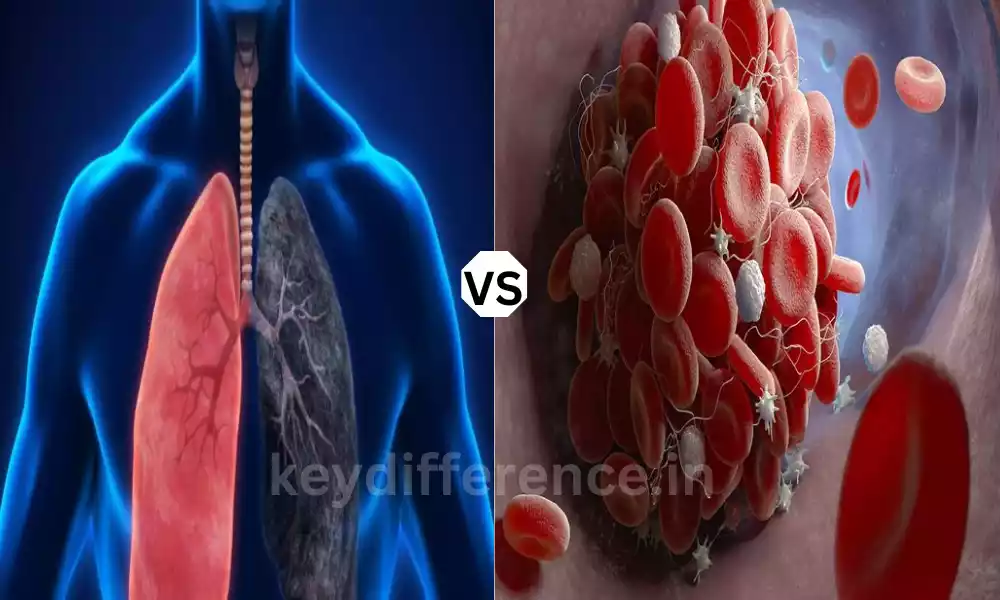
Pulmonary Embolism and Venous Thromboembolism are two medical conditions of extreme importance that are linked to blood clots. However, they differ in their causes and symptoms, diagnosis, and treatment.
Knowing the difference between these two conditions is crucial for a timely and effective treatment. The major distinctions between VTE and PE and VTE, provide information on the causes, symptoms, risks, diagnostics treatment, and prevention strategies.
What is Pulmonary Embolism?
Pulmonary embolism can be a life-threatening medical issue that is characterized by the sudden obstruction in one or several of the arteries that flow through the lung. The blockage is caused by an encasement of blood, usually formed in deep veins (a condition called deep vein thrombosis, or DVT) is released and moves through the bloodstream until it eventually is lodged in the pulmonary veins.
The blockage disrupts the normal flow of blood to the lungs, causing several symptoms such as chest pain, and difficulty breathing, and, in extreme instances, it may cause respiratory or circulatory failure. A prompt diagnosis and timely treatment are crucial to avoid future complications and ensure the health of the patient.

What is Venous Thromboembolism?
Venous Thromboembolism is a medical term that covers two related conditions such as deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT is the forming of blood clots (thrombi) in deep veins. Usually, they are found in the legs.
PE is when blood clots break up and move into the pulmonary arteries and cause blockages to the lung. The condition is a serious, potentially life-threatening disease. Its treatment and diagnosis usually are focused on stopping DVT from becoming PE because these two conditions have common risks and treatment strategies.
Knowing the causes of VTE is essential for successfully controlling the thromboembolic risks and complications.
Importance of distinguishing between PE and VTE
The distinction between Pulmonary Embolism (PE) and Venous Thromboembolism (VTE) is vital for a variety of critical reasons:
- Specific Treatment: Both VTE and PE require different treatment strategies. Both conditions require anticoagulant therapy, their treatment could differ greatly. An accurate diagnosis can ensure you receive proper treatment for your particular health issue.
- Risk assessment: Assessing whether or not a patient is suffering from DVT and the potential for PE is essential in determining their overall risk. Being aware of and addressing these risk factors quickly can help avoid more serious complications.
- Diagnostics: Both VTE and PE may have different prognoses. PE may be life-threatening, particularly in extreme cases, and prompt intervention is crucial. The recognition and differentiation between these conditions can affect the outcomes of patients.
- Methods to Prevent: Being aware of the type of condition present allows for individualized prevention strategies. For instance, in the event that DVT is found, actions are taken to avoid the progression of the clot to PE.
- Resource Allocation: A proper diagnosis will ensure health resources will be distributed effectively. It avoids the need for unnecessary testing as well as treatments for patients that don’t suffer from VTE or PE which reduces the cost of healthcare and the strain on healthcare systems.
- Patient education: People suffering from VTE must be aware of their condition and its risk factors. The distinction between the two conditions of PE and VTE will allow for better education of patients, allowing them to maintain their health and avoid any further complications related to clots.
- Data Analysis and Data Analysis: A precise distinction between VTE and PE within medical documents or research papers is crucial to conducting epidemiological research as well as evaluating the outcomes of treatment and in the development of new treatments.
Knowing the difference between VTE and PE is essential to ensure proper prompt medical intervention to reduce the risk of complications and improve the patient experience.
It also assists in the allocation of resources, research, as well as patient awareness, all of which contribute to more efficient healthcare management and improved public health overall.
Comparison Table of Pulmonary Embolism and Venous Thromboembolism
Here’s a comparison table highlighting the key differences between Pulmonary Embolism (PE) and Venous Thromboembolism (VTE):
| Aspect | Pulmonary Embolism (PE) | Venous Thromboembolism (VTE) |
|---|---|---|
| Definition | A blockage in the pulmonary arteries due to blood clots, often originating from DVT. | An umbrella term encompassing both DVT and PE, where DVT is the formation of blood clots in deep veins, typically in the legs. |
| Origin | Typically results from the migration of a clot from a deep vein, such as the legs. | Includes DVT as a primary component, with clots forming in deep veins. |
| Clinical Presentation | Sudden onset of symptoms, including chest pain, shortness of breath, cough, hemoptysis, syncope, tachycardia, and hypotension. | DVT symptoms (swelling, pain, warmth, redness) and PE symptoms (as described under PE). |
| Risk Factors | Previous DVT or PE, surgery, immobility, trauma, cancer, and pregnancy. | Shared risk factors with PE and additional factors like obesity, smoking, and hormone therapy. |
| Diagnostic Methods | Imaging (CT pulmonary angiography, V/Q scan) and D-dimer blood test. | Imaging (Doppler ultrasound for DVT) and D-dimer blood test. |
| Treatment | Anticoagulant therapy (heparin, warfarin), thrombolytic therapy (severe cases), and IVC filters in some situations. | Anticoagulant therapy, compression stockings, and leg elevation (for DVT), surgery, or interventional procedures (specific cases). |
| Prognosis and Complications | Prognosis varies based on severity; complications may include pulmonary infarction and chronic pulmonary hypertension. | DVT can lead to PE, and chronic complications may result in post-thrombotic syndrome. |
| Prevention | Prophylactic anticoagulation in high-risk situations and early mobilization after surgery. | Prevention of DVT through anticoagulation, compression stockings, lifestyle modifications, and risk factor management. |
This table summarizes the key distinctions between PE and VTE, emphasizing their definitions, origins, clinical presentations, risk factors, diagnostic methods, treatment approaches, prognoses, and prevention strategies.
Understanding these differences is essential for healthcare professionals to provide the appropriate care and for patients to be aware of their condition and associated risks.
Symptoms and Clinical Presentation
We will certainly look into the clinical manifestations and symptoms of Pulmonary Embolism (PE) and Venous Thromboembolism (VTE), specifically deep vein thrombosis (DVT) which is a part of VTE.
Pulmonary Embolism (PE):
- Rapid Onset: PE is often seen with an abrupt onset of symptoms.
- Respiratory Signs and symptoms: Common respiratory symptoms comprise:
- Breathing difficulty or shortness of breath. breathing.
- Chest pain that may get worse with deep breathing (pleuritic chest discomfort).
- Rapid breathing and an increased heart rate (tachycardia).
- Cough: Certain people with PE might have a dry or productive cough.
- Hemoptysis: In certain instances, coughing up blood (hemoptysis) could occur.
- Syncope A twitching (syncope) is a symptom of a more severe PE.
- The symptoms of circulatory disease: Severe PE can cause:
- Blood pressure that is low (hypotension).
- Cyanosis (bluish discoloration of lips or skin) because of low oxygen levels.
Venous Thromboembolism (VTE) which includes DVT:
Deep Vein Thrombosis (DVT):
- The swelling: Affected limb typically the leg might get swelling. The swelling could be sudden or gradual.
- pain: DVT can cause pain in the affected region and may persist or increase when you move.
- Warmth: Affected areas may feel warm to the contact.
- The redness: Skin discoloration or redness around the affected vein could be possible.
- Tendency: The affected area tends to be a bit tender.
- Calf Pain: The development of DVT within the muscles in the calf can cause the calf muscles to hurt.
It’s important to note that not all patients with PE or VTE exhibit the same symptoms and their severity may vary. Certain cases could be asymptomatic or have symptoms that are unusual. A prompt medical examination is essential for a correct diagnosis and proper treatment.
Surgery or interventional procedures for specific cases
Absolutely it is possible to use them for each Pulmonary Embolism (PE) and Venous Thromboembolism (VTE), especially deep vein thrombosis (DVT) surgical or other interventional procedures could be considered in some instances where standard medical treatment options are not sufficient or there is a chance of serious complications.
Here’s a brief overview of the scenarios in which the procedures could be utilized:
Pulmonary Embolism (PE):
- Embolectomy: If you have severe PE, with a huge hemodynamic instability and burdened by clots the surgical procedure called embolectomy can be carried out. When performing an embolectomy, the surgeon will remove the clot from pulmonary arteries in order to bring blood flow back to the lung.
- Catheter-Directed Thrombolysis: This procedure requires using a catheter to administer the clot-dissolving drugs (thrombolytics) directly into pulmonary blood vessels. It’s used in submassive and massive PE cases in which there is an extensive clot burden but with less hemodynamic instability.
- IVC Cava (IVC) Filter: in certain instances where anticoagulant therapy is not recommended or when a patient is suffering from persistent PE, regardless of treatment with an IVC filter could be put in. The device is placed inside the vena cava, which is designed to prevent blood clots prior to they enter the lung.
Venous Thromboembolism (VTE) and DVT:
- Thermotherapy: Thrombectomy is a surgical procedure to remove blood clots in deep veins in the case of massive and severe DVT. It is typically thought of when the clot is massive, leading to major obstruction and the risk of complications.
- Catheter-Directed Thrombolysis: Similar to the way it is used for PE, catheter-directed thrombolysis may be used to treat DVT. A catheter can be used to direct thrombolytic medication into the clot in order to dissolve it.
- Venous Stenting: In some instances in which there is persistent vein obstruction caused by DVT, it is possible to have a venous stent placed to ensure that the vein is open and increase the flow of blood.
It’s crucial to understand that both procedures have their own advantages and risks and their usage is determined on a case-by-case basis. The decision to undergo intervention or surgery is taken after careful analysis of the health status of the patient how severe the illness and the possible negatives and risks that the process may bring.
The patient and the healthcare provider team up to determine the best treatment approach to achieve the best outcomes while minimizing risk.
Prophylactic anticoagulation in high-risk situations
Prophylactic anticoagulation also referred to as thromboprophylaxis is a preventive medical procedure that involves the use of anticoagulants to lower the risk of blood clots forming particularly in high-risk scenarios where the possibility of VTE (VTE) is increased.
Here are a few situations in which prophylactic anticoagulation is frequently used:
- Surgery: patients who are undergoing major operations, including orthopedic procedures such as knee and hip replacements are at a higher likelihood of contracting VTE due to inactivity and surgical trauma. Prophylactic anticoagulation is typically given prior to and following surgery to avoid the formation of clots.
- Hospitalization: People who have been admitted to hospitals, particularly those with limited mobility, serious illness, or medical illnesses are at greater risk danger of contracting VTE. Anticoagulation therapy for prevention is often recommended to decrease the risk.
- medical conditions: Patients with certain medical issues, for example, active heart failure, cancer, or serious infections, are at an increased risk of developing VTE. Anticoagulation therapy for prevention is a possibility in these situations.
- Pregnancy and Postpartum period: Pregnant women and women who are postpartum are more at risk of developing clots. Prophylactic treatment with anticoagulants is recommended particularly for those with risk factors other than those mentioned above.
- Long-Distance Travel: Inactivity for long periods when traveling long distances (e.g. long-haul flights) can increase the chance of clot development, which is commonly known as “economy class syndrome.” Some people may take anticoagulants prophylactically after consulting with a healthcare medical professional.
- Inherited or acquired Thrombophilia: People with known medical or genetic conditions that increase the risk of clotting could receive anticoagulation prophylactically in times of increased risk, for example during pregnancy or surgery.
- Immaturity: Long periods of inactivity, like in bed for a long time or following a serious injury, may cause stagnation of blood within the veins, thereby increasing the risk of blood clot formation. Anticoagulation treatment can be administered as a preventative to reduce the risk.
It’s crucial to understand that the decision to utilize prophylactic anticoagulation is made based on an in-depth assessment of the person’s general health medical history, as well as particular risk factors.
The kind of anticoagulant, dosing regimen, as well as time frame for prophylaxis, can differ depending on the specific situation and specific patient characteristics.
Patients must consult with their healthcare providers to decide on the best method of thromboprophylaxis. the advantages of the prevention of VTE should be carefully evaluated against potential risks, like bleeding complications that can result from the use of anticoagulants.
Prevention of DVT through anticoagulation, compression stockings
The prevention of deep vein Thrombosis (DVT) can be vital, particularly for those at risk. There are a number of prevention measures, including anticoagulation and compression stockings.
- Anticoagulation (Blood Thinners): Anticoagulant medications are frequently used to treat DVT for those at high risk like those who undergo major surgery, trauma patients, or those suffering from certain medical ailments. The most commonly used anticoagulants are heparin and low molecular-weight Heparin. They work by reducing the ability of blood to get clots. The choice of anticoagulant as well as the time of treatment will be contingent on the risk factors specific to your situation and the individual characteristics of the patient.
- Comprise Stockings: Gradually-shaped compression socks are specifically designed to offer an external force to the legs which is beneficial for greater blood flow and stopping blood from accumulating in the veins. They are especially beneficial for those who are at risk of DVT due to inactivity, like patients who are in hospital or who travel long distances. Compression stockings are available at various pressure levels. The decision to choose the right level of pressure must be made under the supervision of a health expert.
- Mobility and Exercise: Maintaining a healthy lifestyle and avoiding prolonged periods of motion is vital to DVT prevention. For instance, those who are recovering from surgery are advised to get up and walk as quickly as they can. For long-distance travel it is recommended to stop for breaks, stroll around the cabin, and do ankle and calf exercises to keep blood circulation.
- Hydration: A healthy diet can keep blood from becoming thick and clotting easily. This is particularly vital during long trips in which passengers can be dehydrated because of the dry climate and lack of accessibility to liquids.
- Healthier Lifestyle: Living a healthier lifestyle, with healthy eating, regular exercising, and not smoking cigarettes, can lower the risk of DVT. Smoking, particularly is a risk factor for clotting.
- Medication Adjustment: People who are taking hormonal replacement therapies or oral contraceptives could be more susceptible to DVT. If additional risk factors are present, medical professionals might suggest adjusting or stopping these drugs.
- Compression devices: In specific clinical situations IPC devices are used intermittently. (IPC) devices could be employed. They are mechanical devices that are used to periodically inflate and deflate cuffs on the legs to increase the flow of blood through the venous system.
It’s crucial to remember that DVT prevention strategies must be customized based on the individual’s risk factors as well as their general health.
Any decision to make use of compression stockings anticoagulants, or other preventive measures, should be discussed with a physician to determine the most suitable and secure method.
Similarities Between Pulmonary Embolism and Venous Thromboembolism
Pulmonary Embolism (PE) and Venous Thromboembolism (VTE) have many similarities due to their interconnected nature:
- Clot Formation: Both VTE and PE result in the creation of blood clots. For PE the clot usually originates within the deep veins of the human body (DVT) and is then transported through the pulmonary arteries, which can cause obstruction. VTE however is a broad term that encompasses both DVT and PE.
- Origins of DVT: In most instances, PE is a result of deep vein thrombosis (DVT). DVT is a kind of VTE which means that PE is in essence the result of VTE.
- Risk Factors: Many risk factors for PE are common with VTE. The risk factors are prior experience with DVT (or PE), surgeries and immobility, cancer obesity, pregnancy, and certain medical ailments. Therefore, identifying and addressing the risk factors is essential for both conditions.
- D-dimer Testing: Blood tests for D-dimer can be utilized to assist in diagnosing both VTE and PE. A higher level of D-dimer may suggest the presence of blood clots.
- Anticoagulation Therapy: The treatment for VTE and PE often requires anticoagulant treatment to prevent any further clot formation, and also to lower the chance of complications. Treatments such as heparin and warfarin are frequently used to treat both ailments.
- Prevention measures: Similar preventive measures are used to lower the risk of PTE as well as VTE. These include anticoagulation prophylactics in situations of high risk and compression stockings that help increase blood flow to the legs, as well as early mobilization following surgery.
- Possibility of Complications: Both PE and VTE can cause serious complications, including chronic hypertension to the lungs as a result of PE, and post-thrombotic syndrome in the case of VTE.
Although there are a lot of similarities between PE and VTE, it is crucial to understand this fact: VTE is a broad term that includes a range of thromboembolic conditions, such as DVT or PE. Recognizing the particular condition and its specific characteristics is vital for successful diagnostics and treatments.
Conclusion
Pulmonary Embolism (PE) and Venous Thromboembolism (VTE) are connected conditions, with common risks, diagnostic methods, and strategies for prevention. PE is usually an underlying complication of VTE and, in particular, deep vein thrombosis (DVT).
Knowing the distinctions between them in terms of clinical presentation and the specific treatment options is crucial in order for health professionals to offer precise care as well as for patients to effectively manage their health.
Early diagnosis, proper treatment, and prevention strategies are crucial to improving patient outcomes and decreasing the chance of developing these life-threatening illnesses.