Introduction
Epilepsy is a neurological disorder characterized by frequent and unpredictable seizures that can have many causes; two common classifications for these seizure types are “idiopathic and cryptogenic epilepsies”, which should help guide diagnosis, treatment decisions, and management strategies. Understanding their differences is vital to accurate diagnosis, effective treatments plans and management strategies.
We will explore the distinctions between idiopathic and cryptogenic epilepsy. Idiopathic epilepsy refers to forms of epilepsy in which the cause for seizures cannot be established through available diagnostic methods; on the other hand, cryptogenic epilepsy implies a possible but unconfirmed cause that remains hidden or elusive despite efforts at diagnosis.Characteristics, causes, diagnostic approaches, treatment options, and long-term outcomes associated with both idiopathic and cryptogenic epilepsy.
Furthermore, it will detail key differences between them, including their respective etiologies, challenges associated with diagnosis, prognoses and prophylactic considerations. Finally, recognising similarities and overlapping features between them will also be covered to offer a complete picture of these conditions.
Healthcare professionals and those affected by epilepsy alike can make more informed decisions regarding diagnosis, treatment and management, ultimately increasing quality of life for those living with epilepsy. Furthermore, ongoing research and advancements within this field will be highlighted to showcase our ever-expanding understanding and approach towards these conditions.
Definition of Idiopathic Epilepsy
Idiopathic epilepsy refers to a form of epilepsy wherein its cause remains unidentified or cannot be ascertained using currently available diagnostic methods. Epilepsy without apparent causes refers to any form of epilepsy where no clear structural, metabolic, or genetic abnormalities can be identified as the source of seizures.
Idiopathic epilepsy, also referred to as primary or essential epilepsy, does not result from any specific medical condition or brain injury and typically diagnosed after all potential causes for seizures have been eliminated through thorough medical testing and evaluation.
“Idiopathic” refers to epilepsies with no identifiable causes that arise spontaneously without apparent reason, yet does not imply they are benign or less severe than other types of epilepsies. It serves as a descriptive term that categorizes them.
Definition of Cryptogenic Epilepsy
Cryptogenic epilepsy refers to a type of epilepsy in which its cause cannot be definitively established through existing diagnostic tools. Cryptogenic epilepsy differs from idiopathic epilepsy in that its cause remains unidentified, suggesting there could be something hidden or obscure that is hard to pinpoint using current medical knowledge and technology.
Assuming there may be an underlying structural, metabolic or genetic abnormality responsible for seizures but that this cannot be pinpointed or diagnosed definitively, this means seizures cannot be diagnosed conclusively or identified.
Cryptogenic epilepsy falls under the category of symptomatic epilepsy and indicates an underlying condition or factor contributing to seizures even though its source remains elusive or undetectable. The term “cryptogenic” comes from Greek word kryptos, meaning hidden or concealed; reflecting how difficult it can be to pinpoint its exact cause in these instances.
Comparison Table of Idiopathic and Cryptogenic Epilepsy
Sure! Here’s a comparison table highlighting the key differences between idiopathic and cryptogenic epilepsy:
| Aspect | Idiopathic Epilepsy | Cryptogenic Epilepsy |
|---|---|---|
| Definition and Categorization | Epilepsy with no identifiable cause or underlying brain abnormality | Epilepsy with an unknown cause or presumed underlying brain abnormality |
| Etiology and Underlying Causes | No known specific cause; genetic factors may play a role | Presumed underlying brain abnormality or structural abnormalities, but the exact cause is unknown |
| Diagnostic Challenges and Approaches | Relatively straightforward diagnosis as there is no identifiable cause | Diagnostic challenges due to the need for extensive testing to identify the presumed underlying cause |
| Clinical Presentation and Symptoms | Varied presentation depending on the specific type of idiopathic epilepsy | Varied presentation depending on the presumed underlying cause or associated structural abnormality |
| Diagnosis | Based on clinical evaluation, medical history, EEG findings, and ruling out other possible causes | Comprehensive evaluation including medical history, physical examination, neurological tests, imaging studies (MRI, CT scan), and EEG findings |
| Treatment Options | Antiepileptic medications are the mainstay of treatment | Antiepileptic medications are the primary treatment, but surgical interventions may be considered for cases with identified structural abnormalities |
| Prognosis and Outcomes | Generally favorable prognosis with good seizure control and minimal impact on daily functioning | Prognosis varies depending on the underlying cause or associated structural abnormality; outcomes may be influenced by the success of treatment |
| Examples of Types | Childhood absence epilepsy, Juvenile myoclonic epilepsy, Benign rolandic epilepsy | Temporal lobe epilepsy, Frontal lobe epilepsy, Occipital lobe epilepsy |
Note: This comparison table provides a concise overview of the main differences between idiopathic and cryptogenic epilepsy. Additional points can be included based on specific aspects or types of epilepsy you wish to focus on.
Importance of understanding the differences between Idiopathic and Cryptogenic Epilepsy
Understanding the differences between idiopathic and cryptogenic epilepsy are of utmost importance for various reasons:
Accurate Diagnosis: Healthcare professionals need to distinguish between idiopathic and cryptogenic epilepsy to provide accurate diagnoses to their patients, which allows for effective treatment strategies and management plans to be put in place. Any misdiagnosis or delayed diagnosis could lead to ineffective or inappropriate treatments – further worsening their condition.
Treatment Planning: Idiopathic and cryptogenic epilepsy may require different approaches for their management, with antiepileptic medication tailored specifically for each type of epilepsy often being enough.
Conversely, cryptogenic forms may necessitate additional measures like surgical resection or alternative therapies like ketogenic diet. Understanding the source of epilepsy helps identify an effective plan that optimizes seizure control while improving quality-of-life for individual patients.
Prognostic Indications: Long-term outcomes can differ depending on whether one has idiopathic or cryptogenic epilepsy, especially among its subtypes. Idiopathic epilepsy tends to respond better to medication and may outgrow seizures over time; cryptogenic epilepsy, on the other hand, may have less predictable course and be caused by brain abnormalities or structural lesions in certain instances; differentiating between them provides insights into expected course and can inform prognosis discussions with patients and their families.
Research and Advancements: Recognizing the differences between idiopathic and cryptogenic epilepsy contributes to ongoing research and advancements within this field. By understanding its causes and mechanisms, understanding its cause-and-effect relationship could lead to targeted therapies and personalized medicine approaches that target epilepsy symptoms directly; furthermore it helps in the identification of genetic factors as well as risk factors, preventive measures and improved diagnostic techniques.
Patient Education and Support: Communication and patient education are paramount when living with epilepsy. Understanding whether it is idiopathic or cryptogenic can provide patients and their loved ones with more insight into its nature, possible causes and treatment options, enabling them to make more informed healthcare decisions while actively taking part in managing their epilepsy management.
Understanding the differences between idiopathic and cryptogenic epilepsy is essential to accurate diagnosis, effective treatment planning, prognostic considerations, research advances, patient education and support services as well as improving overall care outcomes for people living with epilepsy.
Genetic factors and inheritance patterns
Genetic factors play an integral part in both idiopathic and cryptogenic epilepsy. Here are a few key points Related to Genetic inheritance patterns:
Idiopathic Epilepsy:
Genetic Susceptibility: It is thought that Idiopathic epilepsy has an Inherent genetic Component, with Predisposition for seizures Inheritable within Families.
Polygenic Inheritance: Polygenic inheritance is considered a complex genetic disorder in which numerous genes, each having small effects, play an integral part in creating the condition.Genome-wide Association Studies (GWAS) have identified several genetic variants linked with specific forms of idiopathic epilepsy, such as childhood absence epilepsy, juvenile myoclonic epilepsy and generalized epilepsies.
Clustering: Idiopathic epilepsy may appear in several family members at once, suggesting an inherited pattern of inheritance.
Cryptogenic Epilepsy:
Underlying Genetic Causes: Cryptogenic epilepsy can often have identifiable genetic roots, including mutations or structural changes to the brain.
De Novo Mutations: Cryptogenic epilepsy may also result from de novo (new) genetic mutations that don’t pass down from parents but arise spontaneously during early development.
Structural Variants: Structural variants found within a genome, such as chromosomal rearrangements or copy number variations (CNVs), may contribute to cryptogenic epilepsy development.
Genetic Testing: Testing such as targeted gene sequencing, chromosomal microarray analysis and whole exome sequencing may help detect specific genetic abnormalities associated with cryptogenic epilepsy.
With regard to inheritance patterns:
Idiopathic Epilepsy: Autosomal Dominant Inheritance: mes Certain forms of idiopathic epilepsy, such as familial temporal lobe epilepsy and certain benign familial neonatal epilepsies, follow an autosomal dominant inheritance pattern. This means that if one parent carries a gene mutation associated with this condition, there is a 50/50 chance they pass it along to each child they have.
Autosomal Recessive Inheritance: Certain rare forms of idiopathic epilepsy show autosomal recessive inheritance patterns; both parents must carry a gene mutation for it to pass down through generations.
Cryptogenic Epilepsy:
Inheritance patterns of cryptogenic epilepsy vary significantly and depend on its underlying genetic cause or structural abnormality. Some cases may follow autosomal dominant or recessive patterns while others could occur spontaneously through de novo mutations.
Common types of idiopathic epilepsy
There are various idiopathic epilepsy types, each distinguished by distinct clinical symptoms and seizure patterns. Here are some notable types:
Childhood Absence Epilepsy (CAE):
Age of Onset: Most commonly apparent between 4-8 years of age.
Seizure Characteristics: Seizures typically display as brief but frequent absence seizures that cause staring blankly or temporarily losing awareness in children.
EEG Findings: Electroencephalogram (EEG) scans may reveal a characteristic 3 Hz spike-and-wave pattern on EEG scans, indicative of CAE.
Prognosis: CAE generally has an excellent prognosis, with most children outgrowing seizures by the time they become adolescents.
Juvenile Myoclonic Epilepsy (JME): JME involves multiple seizures occurring simultaneously that cannot be stopped with medication alone and usually resolve over time.
Age of Onset: Epilepsy typically appears during puberty in adolescents, typically beginning around age 11. Seizure Features: Myoclonic Jerks (brief muscle contractions that typically affect upper bodies), and generalized tonic-clonic seizures (grand mal seizures).
EEG Findings: EEG findings can indicate specific patterns such as polyspike-and-wave discharges.
Prognosis: Joint Mobility Encephalopathy is typically lifelong condition; however, with effective treatments and management strategies seizure control can often be attained in most cases.
Benign Rolandic Epilepsy (BRE), more commonly referred to as Rolandic Epilepsy with Centrotemporal Spikes:
Age of Onset: Onset usually occurs between 3-13 years.
Seizure Characteristics: Focal seizures typically impacting facial and mouth muscles can result in drooling, speech difficulties and sometimes even facial or tongue twitching.
EEG Findings: Centrotemporal spikes (also called rolandic spikes) on EEG recordings are characteristic of BRE. mes Prognosis: Generally, BRE has an uneventful course, typically clearing by the time of adolescence.
Genetic Generalized Epilepsies (GGE): These genetic generalized epilepsies tend to resolve themselves over time as seizures abate over time.
Description of Idiopathic Epilepsy and Generalized Seizures (IDEGTS): This category refers to various idiopathic epilepsy syndromes with genetic roots and generalized seizures. Seizure Characteristics: Typically include different seizure types such as absence seizures, myoclonic seizures, and generalized tonic-clonic seizures.
EEG Findings: EEG findings typically include generalized spike-and-wave discharges or polyspike-and-wave discharges. Prognosis: Prognosis for GGE spectrum disorders can vary, although most individuals can achieve good seizure control with appropriate treatments.
Noting the changeability of epilepsy syndrome classification and terminology over time, as new research emerges. Therefore, for an accurate diagnosis and classification of idiopathic epilepsy based on current diagnostic criteria and terminology. it is highly advisable to seek professional advice.
Clinical presentation and symptoms
Clinical features and symptoms associated with idiopathic epilepsy vary based on its particular form. Below are some commonly-observed features and symptoms associated with it:
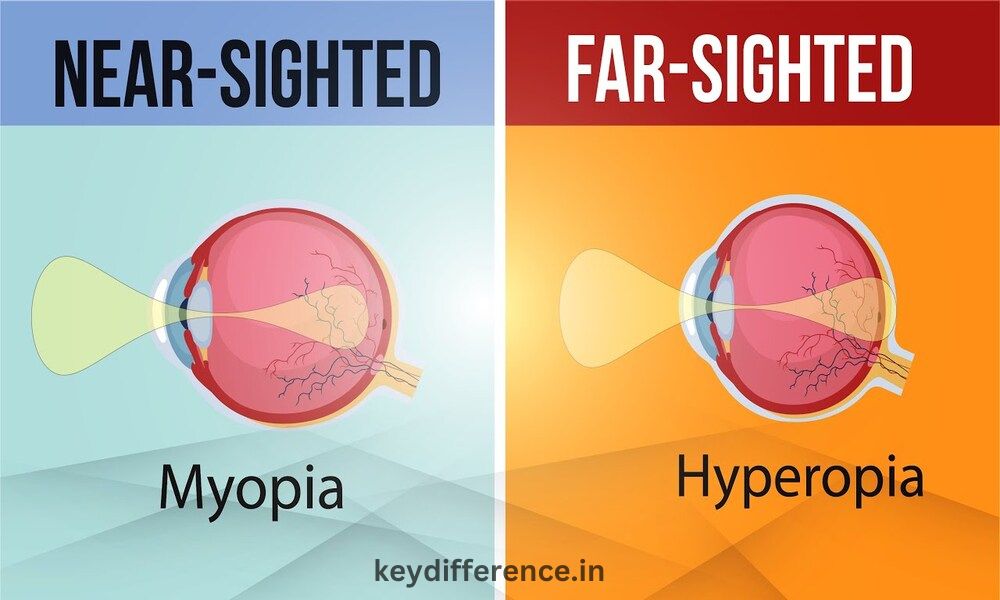
Absence Seizures: These seizures involve brief episodes of altered consciousness or staring spells with sudden on and off events that involve lack of awareness during seizure onset and off, no convulsions or loss of muscle tone occurring, and with no lasting ill effects afterwards.
Rapid Recovery and Resumption of Normal Activities After Seizures Its Myoclonic Seizures: Sudden, brief and involuntary muscle contractions or jerks which typically affect upper body areas like arms, shoulders or facial structures and can occur several times throughout a single day or more frequently. Indiferent if clustered together or occurring randomly.
Generalized Tonic-Clonic Seizures: These seizure episodes often result from fatigue, sleep deprivation or emotional stress. Ideally these seizures should only last minutes before concluding their attack.
Grand Mal seizures involve all the body. They usually start with sudden loss of consciousness and progress into stiffening and jerking movements of muscles (tonic phase) before progressing into loss of bladder or bowel control and excessive salivation or tongue biting, followed by generalized stiffening (tonic phase) before finally dissolving into full-scale seizures with limited control over either.
Postictal phase: After having experienced a seizure, one may experience confusion, drowsiness and muscle soreness in its aftermath. Focal Seizures: These seizures originate in one area of the brain.
Brain damage can have various symptoms depending on which area it affects, from abnormal sensations (tingling or numbness) to repetitive movements like chewing or lip smacking, altered consciousness and behavioral changes.
Focal seizures may progress into generalized seizure if they affect more of the brain. Other Possible Symptoms: Aura: People may notice warning signs (an aura) before experiencing a seizure such as smells, tastes, or visual disturbances before it happens.
Cognitive and Behavioral Issues: Epilepsy can adversely impact cognitive abilities, memory, attention, and behavior in its effects on seizures. When seizures become uncontrollable or frequent enough, seizures can negatively alter these functions as well as behavior patterns and affect learning abilities, memory storage capacity, attention span and behavior patterns.
Comorbid Conditions: Idiopathic epilepsy often co-occurs with other medical issues, including attention deficit hyperactivity disorder (ADHD), anxiety, depression, or developmental delays.
Epilepsy symptoms and severity can vary widely from individual to individual, even among those suffering from the same type of idiopathic epilepsy. An evaluation by healthcare professionals specializing in epilepsy is critical in accurately diagnosing and identifying each person’s unique epilepsy symptoms and presentation.
Challenges in distinguishing between idiopathic and cryptogenic epilepsy
Differing idiopathic from cryptogenic epilepsy can present significant difficulties due to the overlap in characteristics and the complexity of both conditions. Below are some key challenges encountered during this differentiation process:
Lack of Definitive Diagnosis Criteria: Unfortunately, neither idiopathic or cryptogenic epilepsy have clearly defined diagnostic criteria that are universally accepted. Epilepsy syndrome classification continues to change as new types are identified – making it challenging to establish clear boundaries between them.
Diagnostic Uncertainty: Determining the root cause of epilepsy can be challenging; many cases exhibit mixed or ambiguous features. Cryptogenic epilepsy refers to cases in which an underlying cause has not been definitively identified; thus causing diagnostic uncertainty that blurs the lines between idiopathic and cryptogenic epilepsy.
Interleaving Clinical Presentations: Clinical presentations and seizure types may overlap between idiopathic and cryptogenic epilepsy, for instance focal seizures initially appearing to be unrelated but later turning out to have an underlying cause upon further investigation. This complication makes differentiation more challenging.
Evolving Understandings: Our knowledge of the causes and mechanisms of epilepsy is ever evolving, with genetic discoveries and advances in diagnostic techniques leading to changes in classification of certain cases that were once labeled as “idiopathic epilepsy”, creating new opportunities for further research into this condition, potentially blurring the lines between idiopathic and cryptogenic epilepsy.
Diagnostic Limitations: EEG and neuroimaging tools may have their own set of shortcomings when it comes to pinpointing epilepsy’s underlying causes, with subtle brain abnormalities or genetic factors not always easily detectable, leaving diagnostic uncertainty open-ended. Furthermore, some genetic mutations linked to epilepsy might not be detectable through standard testing methods.
Individual Variability: Epilepsy is an individual condition and its root causes and clinical manifestations may differ widely between patients. This variability increases diagnostic complexity and makes categorizing epilepsy cases into distinct groups difficult.
To address these obstacles, a multidisciplinary evaluation team comprised of neurologists, epileptologists, geneticists and neuroimaging specialists may be necessary.
Advanced diagnostic techniques like genetic testing, high-resolution neuroimaging and long-term video EEG monitoring may assist in distinguishing between idiopathic and cryptogenic epilepsy by detecting genetic abnormalities or subtle brain anomalies; yet accurate diagnosis remains key to providing appropriate care and providing proper guidance when considering treatments decisions and care planning for individuals with epilepsy.
Benefits of tailored treatment plans based on accurate diagnosis
Individualized epilepsy treatment plans based on an accurate diagnosis offer numerous advantages for those living with the condition.
Here are a few key advantages:
Optimized Treatment Approach: With accurate diagnosis comes an enhanced treatment approach for epilepsy patients. Different forms may have differing causes, seizure patterns and response to medications; so healthcare providers need to know exactly which antiepileptic drugs (AEDs) will best meet each individual patient’s needs in order to maximize seizure control and increase seizure prevention.
Effective Seizure Control: Tailoring treatment plans around an accurate diagnosis significantly increases the chance of optimal seizure control. Healthcare providers who understand epilepsy types can select medications or combinations of medicines which reduce seizure frequency and severity – ultimately improving quality of life and well-being for individuals.
Minimized Side Effects: Different AEDs may have differing side effect profiles. By tailoring treatment plans specifically to an epilepsy diagnosis, healthcare providers can choose AEDs which are less likely to cause adverse reactions for each individual – thus minimizing unnecessary side effects while improving medication tolerability and treatment adherence.
Targeted Interventions: Epilepsy can require interventions beyond medication alone. Accurate diagnosis helps identify individuals who could benefit from additional therapies like surgical resection, neurostimulation devices or alternative therapies like ketogenic diet. Tailoring treatments plans based on each diagnosis ensures individuals receive appropriate and effective interventions to effectively manage seizure outbreaks.
Prognostic Guidance: Accurate diagnosis is vitally important when predicting outcomes of epilepsy, providing valuable prognostic data. While certain forms have more favorable long-term prognoses with greater chances of outgrowing seizures or entering long-term remission.
Conversely, other forms may have unpredictable courses or be associated with increased risks; accurate diagnosis helps healthcare providers provide more informed prognostic advice so individuals and their families can better comprehend future prospects and make informed decisions regarding treatment, lifestyle modifications and future planning.
Customized Patient Education and Support: Tailored treatment plans that incorporate accurate diagnosis allow healthcare providers to offer tailored patient education and support, including tailored trigger identification.
Informed by accurate diagnoses, healthcare providers can then explain specific characteristics, triggers, and management strategies relevant to a diagnosed epilepsy type so as to empower people with epilepsy to be active participants in their own care by making informed decisions about it.