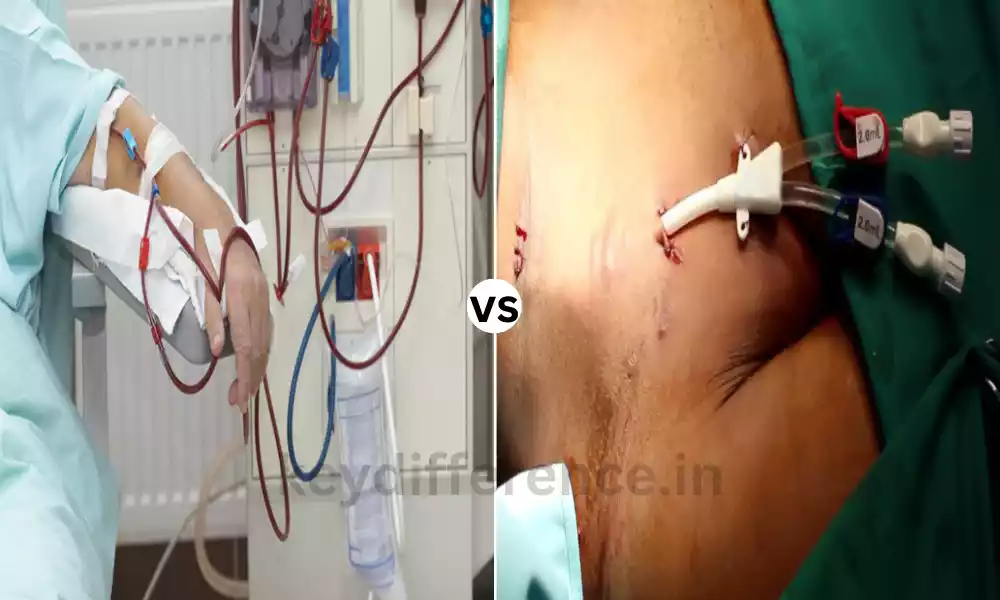
“Renal function plays a vital role in maintaining the body’s equilibrium. When kidneys falter, dialysis becomes a crucial intervention. Among the various dialysis methods, hemodialysis stands as a prominent approach.
Understanding the nuances between Dialysis and Hemodialysis sheds light on their differential impact, efficacy, and patient experiences.”
What is Dialysis?
Dialysis is a procedure that is used to simulate the functions of kidneys in the event that they are not able to effectively remove waste products and excess fluids from the blood.
It requires making use of either a device or a special solution that can eliminate toxins, regulate electrolytes, and ensure the proper balance of fluids in people who suffer from impaired kidney function.
This helps to restore the body’s balance of chemicals and eliminates waste products that normally are eliminated via urine.

What is Hemodialysis?
Hemodialysis is a particular type of dialysis that makes use of a dialyzer machine to remove blood from the body. In hemodialysis, the patient’s blood flows through the dialyzer. It functions as a kidney replacement and removes waste products, fluids, and toxins out of the blood.
The cleansed blood is transferred back to your body. This helps to maintain the proper electrolyte balance as well as eliminate the waste products, thereby compensating for the impaired kidney function.
Hemodialysis is usually performed at least once a week and takes place in a specialized medical facility that is specialized or at home with medical supervision.

Comparison Table of Dialysis and Hemodialysis
Certainly, here’s a comparison table highlighting the key differences between dialysis and hemodialysis:
| Aspect | Dialysis | Hemodialysis |
|---|---|---|
| Definition | A general term encompassing various kidney therapies | A specific type of dialysis using a machine and a dialyzer |
| Types | Includes various methods like hemodialysis and peritoneal dialysis | A subtype of dialysis involving a machine and blood filtration |
| Procedure Location | Can be performed at home or in a clinical setting | Primarily performed in specialized clinics or hospitals |
| Blood Filtration | Uses different methods (peritoneum or blood) to filter waste | Blood is filtered externally through a dialyzer |
| Frequency | Frequency varies based on the type of dialysis | Typically performed multiple times a week, 3-4 hours/session |
| Equipment Needed | May require specialized solutions, catheters, or peritoneal catheters | Requires a dialysis machine, dialyzer, and access point |
| Process Duration | Duration varies depending on the type of dialysis | Each hemodialysis session generally lasts 3-4 hours |
| Complications | Risks associated with specific methods (infections, catheter issues) | Potential complications related to vascular access, infection, or clotting |
| Patient Lifestyle | Impact on daily life varies based on the dialysis method | Requires adherence to scheduled treatment sessions, dietary restrictions, and fluid intake monitoring |
| Cost | Costs may vary depending on the method and setting | Costlier due to machine use, regular clinic visits, and specialized equipment |
| Effectiveness | Varies in terms of efficiency based on the method used | Efficient in quickly removing waste products from the blood and maintaining electrolyte balance |
This table provides a concise overview of the distinctions between dialysis as a broader term encompassing various methods and hemodialysis as a specific modality within dialysis involving blood filtration through a machine.
Dialysis Can Treat Kidney Failure
Dialysis may be used as a treatment option for kidney failure when kidneys cannot effectively remove waste or fluids produced in excess.
There can be numerous causes behind kidney failure; therefore dialysis could become necessary:
- Chronic Kidney Disease (CKD): When your kidneys suffer damage due to disease or damage from trauma, their function gradually deteriorates over time.
- Diabetes and high blood pressure: Both can result in kidney failure as a direct result, harming blood vessels that carry oxygen through your system and damaging kidney small arteries resulting in kidney failure.
- Glomerulonephritis: Glomerulonephritis is an Autoimmune Condition in which the Filtering system of your kidney, known as the Glomeruli, is Attacked by your Immune system Resulting in damage to these Filtration units and Eventual Kidney Failure.
- Polycystic Kidney Disease (PKD): Polycystic Kidney Disease is an Inherited disorder in which cysts of fluid form Within the kidneys, leading to Damage to these vital Organs and Eventually Leading to their Failure.
Dialysis may be necessary in cases of acute Kidney failure due to severe Infections, injuries, or drug Overdose. Dialysis often helps the kidneys recover after Experiencing acute Trauma and Illness. Dialysis may become necessary due to kidney failure caused by various factors; its use can be avoided or delayed through early diagnosis and management of these conditions.
Cause of Hemodialysis
The main reasons that lead to the necessity for hemodialysis are:
- Chronic Kidney Disease (CKD): Progressive and persistent impairment of the kidney with time because of conditions such as diabetes and hypertension (hypertension) glomerulonephritis or polycystic kidney diseases.
- Acute Kidney Injuries (AKI): Sudden and extreme reduction in kidney function owing to many causes like dehydration, infection injuries, injuries, or medicines.
- End-stage renal Disorder (ESRD): A phase of kidney disease in which the kidneys are losing nearly all their functions, and require the use of renal replacement therapies such as kidney transplants or hemodialysis to ensure the survival of the patient.
Hemodialysis doesn’t address the root of kidney disease but acts as a life-sustaining treatment by assisting the kidney in its functions in a controlled manner.
It assists in eliminating electrolytes, waste products, and fluid balance in patients whose kidneys do not do these things efficiently.
Advantages and disadvantages of dialysis
Dialysis can help treat kidney disease. Like any medical treatment, dialysis has its own set of advantages and drawbacks; some of which include:
Dialysis provides many advantages.
Here are just a few:
- Dialysis: Dialysis Can Improve Quality of Life Dialysis is used to clear away Waste fluids and waste products from your body, Which can Improve both Overall Health and Quality of life.
- Dialysis Can Prolong Life Expectancy: Dialysis provides vital lifesaving assistance for people living with kidney failure who would otherwise succumb to life-threatening kidney conditions without it.
- Dialysis: Dialysis treatments are readily accessible, being done in dialysis centers, hospitals, or even at home – making dialysis available to a wider number of those experiencing kidney failure.
Flexible Treatment Options: Dialysis offers various modes of administration. This may include hemodialysis (peritoneal), portable dialysis machines, or peritoneal dialysis. - Dialysis requires much time: Dialysis sessions often last several hours each and should be scheduled several times each week for best results. Dialysis also can cause nausea, low blood pressure, and muscle cramps that interfere with daily living activities and routines.
- Dialysis Patients Must Adhere to Diet Restrictions: Dialysis patients must strictly abide by diet restrictions that limit their consumption of salt, potassium, and phosphorus; however this can often prove challenging to accomplish. Dialysis treatments, particularly hemodialysis, may result in infections. This is especially true among those requiring dialysis treatments on an outpatient basis.
While dialysis may help manage kidney failure overall, individuals must consider all of its possible advantages and drawbacks and collaborate closely with medical providers in finding an individualized approach to treatment that suits each case.
Advantages and disadvantages of hemodialysis
Here are the pros and cons of the hemodialysis procedure:
Advantages of Hemodialysis:
- Affordable Waste Elimination: Hemodialysis is a highly efficient method of eliminating excessive fluids, waste products, and toxins from the bloodstream, assisting in maintaining the proper balance of electrolytes.
- Instant impact: It quickly addresses and manages symptoms of kidney failure. It offers quick relief from symptoms such as nausea, fatigue, and swelling.
- Structured treatment: The treatment schedule is structured and usually occurs frequently throughout the week which can offer regularity and stability for patients.
- Professional supervision: The procedure is carried out under the supervision of a medical professional in specially designed hospitals or clinics, providing rapid assistance in case of complications.
Disadvantages of Hemodialysis:
- Duration: Each session of hemodialysis may last between 3 and 4 hours and can be required several times per week, thereby altering the patient’s schedule as well as their daily routine.
- Vascular Access Problems: The requirement for secure access to vascular structures (such as grafts, fistulas, or catheters) could lead to complications such as bleeding, infection, or the shrinking of blood vessels over time.
- Dietary Restrictions: Patients who undergo hemodialysis typically are subject to strict dietary restrictions that include limits on fluid intake as well as potassium, phosphorus, and sodium. This may be difficult to follow.
- Potential Risks of Complications: The potential risks are low blood pressure and muscle cramps, infection at the entry point, anemia, and complications that are related to dialysis itself.
- Cost and Dependency: Hemodialysis is costly as it requires medical equipment, visits to clinics, and continuous medical monitoring. In addition, it can create a dependence on regular treatments.
Knowing the advantages and disadvantages is vital in assessing the effects of hemodialysis on the patient’s quality of life and overall health.
Summary
“Hemodialysis, a life-sustaining treatment for kidney failure, acts as a vital support system when the kidneys can no longer effectively filter waste and excess fluids from the blood.
This method, while efficacious in restoring electrolyte balance and removing toxins, presents both benefits and challenges in the lives of those dependent on this essential medical intervention.”