particular structures involved are distinct.
Bone spurs are the result of the growth of bony protrusions on bones that are already present, while plantar fasciitis is an inflammation condition that affects the plantar fascia which is a connective tissue found in the foot.
A proper diagnosis by a healthcare expert is vital to determine the cause and devise the appropriate treatment plan that is tailored to the needs of the patient.
Reference Books
Certainly, here are some reference books related to orthopedics, bone spurs, plantar fasciitis, and related subjects:
- “Campbell’s Operative Orthopaedics” by Frederick M. Azar, James H. Beaty, and S. Terry Canale
- A comprehensive reference book on orthopedic surgery, covering a wide range of topics including conditions, procedures, and techniques.
- “The Plantar Fasciitis Plan: Free Your Feet from Morning Pain” by Colin Dombroski
- A book that focuses on plantar fasciitis, offering insights into its causes, prevention, and various treatment options.
- “Orthopaedic Physical Therapy Secrets” by Jeffrey D. Placzek and David A. Boyce
- Provides insights into the physical therapy aspect of orthopedics, which is relevant to the rehabilitation and treatment of conditions like plantar fasciitis.
- “Orthopedic Physical Assessment” by David J. Magee
- A valuable resource for clinicians and students in physical therapy and orthopedics, offering guidance on assessing musculoskeletal conditions.
- “Atlas of Human Anatomy” by Frank H. Netter
- An anatomy atlas that provides detailed illustrations and explanations of the human body, including the musculoskeletal system.
- “Orthopedic Secrets” by Surena Namdari, Stephan R. Gunther, and Jeffrey A. Kalunian
- This book covers a wide range of orthopedic topics, including conditions, diagnostic approaches, and treatment options.
Conclusion
plantar fasciitis and bone spurs are distinct orthopedic conditions that have distinctive causes, symptoms, and treatment strategies. Differentiating between these two conditions is crucial to ensure a proper diagnosis and efficient treatment.
While they do share some similarities including heel discomfort and risk factors, their differences are in the root causes and diagnostic techniques. Consulting a medical professional is essential for an accurate diagnosis and a customized treatment with the intention of relieving pain, increasing mobility, and improving the quality of life overall.