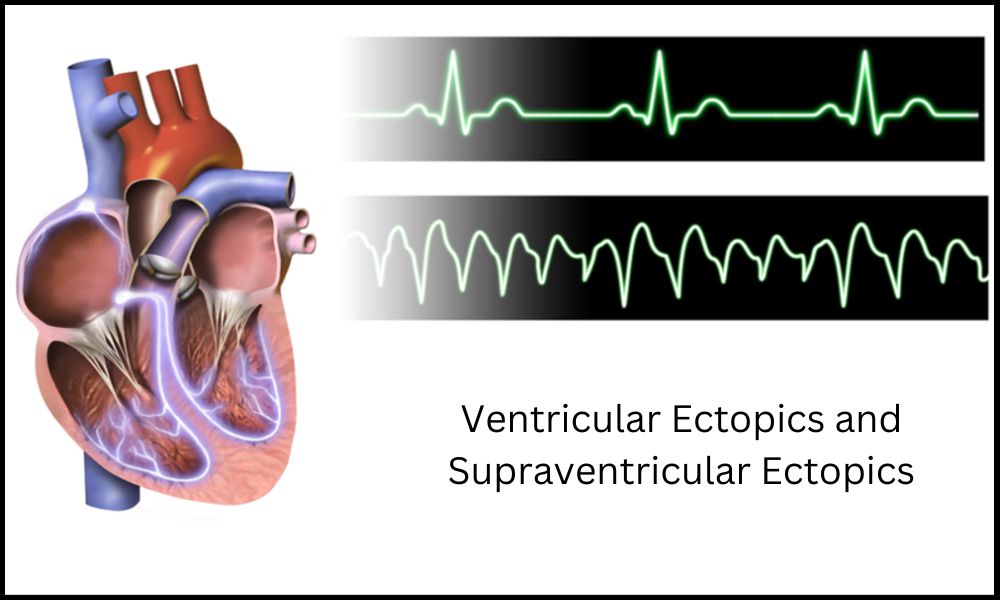
Introduction of Ventricular Ectopics and Supraventricular Ectopics
Ectopic beats are abnormal electrical impulses that disrupt the normal rhythm of your heart, known as arrhythmias. Ectopic beats may emanate from any location within your cardiovascular system and come in various types; two such forms include ventricular and supraventricular ectopics.
As it varies significantly in their origins, characteristics, diagnostic approaches, and treatment approaches, distinguishing between ventricular and supraventricular ectopics is vital to accurate diagnosis and appropriate management. Understanding their distinct differences allows physicians to provide accurate diagnoses and proper treatments.
Ventricular Ectopics
Ventricular ectopics, also known as premature ventricular contractions (PVCs), are abnormal electrical impulses originating in the ventricles of the heart. Normally, electrical signals originate at the sinus node (natural pacemaker) located in the right atrium and travel along specific pathways coordinating contraction of both atria and ventricles in unison.
Vessel Ectopics occur when an electrical signal prematurely triggers early contraction of one or both ventricles, disrupting their regular rhythm and producing an unexpected, “out-of-place” beat. Vessel Ectopics may occur either sporadically or clustered and their frequency varies from person to person.
Note that ventricular ectopics differ from sinus beats in that they originate in different locations (ventricles), with differing electrical properties than regular heart rhythms.
Supraventricular Ectopics
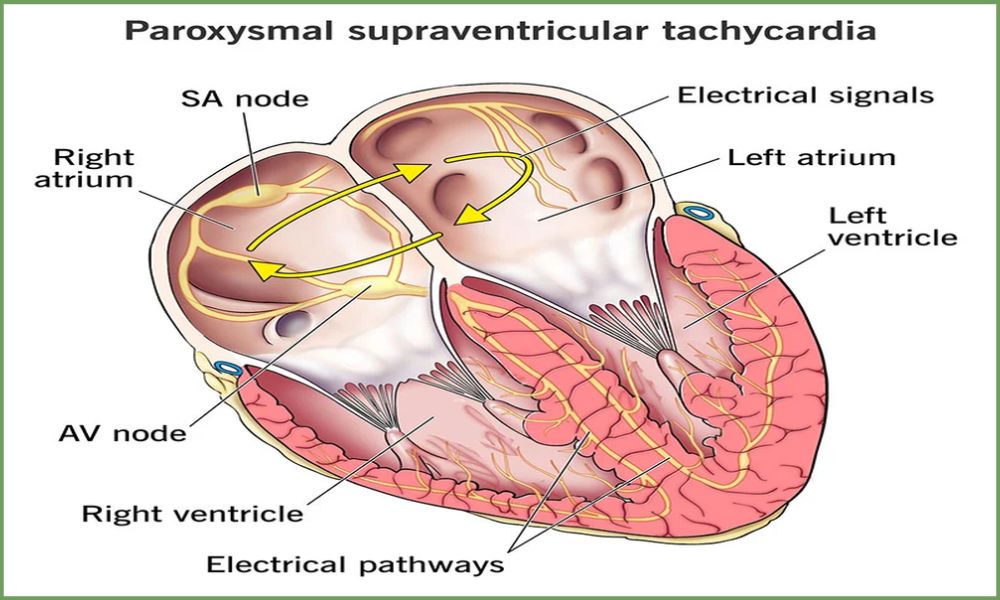
Supraventricular ectopics also referred to as premature atrial contractions (PACs) or premature supraventricular contractions (PVCs), are abnormal electrical impulses originating above the ventricles in the heart. While ventricular ectopics originate within each ventricle, supraventricular ectopics originate within other supraventricular structures like the atria or the AV node.
At its heart lies an ectopic beat, in which an electrical signal arrives early and causes early contraction of the atria, disrupting normal heart rhythm and producing an extra “out-of-place” beat. Supraventricular ectopic beats can occur intermittently or cluster throughout a day’s activity and their frequency varies according to individuals.
Supraventricular ectopic beats should be distinguished from regular sinus beats as they originate in a different location above the ventricles and possess different electrical characteristics compared to the typical heart rhythm.
Difference Between Ventricular Ectopics and Supraventricular Ectopics
Here’s a comparison table highlighting the key differences between ventricular ectopics and supraventricular ectopics:
| Aspect | Ventricular Ectopics | Supraventricular Ectopics |
|---|---|---|
| Origin | Arise from the ventricles | Arise from the atria, AV node, or supraventricular structures |
| ECG Characteristics | Wide QRS complex | Narrow QRS complex |
| Clinical Presentation | Palpitations, skipped beats, awareness of heartbeats | Palpitations, awareness of heartbeats |
| Associated Symptoms | Shortness of breath, dizziness, chest discomfort | Shortness of breath, dizziness, chest discomfort |
| Diagnosis | ECG, Holter monitor, event recorder | ECG, Holter monitor, event recorder |
| Underlying Causes | Heart disease, electrolyte imbalances, stimulants | Stress, anxiety, caffeine, medications, heart disease |
| Management | Lifestyle modifications, medications, ablation | Lifestyle modifications, medications, ablation |
| Prognosis | Generally benign, but can indicate underlying heart disease | Generally benign, but can indicate underlying heart disease |
| Risk of Complications | Higher risk of developing potentially life-threatening arrhythmias | Lower risk of developing life-threatening arrhythmias |
| Treatment Goals | Reducing frequency and severity of ectopic beats, addressing underlying causes | Reducing frequency and severity of ectopic beats, addressing underlying causes |
| Treatment Approaches | Beta-blockers, antiarrhythmic medications, catheter ablation | Beta-blockers, antiarrhythmic medications, catheter ablation |
It’s important to note that this table provides a general overview, and individual cases may vary. It is always recommended to consult with a healthcare professional for accurate diagnosis and personalized treatment recommendations.
Are they dangerous?
Ventricular and supraventricular ectopics pose different degrees of risk.
Here is an overview:
Ventricular Ectopics: Ventricular ectopics may be more concerning than supraventricular ectopics under certain circumstances. They could indicate heart conditions or structural abnormalities such as coronary artery disease, heart failure, or prior heart attack; frequent or sustained patterns like ventricular tachycardia could increase the risk for more serious arrhythmias such as ventricular fibrillation which can be life-threatening; while symptoms like palpitations, dizziness or fainting could arise as a result; so proper evaluation and management would reduce risks significantly and potentially reduce adverse events arising.
Supraventricular Ectopics: Supraventricular ectopics generally pose less of a risk than their ventricular counterparts, typically originating in the atria or atrium and often being benign in nature.
Supraventricular ectopics have been linked with anxiety, excessive caffeine intake, and heart diseases like mitral valve prolapse or atrial fibrillation. Although supraventricular ectopics may cause bothersome symptoms like palpitations, chest discomfort, or shortness of breath, they are generally not life-threatening or associated with serious complications.
If they become increasingly frequent or severe or lead to sustained rapid heart rates (e.g. supraventricular tachycardia), medical evaluation and management are still recommended for diagnosis and management purposes.
As the above information provides only an overall snapshot, individual cases may vary greatly. If you experience symptoms or have concerns regarding ectopic beats, it is recommended that you seek guidance from healthcare providers who can assess your individual circumstances and offer personalized advice and assistance.
Common causes of ectopic beats
Ectopic beats may have various causes, which vary depending on whether they are ventricular ectopics or supraventricular ectopics. Here are some potential reasons:
Ventricular Ectopics:
Heart Disease: Underlying heart Conditions such as coronary artery disease, Myocardial infarction (heart attack), heart failure, or Cardiomyopathy can increase the risk of Ventricular Ectopics.
Electrolyte imbalances: Low levels of Potassium, magnesium, or calcium in the blood can Compromise the heart’s Electrical system and cause Abnormal heartbeats to occur.
Medications and substances: Some medications such as beta-blockers, antiarrhythmic, and asthma medications can contribute to ventricular ectopic beats. Illicit drug use – such as stimulants like cocaine – may also trigger these abnormal beats.
Alcohol and Caffeine: Excessive consumption of alcohol and caffeinated beverages has been shown to contribute to ventricular ectopics in some individuals.
Emotional Stress and Anxiety: Emotions such as fear, worry, and stress can stimulate the release of stress hormones which in turn influence electrical activity in the heart and result in irregular heartbeats or even beats that don’t follow normal patterns.
Physical Factors: Overexertion, dehydration, fatigue or electrolyte imbalances associated with intense physical activity may increase the risk of ventricular ectopics.
Supraventricular Ectopics:
Atrial Conditions:
Certain atrial conditions such as atrial fibrillation, atrial flutter and atrial enlargement can increase an individual’s susceptibility to supraventricular ectopics.
Medications and substances: Some medications, like digitalis, may exacerbate supraventricular ectopics. Stimulants like caffeine and illicit drugs can also increase their likelihood.
Electrolyte imbalances: Electrolyte imbalances may also contribute to supraventricular ectopics; they occur when potassium, magnesium or calcium levels drop below certain thresholds and disrupt the heart’s electrical system leading to supraventricular ectopics.
Emotional Stress and Anxiety: Emotional stress and anxiety may also play a part in triggering supraventricular ectopics by altering heart electrical activity.
Metabolic conditions: Hyperthyroidism or adrenal gland abnormalities may increase the risk of supraventricular ectopics. f. Age-related changes: Supraventricular ectopics risk may increase with age, particularly among older adults.
As is true in most situations, these causes of ectopic beats are not exhaustive; individual cases may involve numerous contributing factors. If you experience or suspect ectopic beats or have concerns about them, seeking professional guidance for evaluation and guidance from healthcare practitioners is advised.
Catheter ablation
Catheter ablation is a minimally invasive procedure used to treat certain abnormal heart rhythms, including ectopic beats. This procedure is performed by cardiac electrophysiologist specialists who specialize in diagnosing and treating heart rhythm disorders. Here are some key points about catheter ablation:
Procedure Overview:
Before an ablation is performed, patients undergo a comprehensive evaluation process which may include electrocardiogram (ECG), Holter monitoring or electrophysiology studies (EPS). This helps pinpoint both the location and mechanism behind any ectopic beats present.
Catheter Insertion: This procedure involves inserting thin, flexible tubes called catheters into blood vessels via the groin area and directed towards the heart.
Mapping and Ablation: Specialized mapping techniques help locate the source of ectopic beats. Once identified, catheter-delivered energy – typically radiofrequency energy or cryotherapy – may be used to destroy or modify abnormal tissue that’s responsible.
Post-procedure: After ablation, catheters are removed and pressure applied to the insertion site to prevent bleeding. Patients will then be monitored for an indeterminate period before being released back home.
Purpose and Effectiveness:
Catheter ablation has been shown to be an effective treatment option for many patients who experience frequent or severe ectopic beats, by targeting and ablationing abnormal tissue that causes arrhythmias.
By targeting and treating this abnormal tissue directly, catheter ablation helps restore normal heart rhythm while relieving symptoms associated with arrhythmias. Catheter ablation has proven itself as an effective solution.
Risks and Complications: Although catheter ablation is generally safe, there may be risks and complications involved, including:
a. Bleeding or bruising at the catheter insertion site
b. Infection
c. Damage to blood vessels or heart structures
d. Blood clot formation
e. Nerve injury and
f. Recurrence or new arrhythmias.
Cardiac Perforation (rare but potentially serious complication)
Success Rate and Follow-up: The success rate of catheter ablation to treat ectopic beats may depend on many factors, including their cause, their location in relation to abnormal tissue, as well as an individual patient.
In some instances, one ablation procedure may successfully eliminate all ectopic beats; other times multiple procedures or additional treatments may be needed; follow up appointments are key in order to assess and modify treatment plans appropriately.
Consult with a healthcare provider in order to assess whether catheter ablation is an appropriate treatment option for you and any ectopic beats in your particular case. They can provide specific details regarding this process, discuss potential risks and benefits as well as address any concerns that may arise from the procedure.
Clinical presentation and symptoms
Individuals may experience different degrees of symptoms associated with both ventricular ectopics and supraventricular ectopics, and the exact nature and presentation may depend on an individual’s overall state. Here are the most frequently occurring presentations and symptoms:
Ventricular Ectopics:
Palpitations: Rapid or forceful heartbeats that may feel like rapid heartbeats with rapid, skipped or pounding sensations in the chest. b. Chest discomfort: Individuals may experience pressure, discomfort or pain during or following ventricular ectopic beats.
Ectopic beats may sometimes produce shortness of breath and difficulty in taking in oxygen, and can even lead to dizziness or lightheadedness; occasionally even syncope can result in temporary loss of consciousness (syncope).
Fatigue: Ectopic beats may contribute to feelings of general fatigue or decreased energy levels, while frequent or intense ventricular ectopics may increase anxiety by disrupting its rhythm and prompting greater concern from doctors about possible consequences on heart health.
Supraventricular Ectopics: Palpitations: Supraventricular ectopics can also produce irregular or rapid heartbeat sensations similar to their ventricular counterparts, with palpitations being the key symptom.
Fluttering or Pounding Sensation: Some individuals may experience a fluttering or pounding feeling in their chest during or following supraventricular ectopic beats.
Chest Aches: Mild discomfort, pressure or tightness in the chest may occur as well.
Shortness of Breath or Breathlessness: Ectopic beats from the atria or AV node can occasionally result in shortness of breath or breathlessness, while supraventricular ectopics may contribute to feelings of tiredness or fatigue.
Anxiety: Like their ventricular counterparts, supraventricular ectopics may also increase anxiety levels significantly.
As it’s important to keep in mind, some individuals may experience ectopic beats without experiencing any discernable symptoms, the severity and frequency of symptoms can also vary widely between individuals.
If you are concerned about or experience any symptoms related to ectopic beats it is strongly advised that you visit a healthcare professional for assessment and appropriate management in your particular case. They will offer personalized assessment as well as advice tailored specifically for you and your situation.
Diagnosis and diagnostic tests
Diagnostic criteria for both ventricular ectopics and supraventricular ectopics typically consist of reviewing patient history, physical exam, and conducting specific diagnostic tests. Here are some popular methods used to identify ectopic beats:
Patient History and Physical Exam:
A healthcare provider will ask about symptoms experienced, duration, frequency and potential triggers that have arisen over time.
Risk factor evaluation: Evaluate any preexisting heart conditions, prior heart events, family history, medication use or substance abuse history as well as lifestyle factors which may contribute to an ectopic beats condition.
Physical Examination: This includes a complete examination of the heart and other vital signs to assess overall cardiovascular health and identify any physical findings associated with cardiovascular illness.
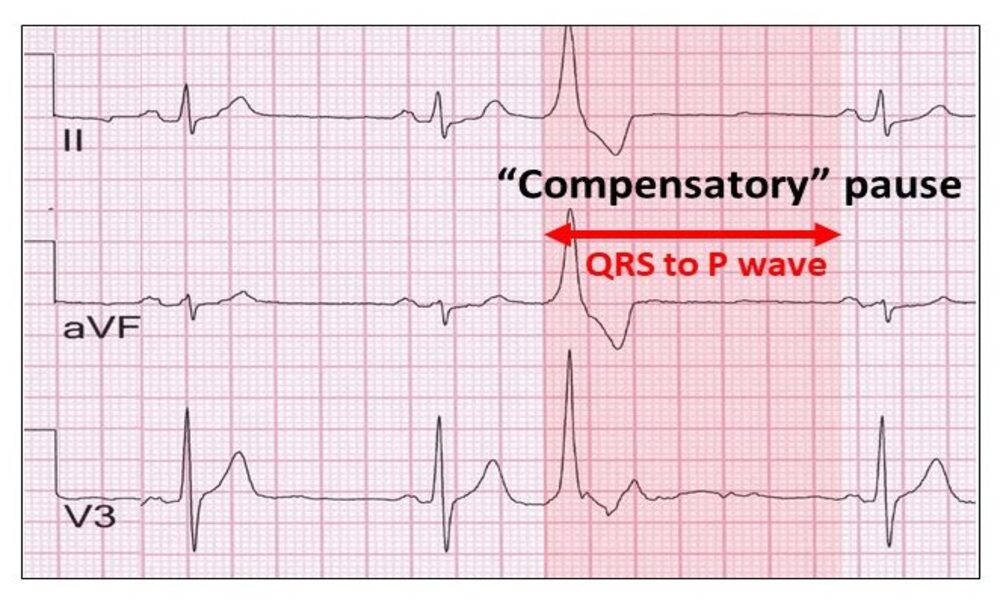
Electrocardiogram (ECG):
An ECG is a standard diagnostic test used to record the electrical activity of the heart. It can help identify the presence, frequency and specific characteristics of ectopic beats; however, due to their unpredictable nature they may require multiple ECGs or longer term monitoring to capture their occurrence.
Holter Monitoring: Holter monitoring involves wearing a portable device that continuously records your heart’s electrical activity for 24 to 48 hours or longer, providing more extended monitoring and an increased chance of capturing ectopic beats that may otherwise go undetected on an ECG test. Furthermore, this gives more comprehensive assessment of your heart rhythm over a longer timeframe.
Event Recorders:
An event recorder is a portable device that patients can activate when experiencing symptoms. This recording device captures heart’s electrical activity during episodes that cause symptoms, helping identify their type and source.
Echocardiogram: An echocardiogram is an ultrasound examination of the heart that provides detailed images of its structure, function, and blood flow. An echocardiogram can help identify any structural abnormalities or conditions such as valve disorders that could contribute to irregular heartbeats – as well as any that could potentially contribute to premature or ectopic beats.
Electrophysiology Studies (EPS): An EPS involves inserting catheters into the heart in order to assess its electrical signals and pinpoint any ectopic beats, often performed in cardiac electrophysiology laboratories. EPS may be particularly helpful when other diagnostic tests prove inconclusive or when an individual has increased risk for arrhythmias.
Diagnostic procedures depend on each person’s clinical presentation, suspected cause and healthcare provider’s judgement. When combined, these tests can help accurately diagnose, classify and determine treatment strategies for ventricular and supraventricular ectopics.
Consultation with healthcare professionals is vital in order to receive professional evaluation and advice tailored specifically for you and your circumstances.
Prognosis and potential complications
Prognosis for both ventricular ectopics and supraventricular ectopics varies based on several factors, including their source, frequency and severity of ectopic beats, presence of heart conditions and overall health status of an individual. Overall, prognosis tends to be positive when properly managed and treated; however, individual cases may differ and complications may occur in some instances; here are the potential complications and considerations:
Ventricular Ectopics:
mes Its mes serious arrhythmias such as ventricular tachycardia or fibrillation, which require medical intervention immediately – otherwise they can become life threatening and must be immediately treated with immediate medical intervention.
Impaired Cardiac Function: When frequent ventricular ectopics interfere with pumping function of the heart, cardiac output decreases significantly and symptoms of heart failure may arise.
Emotional Impact: Ectopic beats can have an emotionally devastating impact, often leading to increased anxiety, stress, or decreased quality of life for some individuals.
Complications related to an underlying cardiac condition: When ventricular ectopics result from an existing cardiac condition, their prognosis will depend on how that condition progresses and is managed.
Supraventricular Ectopics:
Its Symptomatic Burden: Repeated or frequent supraventricular ectopics may produce bothersome symptoms like palpitations, chest discomfort and shortness of breath that reduce quality of life for their victims.
Supraventricular Ectopics can have an impactful on daily activities; physical exertion or participation in certain activities may need to be limited out of concern that trigger or worsen an arrhythmia.
Risk of Other Arrhythmias: While supraventricular ectopics are generally considered less dangerous than their more dangerous counterparts, certain varieties such as supraventricular tachycardia can result in sustained or rapid arrhythmias that require medical intervention to control.
Underlying heart conditions: If supraventricular ectopics are linked with an underlying cardiac condition, their prognosis will depend on its progression and management.
As it’s important to remember, most individuals living with ectopic beats tend to enjoy good prognoses and can manage their symptoms and lower risk by seeking medical assistance, lifestyle modifications and intervention options such as catheter ablation. Routine follow ups with healthcare professionals are necessary in order to monitor condition progression and modify treatment plans as necessary.
As each case is unique and individual prognosis may differ significantly, it is wise to seek professional medical advice in order to obtain an in-depth evaluation and tailored prognosis based on your unique circumstances. For this purpose, healthcare providers provide evaluation services as part of a comprehensive assessment and personalized prognosis for their patients.
Similarities Between Ventricular Ectopics and Supraventricular Ectopics
Although ventricular and supraventricular ectopics are two distinct forms of abnormal heart rhythms originating from various areas within the heart, there are some similarities. Here are a few:
Origin: Both ventricular ectopics and supraventricular ectopics are considered ectopic beats, meaning that they originate outside the normal sinus node in the upper right atrium of the heart. Ventricular ectopics typically originate in the ventricles (lower chambers of the heart), while supraventricular ectopics originate in either the atrium (upper chambers) or attrioventricular (AV) node.
Abnormal Electrical Activity: Ectopic beats represent abnormal electrical activity in the heart, breaking its regular rhythm and potentially leading to palpitations or irregular heartbeats.
Clinical Presentation: Ventricular and supraventricular ectopics may present with similar symptoms, including palpitations, chest discomfort and shortness of breath. Furthermore, any sensation experienced during an ectopic beat could be identical regardless of its origin.
Triggers: Certain factors, including emotional stress, caffeine consumption, alcohol intake and medications may all aggravate both ventricular ectopics and supraventricular ectopics and lead to an increased rate of ectopic beats in either case. These triggers could exacerbate occurrence of these beats and accelerate their frequency further.
Diagnosis: Diagnosing both ventricular ectopics and supraventricular ectopics requires similar steps for diagnosis. Both conditions can be identified through patient history review, physical exam findings, ECG measurements (ECG or Holter monitoring), event recorders or Echocardiogram. Electrophysiology studies (EPS) may also be employed in order to further characterize and localize any possible ectopic beat sources.
Treatment Options: Treatment strategies for both ventricular ectopics and supraventricular ectopics have many similarities. In cases with infrequent or asymptomatic ectopic beats, no medical treatment may be required; lifestyle modifications like avoiding triggers like caffeine or alcohol could help.
Beta-blockers or antiarrhythmic medications could be prescribed to control symptoms or reduce frequency; catheter ablation could also be considered in more serious or refractory cases of either form of ectopic beats.
Important to keep in mind is the distinctions between these two forms of ectopic beats; while similar in appearance and mechanism, each has unique traits which require tailored diagnosis and management strategies based on its origins and causes. Seeking professional medical advice will help ensure accurate diagnosis and appropriate management based on your particular circumstances.
Summary
Ventricular and Supraventricular ectopic beats are two forms of irregular heart rhythms known as Ectopic beats that interfere with normal Electrical activity of the heart and are known as Abnormal heart rhythms.
Although they originate in different areas of the heart (ventricles for ventricular ectopics and atrium or AV node for supraventricular ectopics), there are similarities among them. Both types of ectopic beats can present with similar symptoms, including palpitations, chest discomfort and shortness of breath.