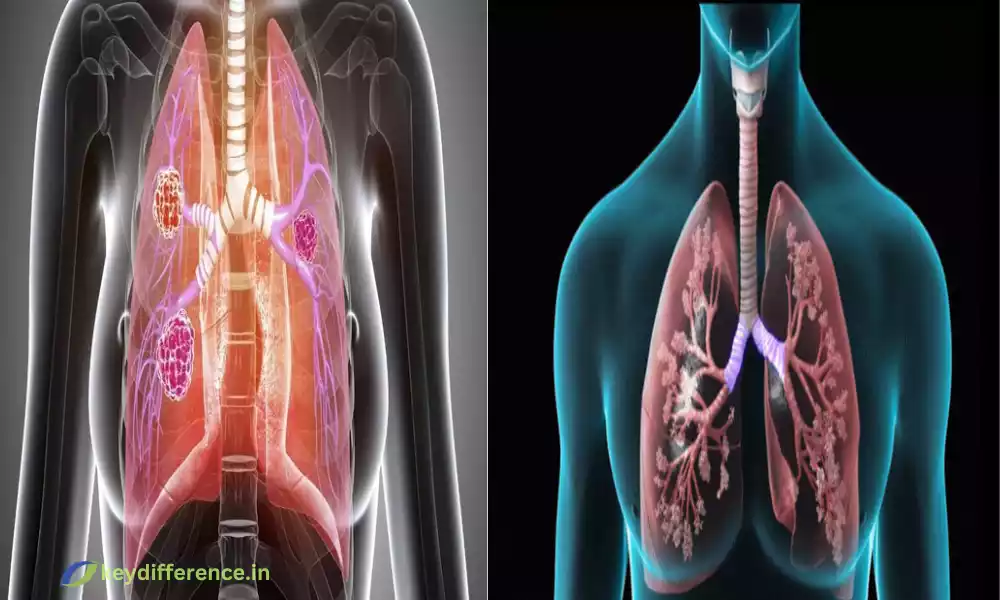
“Restrictive and obstructive pulmonary diseases are two distinct categories of respiratory disorders that affect the lungs and airways. While both can lead to breathing difficulties, they have different underlying causes, symptoms, and treatment approaches.
This brief overview will highlight the key differences between these conditions, providing insight into their significance in the field of pulmonary medicine.”
What is Restrictive Pulmonary Disease?
Restrictive pulmonary disease, commonly called the restrictive lung condition, is a category of respiratory disorders that are characterized by a diminished capacity of the lung to expand and fill up with air.
In these conditions the lung tissue gets damaged or stiff, making it difficult to absorb an adequate amount of air when inhaling. The decreased lung compliance or elasticity causes difficulties in reaching fully expanded lung capacity.
Important characteristics and traits of a pulmonary disease that is restrictive include:
- Reduced Lung Volume: People suffering from restrictive lung diseases suffer from a reduced lung capacity overall and therefore aren’t able to breathe in the same amount of air as healthy individuals when taking deep breaths.
- Lungs with difficulty expanding: The primary issue in restrictive lung ailments is the inability of the tissue of your lung to stretch properly. It can be caused by a variety of causes, such as swelling of the lung, scarring, or chest wall irregularities.
- The causes: There are several conditions that may cause restrictive lung conditions such as interstitial lung diseases (e.g. Idiopathic pulmonary fibrosis) chest wall disorders (e.g. scoliosis) as well as neuromuscular disorders (e.g. muscular dystrophy) and some occupational exposures.
- Pathophysiology: One of the most frequent reasons behind restrictive lung diseases is the fibrosis or scarring of the lung’s tissue. This affects the lung’s flexibility and compliance which makes it difficult to expand the lungs while inhaling.
- Clinical Signs: Individuals with restrictive lung disease usually experience dyspnea (shortness of breath) along with shallow and rapid breathing, as well as a reduced exercise tolerance. Chest discomfort and cough may also be in the air.
- Diagnose Methods: The diagnosis usually involves lung function tests like spirometry, which evaluates lung capacity and volume. Imaging tests like chest X-rays and CT scans could aid in identifying the root cause.
- Treatment and Management: The method of treating restrictive pulmonary disease is based on the causes. It can involve addressing the root cause and pulmonary rehabilitation to enhance lung function and in the case of severe instances oxygen therapy to assist in breathing.
It’s crucial to understand that early detection and proper treatment for restrictive pulmonary diseases are crucial in order to stop further lung damage and enhance the patient’s health. The treatment strategies are designed to ease symptoms, stop the progression of disease, and improve the performance of the lungs.

What is Obstructive Pulmonary Disease?
Obstructive pulmonary disease, commonly known as obstructive respiratory illness, can be described as a class of respiratory diseases that are characterized by closing or blockage of airways, making it difficult for patients to eliminate air out of their lungs upon exhalation.
The obstruction of airflow can lead to a variety of symptoms and may be chronic in nature.
The most important characteristics and characteristics of obstructive pulmonary diseases include:
- Airflow Limitation: The most prominent symptom of obstructive lung disease is the limitation of airflow, especially when exhaling. The reason for this is that the airways are narrowed by different factors, including the inflammation of muscles, constriction, or excessive mucus production.
- Greater resistance to airflow: In these conditions, there is a higher resistance to airflow through the bronchial tubes as well as the smaller airways (bronchioles). This may result in difficulties getting rid of air and lower airflow rates.
- causes: Obstructive pulmonary diseases include conditions such as Chronic Obstructive Pulmonary Disorder (COPD) as well as asthma and bronchiectasis. COPD is usually caused by long-term exposure to fumes from tobacco and asthma is characterized by chronic airway inflammation that can be caused by irritants or allergens.
- Pathophysiology: Obstructive lung diseases are inflammation and constriction of the bronchial tubes (narrowing in the airways) as well as excessive mucus production. All of these factors can cause restriction of airflow.
- Clinical manifestations: Common symptoms of obstructive lung disease are wheezing (a high-pitched whistling sound that occurs during breathing) and chronic cough. more breathing effort and breathing difficulty, particularly when you are active or at night.
- Diagnose Methods: Diagnostic methods typically involve lung function tests such as spirometry which assesses lung function as well as the rate of airflow. In some instances, tests for bronchodilator responsiveness can be done to test the possibility of reversing airflow limitation.
- The Management of and the Treatment: The treatment of obstructive lung conditions aims to ease symptoms, lessen inflammation of the airways, and increase the flow of air. Treatment usually includes bronchodilators to relax and expand your airways. Other treatments include anti-inflammatory medicines (corticosteroids) as well as changes in lifestyle such as quitting smoking. The management of asthma can also include the avoidance of triggers and the use of emergency inhalers when there is an exacerbation.
It’s crucial to understand that obstructive pulmonary conditions are often progressive and chronic which is why long-term care and monitoring is essential to reduce symptoms, avoid flare-ups, and keep the lung function. Early diagnosis and effective treatment can greatly enhance the health of those who suffer from obstructive lung diseases.

Comparison Table of Restrictive and Obstructive Pulmonary Disease
Here’s a comparison table outlining the key differences between restrictive and obstructive pulmonary diseases:
| Characteristic | Restrictive Pulmonary Disease | Obstructive Pulmonary Disease |
|---|---|---|
| Primary Feature | Reduced lung volume and capacity | Airflow limitation during exhalation |
| Underlying Causes | Interstitial lung diseases, chest wall abnormalities, neuromuscular disorders, occupational exposures | Chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis |
| Pathophysiology | Lung tissue scarring decreased lung compliance | Airway inflammation, bronchoconstriction, excess mucus production |
| Clinical Manifestations | Dyspnea, rapid and shallow breathing, reduced exercise tolerance, cough, chest discomfort | Wheezing, chronic cough, increased work of breathing, shortness of breath |
| Diagnostic Methods | Pulmonary function tests (spirometry, lung volume measurements), imaging (X-ray, CT scan) | Pulmonary function tests (spirometry, peak flow), bronchodilator responsiveness testing, imaging (X-ray, CT scan) |
| Treatment Approaches | Address underlying causes (e.g., pulmonary fibrosis), pulmonary rehabilitation, oxygen therapy | Bronchodilator medications (e.g., inhalers), anti-inflammatory drugs (e.g., corticosteroids), lifestyle changes (e.g., smoking cessation), avoiding triggers (e.g., allergens) |
| Long-term Management | Focus on preventing progression and improving lung function | Emphasis on symptom control, reducing exacerbations, and managing inflammation |
| Reversibility of Airflow Limitation | Generally not reversible | Partially or fully reversible in some cases, especially in asthma |
| Common Conditions | Idiopathic pulmonary fibrosis, scoliosis, muscular dystrophy | Chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis |
| Onset and Progression | Often gradual onset and progressive | Can vary in onset (e.g., acute exacerbations in asthma) and may have a progressive component (e.g., COPD) |
This table provides a concise overview of the main differences between restrictive and obstructive pulmonary diseases, including their primary characteristics, underlying causes, pathophysiology, clinical manifestations, diagnostic methods, treatment approaches, and more.
Understanding these distinctions is crucial for healthcare professionals in diagnosing and managing these conditions effectively.
Importance of understanding restrictive and obstructive pulmonary diseases
Understanding obstructive and restrictive pulmonary illnesses is vital for a number of reasons:
- Accurate Diagnosis: Differentiating between these two types of lung disease is crucial for health professionals to arrive at the correct diagnosis. Each category needs specific diagnostic tests and strategies to determine the causes and formulate a suitable treatment strategy.
- Tailored Treatment: Treatment options for obstructive and restrictive pulmonary conditions differ greatly. Knowing the class a patient is in makes sure that they receive the most effective and appropriate treatments that minimize side effects while optimizing the outcomes.
- The Prevention of Disease Progress: Early diagnosis and treatment can stop the progress of these diseases. When it comes to obstructive diseases such as COPD, timely intervention may reduce the decline in lung function. For chronic diseases, addressing the root of the issue can help prevent the development of lung tissue damage.
- Enhancing the quality of life for patients: Properly managed lung conditions can greatly improve the quality of life of a patient. Recognizing the unique difficulties and symptoms that come with obstructive and restrictive diseases permits healthcare professionals to address these issues in a way that helps patients breathe more easily and live more enjoyable lives.
- Patient Education: Patients who know the underlying causes of their illness are more likely to follow treatment protocols and adopt the lifestyle changes that are needed. Information about their condition enables patients to take a more active part in managing their health.
- Preventative Measures Knowing: the risks and the reasons for these illnesses can result in preventative actions. For instance, quitting smoking can aid in preventing COPD and the proper security measures at work can decrease the chance of being exposed to harmful substances for the lung.
- Innovative Research: A deep understanding of these diseases is essential for continuing research and the creation of new treatments and therapies. The advancement of knowledge could result in breakthroughs that will benefit both future and current patients.
- The Public Health Effect: Pulmonary diseases have an impact on public health in terms of healthcare expenses as well as the burden they place on people and society. Knowing more about these illnesses will allow you to allocate resources more effectively and decrease the impact of these diseases on overall the health of the public.
In the end, understanding the underlying causes of obstructive and restrictive lung illnesses is vital to ensure accurate diagnosis, individualized treatment, prevention of disease, and better outcomes for patients. Additionally, it plays a crucial role in helping to advance research in medicine and public health initiatives in relation to lung ailments.
Inflammation and narrowing of airways
The narrowing and inflammation of the airways are fundamental features of a variety of respiratory ailments including obstructive pulmonary conditions such as asthma, and chronic obstructive Pulmonary Disorder (COPD).
These factors significantly influence the pathophysiology and symptoms of these illnesses. This article will provide a more detailed review of inflammation and airway narrowing
Inflammation:
- definition: Inflammation is the body’s response to an injury, infection, or irritation. It triggers the immune system as well as the release of mediators of inflammation, including the chemokines, cytokines, and immune cells such as neutrophils and Eosinophils.
- In the Airways: In the context of respiratory diseases, inflammation occurs within the airways–specifically, the bronchi and bronchioles. The inflammation may be caused by a variety of factors, such as allergies (allergies like asthma) as well as irritations (such as smoking tobacco) respiratory infections as well and environmental pollutants.
- Role in Disease: Inflammation of the airways can cause negative consequences, including the narrowing of the airways, an increase in mucus production, as well as increased susceptibility to triggers. This can cause symptoms such as coughing, wheezing, and breath shortness.
- asthma: In asthma, chronic inflammation of the airways is a characteristic feature. This inflammation results in the closing of airways as a result of the constriction of smooth muscular cells within the bronchial walls. The swelling also affects the airway liner (mucosa) as well as increases the production of mucus which further blocks airflow.
- Therapy: The management of diseases characterized by inflammation of the airways usually involves anti-inflammatory drugs such as corticosteroids to decrease inflammation and avoid aggravations. These medications help ease symptoms and enhance lung function.
Narrowing of the Airways:
- Defined: Narrowing of the airways is a decrease in the diameter of lung bronchioles and bronchioles, which are the tiny air passages within the lung. This can be because of a variety of factors such as the constriction of muscles, inflammation, and mucus accumulation.
- The consequences: The blocked airways cause an increase in resistance to breathing. In the end, people might have difficulty exhaling air when exhaling, which is typical of obstructive pulmonary illnesses.
- Mechanisms: In asthma, airway narrowing is primarily because of the contraction of the smooth muscles that surround the airways. In COPD it may result from inflammation as well as the degeneration of the lung (emphysema) which decreases the structural strength of the airways.
- The symptoms are: Narrowed airways lead to typical symptoms such as wheezing (a high-pitched whistling sound when breathing) as well as increased breathing, and shortness of breath, particularly in the course of physical exercise or when there are aggravations of the condition.
- Therapy: Management of conditions that cause airway narrowing typically involves the use of bronchodilators, which include beta-agonists as well as anticholinergics. These medications reduce the tension of smooth muscle surrounding the airways, opening them up and enhancing the flow of air.
Understanding the interaction between inflammation and narrowing of the airways is vital in the diagnosis and treatment of obstructive pulmonary conditions. The ability to target these mechanisms using appropriate treatment and medications is crucial in reducing symptoms and enhancing lung function in patients with ailments.
Clinical manifestations and symptoms
The signs and symptoms that are associated with lung diseases differ based on the condition being treated However, here are a few common respiratory symptoms and symptoms that are common when someone suffers from lung-related issues:
- Dyspnea (Shortness of breath): This is one of the hallmark symptoms of lung illnesses. Patients may experience the sensation that they’re unable to breathe and their severity may vary from mild to severe.
- Cough: An ongoing and frequently chronic cough is typical in a variety of lung disorders. The cough can cause dryness or mucus in nature.
- “Wheezing”: It is an extremely high-pitched whistling sound that occurs during breathing, usually when exhaling. It’s often linked to airway narrowing or constriction.
- Chest Pain or discomfort: Chest pain can be a sign of a condition such as Pleuritis (inflammation of the pleura) lung infections or heart-related problems. The cause and area of pain could be different.
- Rapid Breathing (Tachypnea): An increased rate of respiration is typically experienced by people with lung disorders in order to compensate for the decreased oxygen exchange.
- Cyanosis: Discoloration that is gray or bluish on your skin lips, or nails may result from a lack of oxygen levels in blood. This is a sign of serious illness and requires medical attention immediately.
- Chronic Cough and Sputum Production: Chronic bronchitis and bronchiectasis can cause a chronic cough, accompanied by thick mucus or Sputum.
- Greater Breathing Work: Patients with severe lung diseases may require extra muscles and efforts to breathe, which can lead to visible chest retractions or the use of additional muscles.
- reduced tolerance to exercise: Some people may be tired or breathless during exercise, which can limit their capacity to exercise.
- Chills and fever: Infections, such as bronchitis or pneumonia, can cause chills, fever, and general feelings of sickness.
- clubbing on the fingers: In certain chronic lung diseases, the fingers might become rounded and larger (clubbed) which could be an indication of oxygen deficiency.
- Productive cough with blood: Hemoptysis which is bleeding blood from the lungs can be a sign of various lung ailments, including lung cancer, lung infections, and pulmonary embolism.
- Weight Fatigue and Loss: Chronic lung disease can result in unintentional reduction in weight and tiredness as a result of an increased expenditure of energy during breathing, and decreased appetite.
- Noisy Breathing: Unusual sounds like crackles, rales, or rhonchi could be detected by health professionals during lung exams, which could indicate possible problems.
It’s crucial to recognize that the symptoms and signs differ widely based on the cause of respiratory disease. A precise diagnosis and proper treatment are crucial to addressing these symptoms and improving the quality of life for the patient. Early intervention is crucial in preventing any further complications and enhancing health and quality of life.
What are the Similarities Between Restrictive and Obstructive Pulmonary Disease?
Although obstructive and restrictive pulmonary illnesses have distinct features they share some features between them too in the main, which is due to their impact on overall health. Here are a few of the key similarities:
- Respiratory Signs and symptoms: Both restrictive and obstruction-related pulmonary conditions can trigger common respiratory symptoms, such as coughing breathlessness (dyspnea), and chest discomfort, although due to various reasons. These symptoms usually prompt patients to seek medical treatment.
- reduced exercise tolerance: Patients suffering from the two kinds of pulmonary disorders might experience restrictions in their ability to take part in physical activities. Reduced exercise tolerance is a common symptom of diminished lung function.
- Image Abnormalities: Image studies like chest X-rays and CT scans may reveal irregularities that affect the lung structures of patients who suffer from both obstructive and restrictive lung illnesses. They could include inflammation, scarring, or changes in tissues of the lung.
- Tests for Pulmonary Function: Both conditions typically have abnormal results from lung tests of function (PFTs). However, the precise patterns of abnormalities vary. In restrictive conditions, the result is a decline in lung capacity and volume when compared to obstructive disorders airflow limitations are a major symptom.
- Long- and Short-Term impact: Both types of lung diseases can have substantial impact on the short- and long-term quality of life for an individual. Controlling symptoms and preventing progression are crucial in both instances.
- Risk Factors: Certain risk factors associated with lung diseases, like smoking cigarettes and exposure to pollutants from the environment, are common to both obstructive and restrictive conditions. Eliminating these risk factors is vital to preventing them.
- Multidisciplinary Treatment: Both types of lung diseases can need a multidisciplinary approach for care that involves pulmonologists physical therapists, respiratory therapists, and other health specialists to tackle different aspects of the illness and enhance the quality of life for patients.
Even though these similarities are present it’s important to realize that obstructive and restrictive pulmonary conditions are distinct in relation to their underlying cause, pathophysiology, diagnosis criteria, and methods of treatment.
A precise diagnosis and distinction between them is essential to provide appropriate treatment and enhance the patient’s outcomes.
Reference Books
Certainly! Here are some reference books related to pulmonary diseases and respiratory medicine that can provide in-depth information on the topic:
- “Murray and Nadel’s Textbook of Respiratory Medicine” by V.C. Broaddus, J.F. Murray, and J.A. Nadel
- This comprehensive textbook covers all aspects of respiratory medicine, including both restrictive and obstructive pulmonary diseases.
- “Interstitial Lung Disease” by Talmadge E. King Jr. and Joel D. Ernst
- Focuses on interstitial lung diseases, a significant subset of restrictive pulmonary diseases, offering insights into their diagnosis and management.
- “Chronic Obstructive Pulmonary Disease” by Bartolome R. Celli and John E. Heffner
- A specialized book that delves into COPD, one of the most common obstructive pulmonary diseases, with an emphasis on its clinical aspects.
- “Asthma: Epidemiology, Anti-Inflammatory Therapy, and Future Trends” by Mario Cazzola and Stephen T. Holgate
- Provides a comprehensive overview of asthma, a prevalent obstructive pulmonary disease, discussing its epidemiology, treatment, and emerging trends.
- “Pulmonary Physiology” by Michael G. Levitzky
- A foundational book that explains the principles of pulmonary physiology, offering a solid understanding of how the respiratory system works.
Conclusion
Knowing the distinction between obstructive and restrictive conditions is crucial for health doctors or patients as well as anyone who is interested in the health of their respiratory system. Each of these conditions has distinct characteristics such as their causes, symptoms, treatments, and diagnostic methods.
A proper diagnosis and treatment can significantly enhance the living quality of those affected by these illnesses, highlighting the importance of early detection and proper treatment.