Dermatitis is a very common skin condition that can take on a variety of forms. Two of them are Atopic skin eczema (eczema) as well as seborrheic. While they share a few similarities however, knowing the main distinctions between the two types of dermatitis is essential for a precise diagnosis and effective treatment.
We will look at the differences between Atopic and Seborrheic Dermatitisas well as their causes, symptoms age groups affected, and treatment options.
Definition of Atopic Dermatitis
Atopic dermatitis, more commonly referred to as eczema, is a persistent and inflammatory skin condition that is characterized by red, itchy dry, and sometimes skin-like patches that are scaly or brittle skin.
It is regarded as one of the most common forms of dermatitis. It typically starts in childhood but may be present throughout adulthood. Atopic dermatitis is usually due to an inherited predisposition.
It is often triggered or exaggerated by a variety of environmental triggers, including allergies, irritants, or stress. The severity of the problem varies in some people, who experience periodic flare-ups and others experience more frequent and severe symptoms.
Effective treatment for Atopic dermatitis usually requires an array of treatments for the skin and moisturizers, lifestyle modifications as well as, in more severe instances, medications for the entire body or immunosuppressants.

Definition of Seborrheic Dermatitis
Seborrheic Dermatitis is a typical chronic skin condition that is characterized by itching, redness, and the appearance of white or yellow oily scales on the skin. It mostly affects regions of the body that have the highest concentration of oil glands like the face, scalp (especially around the eyes and nose) chest, and various skin folds. Seborrheic dermatology is frequently called “dandruff” when it affects the scalp.
The condition is thought to be related to an increase in the amount of naturally occurring yeast known as Malassezia that is found on the skin. Hormonal factors, neurological factors, and individual susceptibility could cause the condition.
Although seborrheic dermatitis is an ongoing problem its symptoms can usually be treated with medication-based shampoos, topical corticosteroids, and lotions for antifungal use good hygiene practices, and, in certain cases lifestyle changes. It is usually an ongoing issue with periods of remission or exacerbation.

The prevalence and impact of dermatitis on individuals
The impact and frequency of dermatitis on an individual can differ based on the particular kind of dermatitis and severity. We’ll present a review of the prevalence and effects of dermatitis
- Prevalence:
- Dermatitis is a very common skin condition that affects a large proportion of people worldwide.
- Different types of dermatitis are available including atopic dermatitis seborrheic and contact skin dermatitis, among others.
- The rates of prevalence may vary by location, age group, or genetic condition.
- It can affect people at any age, from babies to seniors.
- Impact on Individuals:
- Physical Discomfort: Dermatitis typically causes redness, itching discomfort, and pain which can seriously impact the quality of life for a person.
- Psychological impact: Skin conditions such as dermatitis can cause feelings of shame, self-consciousness, and low self-esteem because of obvious signs.
- Sleep disturbances: Itching and discomfort could interfere with sleep patterns and can lead to an increase in fatigue and lower general well-being.
- Deteriorated Functionality: In extreme cases, dermatitis may limit the ability of a person to carry out everyday activities and function effectively.
- Emotional and social effects Dermatitis can affect the social interaction and relationships of people because people are able to avoid social settings because of embarrassment or discomfort.
- Economic Impact: The costs that are associated with dermatitis may include dermatologist visits, over-the-counter remedies, and loss of productivity.
- Quality of Life:
- The effects of dermatitis can have a significant impact on a person’s well-being, impacting their emotional, physical, and social well-being.
- In severe or chronic cases, it can cause a decline in the capacity to participate in daily activities and live life to the highest degree.
- Achieving effective management and treatment for Dermatitis is essential to improve the living quality of those affected.
- Management and Coping:
- A lot of people with dermatitis get relief by identifying the cause and treatment. This could consist of topical creams, medicines lifestyle changes, as well as avoidance of the triggers.
- Strategies for managing stress, such as stress management strategies and assistance from medical professionals, friends, and relatives can help reduce the effects of dermatitis.
Dermatitis is an incredibly common skin condition that has an impact on a person’s physical as well as psychological well-being. An early diagnosis, timely treatment, and efficient methods of management are vital to minimizing its effects and enhancing the living quality of people affected by this skin condition.
The focus on differentiating between atopic and seborrheic dermatitis
It is crucial to distinguish between atopic (eczema) as well as seborrheic dermatitis is crucial to ensure a proper diagnosis and efficient treatment. Although both skin conditions are similar in some ways, however, they have distinct characteristics that can assist healthcare professionals in choosing the right procedure to follow.
This article will look at the main aspects that distinguish them:
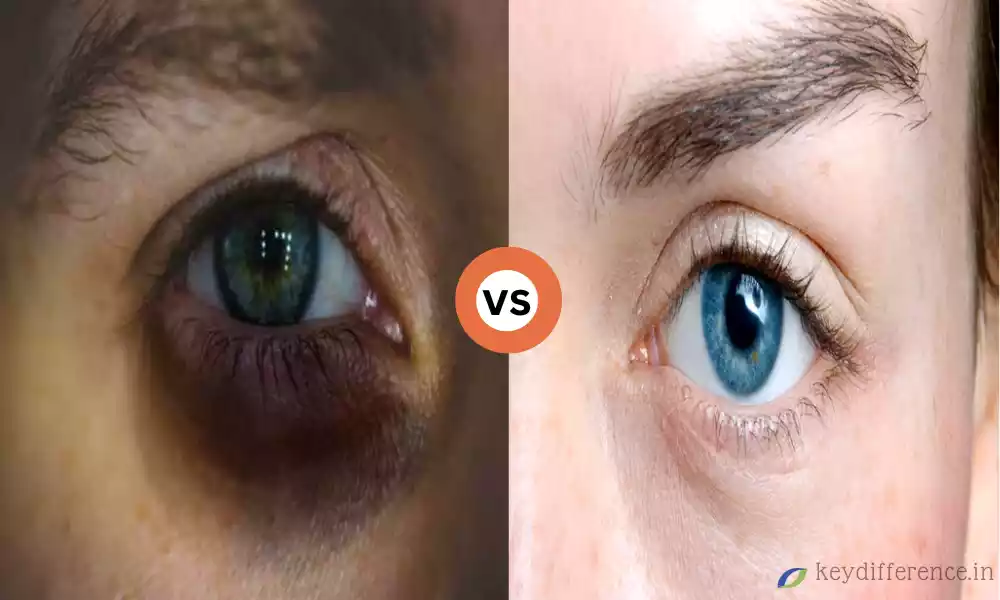
- Clinical Presentation:
- Atopic Dermatitis :
- Typically, it appears as dry, red, and itchy patches on the skin.
- Lesions can leak, ooze, or crust or turn an ecchymose.
- Most often, it affects the flexural regions (inside of knees, and in the back) but it may also affect other body parts.
- Seborrheic Dermatitis :
- It is distinguished by yellow, greasy, or white scales that are on an erythematous (red) foundation.
- Most often, it affects areas that have the most sebaceous (oil) glands including the face, scalp (nose eyebrows) chest, and skin folds.
- Atopic Dermatitis :
- Age of Onset:
- Atopic Dermatitis :
- Most cases begin in childhood, and some cases persist throughout adulthood.
- Seborrheic Dermatitis :
- Most often, it occurs in adulthood but it can be a problem for babies (cradle cap) as well as adolescents.
- Atopic Dermatitis :
- Affected Areas:
- Atopic Dermatitis :
- It can occur on different parts of the human body such as feet, hands, as well as the extremities.
- Seborrheic Dermatitis :
- It is most commonly found in areas with more sebaceous glands, like the face, scalp chest, face, and folds.
- Atopic Dermatitis :
- Scalp Involvement:
- Atopic Dermatitis :
- The presence of a scalp is possible, but not as common as in seborrheic dermatitis.
- Seborrheic Dermatitis :
- Sometimes, it is called “dandruff” when it affects the scalp. It can manifest as an itchy, flaking appearance.
- Atopic Dermatitis :
- Associated Symptoms:
- Atopic Dermatitis :
- The intense itching (pruritus) is a typical manifestation.
- Seborrheic Dermatitis :
- Itching (itching) can be common, but it may occur less frequently than the case of atopic allergic dermatitis.
- Atopic Dermatitis :
- Etiology:
- Atopic Dermatitis :
- Genetic predisposition plays an important impact on.
- Allergens and environmental factors can cause or intensify symptoms.
- Seborrheic Dermatitis :
- Sometimes, this is due to an overgrowth of yeast Malassezia that is often seen on the skin.
- Neurological and hormonal factors could be a contributing factor.
- Atopic Dermatitis :
- Treatment Approach:
- Atopic Dermatitis :
- The treatment typically consists of the use of moisturizers, topical corticosteroids, immunosuppressant drugs in extreme instances, and trigger avoidance.
- Seborrheic Dermatitis :
- Treatment typically includes medicated shampoos containing antifungal ingredients and corticosteroids for topical use (for extreme cases) and lifestyle adjustments.
- Atopic Dermatitis :
Although seborrheic and atopic skin dermatitis can share certain symptoms, such as itching and redness their clinical manifestations as well as the time of onset of affected areas, and the root cause of the problem differ.
A thorough exam by a doctor is essential for a precise diagnosis and the development of a suitable treatment plan to treat each condition.
Comparison Table of Atopic and Seborrheic Dermatitis
Here’s a comparison table highlighting the key differences between atopic dermatitis (eczema) and seborrheic dermatitis:
| Aspect | Atopic Dermatitis (Eczema) | Seborrheic Dermatitis |
|---|---|---|
| Clinical Presentation | Red, dry, itchy patches of skin; may ooze, crust, or scale | Greasy, yellow, or white scales on a red base; oily skin texture |
| Age of Onset | Often begins in childhood, can persist into adulthood | Usually occurs in adulthood; can affect infants (cradle cap) and adolescents |
| Affected Areas | Various body parts, including flexural areas (inside of elbows, behind knees) | Predominantly affects areas with more sebaceous (oil) glands, such as the scalp, face (nose, eyebrows), chest, and skin folds |
| Scalp Involvement | Less common but possible | Common; often referred to as “dandruff” |
| Itching (Pruritus) | Intense itching is a hallmark symptom | Pruritus is common but may not be as severe |
| Etiology | Genetic predisposition; triggered or exacerbated by environmental factors and allergens | Associated with an overgrowth of the yeast Malassezia; influenced by hormonal and neurological factors |
| Typical Name | Eczema | Dandruff (when affecting the scalp) |
| Treatment Approaches | Moisturizers, topical corticosteroids, immunosuppressant medications (severe cases), trigger avoidance | Medicated shampoos with antifungal agents, topical corticosteroids (severe cases), lifestyle modifications |
| Common in Infants | Yes (commonly known as infantile eczema) | Yes (cradle cap) |
| Severity | Can range from mild to severe | Generally milder but can vary in severity |
| Associated Conditions | Often associated with allergic conditions (e.g., asthma, hay fever) | Less frequently associated with allergic conditions |
| Body Areas Affected | Extremities, hands, feet, and other body parts | Primarily affects areas with more oil glands |
| Frequency of Occurrence | Common condition, affecting a significant portion of the population | Common condition, but less prevalent than atopic dermatitis |
| Treatment of Scalp Symptoms | Scalp-specific treatments may be needed | Often responds well to medicated shampoos |
Please note that individual cases may vary, and accurate diagnosis and treatment should be provided by a healthcare professional based on a thorough evaluation of the specific condition.
The focus on differentiating between atopic and seborrheic dermatitis
The distinction between atopic dermatitis (eczema), as well as seborrheic skin dermatitis, is vital for accurate diagnosis and efficient treatment. Although these two skin conditions are similar in some ways, however, they have distinct characteristics that can assist medical professionals in deciding on the best treatment plan. This article will concentrate on the most important factors that differentiate them:
- Clinical Presentation:
- Atopic Dermatitis :
- Typically, it appears as dry, red, and itchy patches on the skin.
- Lesions can ooze, become crusty, or even become scale-like.
- It most often affects the flexural areas (inside of the knees, and in the back) however it can also affect other body parts.
- Seborrheic Dermatitis :
- The characteristic of this species is yellow, greasy, or white scales that are on a red (red) foundation.
- Typically, the affected areas have Sebaceous (oil) glands like the face, scalp (nose eyebrows) chest, and folds of skin.
- Atopic Dermatitis :
- Age of Onset:
- Atopic Dermatitis :
- The majority of cases begin in childhood, but some instances persist throughout adulthood.
- Seborrheic Dermatitis :
- It usually occurs in adulthood, however, it can also be a problem for children (cradle cap) and teenagers.
- Atopic Dermatitis :
- Affected Areas:
- Atopic Dermatitis :
- It can occur on different parts of the body such as feet, hands, and even the extremities.
- Seborrheic Dermatitis :
- It is most commonly found in areas with more sebaceous glands, like the face, scalp chest, face, and folds.
- Atopic Dermatitis :
- Scalp Involvement:
- Atopic Dermatitis :
- It is possible to have a scalp, however, it is less frequent than seborrheic dermatitis.
- Seborrheic Dermatitis :
- Oft is described as “dandruff” when it affects the scalp, manifesting as itching and flaking.
- Atopic Dermatitis :
- Associated Symptoms:
- Atopic Dermatitis :
- The intense itching (pruritus) is a typical manifestation.
- Seborrheic Dermatitis :
- Itching (itching) is a common occurrence, but it isn’t as severe as it is in the case of atopic skin rashes.
- Atopic Dermatitis :
- Etiology:
- Atopic Dermatitis :
- Genetic predisposition plays an important part.
- Allergens and environmental triggers can cause or worsen symptoms.
- Seborrheic Dermatitis :
- Most often, it is associated with an overgrowth of the yeast Malassezia that is often seen on the skin.
- The hormonal and neurological influences may contribute.
- Atopic Dermatitis :
- Treatment Approach:
- Atopic Dermatitis :
- Treatment typically involves moisturizing agents as well as topical corticosteroids and immunosuppressant drugs in extreme cases, and trigger avoiding.
- Seborrheic Dermatitis :
- Treatment typically includes medicated shampoos that contain antifungal substances and corticosteroids applied to the skin (for the most severe cases) and lifestyle adjustments.
- Atopic Dermatitis :
Even though seborrheic and atopic skin dermatitis can share certain symptoms such as redness and itching their clinical manifestations and onset dates affected areas, and the underlying causes are different.
An attentive examination by a medical professional is essential for a precise diagnosis and for determining the best treatment plan to treat each condition.
Immunosuppressant medications in severe cases
In the case of Atopic skin eczema (eczema), the use of immunosuppressants can be considered as an option for severe cases that do not respond to conventional treatment options.
They work by reducing the immune system’s overactive reaction that can cause skin inflammation and symptoms caused by Atopic skin dermatitis.
Here are some essential details to consider regarding how immunosuppressants are used in the case of severe atopic dermatitis
- Indications: The use of immunosuppressants is typically reserved for those suffering from severe atopic dermatitis, who have not been able to respond effectively to other treatments, for example, topical corticosteroids moisturizers, and avoiding triggers. They aren’t typically utilized as an initial treatment.
- Types of Immunosuppressants:
- Topical calcineurin Inhibitors: They are applied directly on the affected skin and comprise medications like tacrolimus (Protopic) and pimecrolimus (Elidel).
- Systemic immune suppressants in more serious instances, injectable or oral drugs such as methotrexate, cyclosporine, azathioprine, dupilumab (a biologic) could be considered. These medicines have a wider effect on the body’s immune system and are generally recommended under strict medical supervision.
- Monitoring: If you are taking immune system suppressants, regular monitoring by a doctor is vital. Routine blood testing and checks will ensure that the medication is safe and safe and that any potential negative effects are detected in the early stages.
- The Side Effects: Immunosuppressant medicines may have adverse effects that can vary depending on the particular medication being used. These side effects could include a higher risk of getting sick as well as kidney and liver issues as well as high blood pressure and many more. The risk-to-benefit ratio must be carefully determined by the physician treating you.
- Time to Treat: The time frame of immunosuppressant treatment may differ from individual to individual and is contingent upon the seriousness of your disease and the response of each individual to treatment. The medications can be prescribed for a brief duration to treat the disease after which a long-term maintenance program with other treatments could be devised.
- Warning and monitoring of Children: Immunosuppressants, particularly systemic ones, should be recommended to be used with caution when children are involved because of their potential effects on development and growth. The decision to utilize these drugs in children is usually made after careful consideration of the potential risks and advantages.
- Multidisciplinary approach: Management of atopic dermatitis that is severe often requires a multidisciplinary approach which includes allergists, dermatologists, and immunologists, who tailor treatment plans according to each patient’s needs and address any of the underlying conditions that contribute to the condition.
It is essential for those suffering from severe atopic dermatitis, to work closely with their healthcare professional to establish the best treatment plan and also to track their condition for potential adverse effects or changes to the treatment plan.
Immunosuppressant medication is reserved for situations where the benefits are greater than the risks and when other treatments have proved ineffective in alleviating those symptoms associated with severe atopic allergic dermatitis.
Often referred to as “dandruff” when it affects the scalp
Seborrheic dermatitis is commonly known as “dandruff” when it affects the scalp. Dandruff is a frequent and prominent symptom of seborrheic skin dermatitis on the scalp. It is distinguished by the appearance of white, flaky hair or skin-colored scales that can be seen on dark-colored hair or clothing. The scales are caused by the excess shed of skin cells. They can be associated with redness and itching.
It is important to remember that dandruff can be a usual manifestation of seborrheic skin dermatitis in the scalp area, seborrheic skin dermatitis may also affect other parts of the body including your face (especially around the eyes and nose) and chest skin folds. In these locations, it can appear as greasy, red, and scaly patches more than flaky scales.
Treatment for scalp seborrheic Dermatitis typically involves the use of medicated shampoos with ingredients like ketoconazole and selenium sulfide or zinc pyrithione. These shampoos reduce the growth of Malassezia yeast on the scalp and ease symptoms. If you suffer from chronic or severe seborrheic dermatitis of the scalp the doctor might suggest alternative topical or oral treatments.
It’s crucial to distinguish between scalp seborrheic and other scalp issues such as psoriasis and tinea capitis (ringworm of the scalp) in that treatments for these conditions may differ.
If you suspect that you may have scalp dermatitis or dandruff it is recommended to speak with a dermatologist to get the correct diagnosis and advice regarding the most suitable treatments.
Medicated shampoos with antifungal agents
Shampoos with antifungal ingredients are commonly employed to treat conditions of the scalp that are caused or exacerbated by an overgrowth of fungal spores, like seborrheic dermatitis as well as certain kinds of dandruff.
They work by focusing and inhibiting the growth of the scalp fungus and can alleviate symptoms such as itching, redness, and flaking. Here are some commonly-used antifungal substances used in medicated shampoos
- Ketoconazole: Ketoconazole is an antifungal agent with a broad spectrum often employed in medicated shampoos to treat scalp problems. It is effective against yeast Malassezia which is commonly related to conditions such as seborrheic and Dandruff. Ketoconazole shampoos are sold on prescription or on the market.
- Selenium Sulfide: Selenium sulfide is another antifungal ingredient that is found in shampoos that contain medicated ingredients. It aids in limiting the development of Malassezia yeast and reduces symptoms of seborrheic dermatologic. Selenium sulfide shampoos are sold on the market and can be purchased by prescription.
- Pyrithione Zinc: Pyrithione Zinc is an antifungal and antibacterial ingredient that is often used in shampoos for dandruff. It assists in reducing the development of scalp yeast and reduces itching and flaking that are caused by the dandruff.
- COAL Tar: Coal Tar is a more traditional treatment option for a variety of scalp disorders like seborrheic dermatology. It aids in slowing the turnover of skin cells and decreases inflammation. Coal Tar shampoos can be purchased on the market.
If you are using medicated shampoos that contain antifungal agents:
- Follow the directions on the label of the product or as directed by your doctor.
- Typically, you’ll dampen your hair, then apply the shampoo on your scalp, then apply it to your scalp and massage it into. Let it sit for the time you’ve been advised to leave it on.
- Rinse thoroughly using water.
- The frequency of use can differ based on how severe your health condition is. Some shampoos are applied frequently and others are not used as often.
- Be careful not to get the shampoo into your eyes as certain formulas may cause irritation to your eyes.
- If you are experiencing any adverse reactions or if your symptoms become worse, you should consult an experienced healthcare professional.
It is important to remember that although these shampoos may be efficient in treating scalp issues they’re not the permanent solution. The ailments they treat tend to be long-lasting and require constant maintenance.
If you’re suffering from frequent or extreme scalp issues you should consult with an expert dermatologist to get a correct diagnosis and treatment strategy.
Presence of yellow or white scales
The appearance of white or yellow skin scales is a typical symptom of various skin conditions, such as seborrheic dermatitis psoriasis, and various kinds of fungal diseases. The appearance of these scales is a result of an abnormal shed from dead cells. They could differ in thickness and color in relation to the condition that is causing it.
This is a review of the appearance of white or yellow scales for various skin conditions:
- Seborrheic dermatology: Seborrheic dermatitis often manifests as greasy, yellow, or white scales that rest on the exudative (red) basis. These are usually seen on body parts with a large amount of oil glands, like the face, and scalp (especially around the eyes and nose) as well as the chest and folds of the skin. When they affect the scalp, it’s often called “dandruff.”
- Psoriasis: Psoriasis is a different skin condition that manifests as silvery or white scales that appear on inflamed, red skin. The scales tend to be larger and more prominent as compared to seborrheic dermatitis. Psoriasis can affect different areas of the body, including the elbows, scalp knees, nails, and knees.
- Fungal Infections: The fungal infection that affects the skin like tinea (ringworm) causes yellow or white scales to appear in those affected regions. It is possible to see the appearance as well as texture scales will vary based on the kind of fungus and area of the fungus.
- Ichthyosis: Ichthyosis is a type of genetic skin disorder that is characterized by scaly, dry skin. The ichthyosis scales can be thick and can be yellowish or have a whitish appearance. The condition can last for a long time and requires continual treatment.
- Xerosis (Dry skin): Extremely dry skin may cause the formation of yellowish or white scales. It is typically seen on areas that are susceptible to dryness, for instance, hands or legs, particularly during the colder months.
- Contact Dermatitis: Allergic or irritable contact dermatitis may cause the skin to dry out and become scaling, and the scales can appear yellow or white. This happens in response to contact with irritants or allergens.
It’s crucial to recognize the particular appearance of scales, as well as other symptoms and the position of the scales may aid healthcare professionals in identifying these different skin disorders.
A precise diagnosis is essential to determine the most appropriate treatment method, which could include medicated creams and Ointments, antifungal treatments the use of topical steroids and moisturizers or other treatments that are specifically designed to address the reason for the scaling.
If you’re concerned regarding the presence of scales in your body, it is recommended to see a dermatologist for an extensive examination and diagnosis.
Similarities Between Atopic and Seborrheic Dermatitis
Atopic dermatitis (eczema) and seborrheic are both skin conditions that are common although they do have distinct distinctions, they do have some commonalities. Here are a few key similarities between seborrheic and atopic dermatitis:
- Inflammatory skin conditions: Atopic seborrheic and atopic chronic skin conditions that cause inflammation, which means they are caused by an inflammation of the skin.
- The condition of pruritus (Itching): Itching (pruritus) is a common manifestation of both of the conditions. People with either disorder typically have severe itching, which can be extremely painful and depressing.
- Redness: It is a sign of inflammation. (erythema) can be a typical aspect of both atopic as well as seborrheic dermatitis. The skin affected may be red or itchy because of inflammation.
- Chronic as well as Recurrent: The two conditions are both thought to be recurrent and chronic in that they may last for a long time and can flare up frequently.
- Environmental triggers: These conditions are triggered or worsened through a variety of environmental triggers. For atopic dermatitis, typical triggers are allergens irritating substances, and seasonal changes. Seborrheic dermatitis can become more severe because of hormonal changes, stress, as well as exposure to certain skincare products.
- Effect on the Quality of Life: Both conditions have the potential to significantly affect the quality of life of a person. The redness, itching, and discomfort that accompany these conditions can result in stress, insomnia, and restrictions in everyday activities.
- Alternative Treatments: There is a bit of similarity in the treatment options for seborrheic and atopic dermatologists. Emollients and moisturizers are frequently suggested for both conditions to ease dryness and preserve the skin barrier. In some instances, topical corticosteroids can be employed to lessen inflammation.
- Individual Variation: The severity and duration of both conditions may differ greatly among people. Certain individuals may experience less severe symptoms that are more manageable to manage, whereas others might suffer from more severe and long-lasting varieties of ailments.
- Skin Care Guidelines: Good methods of skin care, including gentle cleansing, and staying clear of harsh soaps and irritants are crucial to control seborrheic and atopic dermatology.
Despite these similarities, it’s crucial to stress that atopic as well as seborrheic dermatitis are distinct in their symptoms with distinct causes, symptoms, and regions.
A proper diagnosis by a healthcare expert is vital to determine the difference between these two conditions and formulate specific treatment strategies. Treatment strategies can differ, particularly where triggers or other underlying issues need to be addressed.
Reference Books
Certainly, here are some reference books on various topics that you may find valuable. Please note that my knowledge is current up to September 2021, so there may be newer publications available since then:
General Reference:
- “The Oxford English Dictionary” – A comprehensive and authoritative dictionary of the English language.
- “The Encyclopedia of World History” by Peter N. Stearns – A comprehensive reference on world history.
- “The World Almanac and Book of Facts” – An annual publication containing a wealth of information on various topics, including statistics, events, and facts.
Science and Nature:
- “Cosmos” by Carl Sagan – A classic exploration of the universe and our place in it.
- “A Short History of Nearly Everything” by Bill Bryson – A popular science book that covers a wide range of topics in an accessible and engaging manner.
- “The Selfish Gene” by Richard Dawkins – A seminal work in evolutionary biology that explores the concept of the gene as a unit of selection.
History:
- “A People’s History of the United States” by Howard Zinn – A perspective on U.S. history from the viewpoint of marginalized groups.
- “Guns, Germs, and Steel” by Jared Diamond – An exploration of how geographic and environmental factors shaped human history.
- “The Rise and Fall of the Third Reich” by William L. Shirer – A detailed account of Nazi Germany and World War II.
Conclusion
Reference books are a great resource to acquire knowledge and details on a range of topics. If you’re looking to learn about the history of science, literature philosophy, or any other field, these reference books offer a wealth of information and information.
Remember that new books and editions are constantly being published so keeping up-to-date with the latest information will help you understand and increase your knowledge about your fields of interest.