Introduction
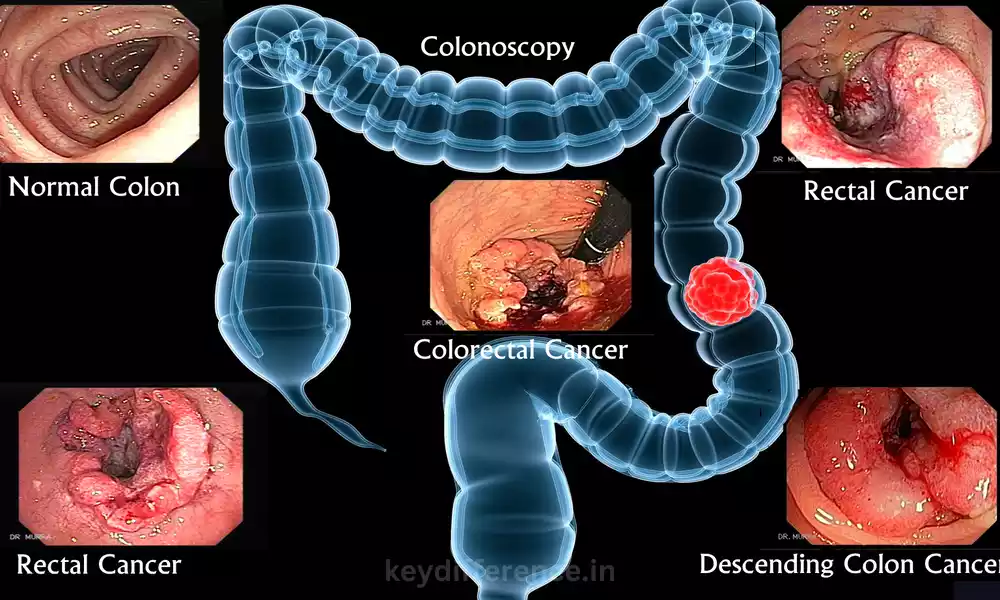
Colon and rectal cancers are two forms of digestive malignancies, each affecting different areas within the large intestine. While they share similarities in terms of their causes and treatments, their locations vary, making understanding the differences between colon and rectal cancer essential for accurate diagnosis, effective treatment planning and improved patient outcomes.
This content outline explores the Differences between colon and rectal cancer in terms of Anatomy, location, risk factors, symptoms, diagnosis, Treatment options, prognosis and Prevention strategies.
By Understanding these differences better, healthcare Professionals and Individuals alike can gain more Knowledge and make informed decisions regarding Prevention, early detection, management and prognosis of these conditions.
Definition of colon cancer
Colon Cancer (also referred to as colorectal cancer) is a Malignant tumor found in the colon of the Large Intestine. Typically, colon Cancer arises from Polyps that form on its inner lining; Eventually these polyps can turn cancerous and spread throughout surrounding tissue causing severe complications that significantly decrease survival rates if left untreated. Early detection and prompt treatment are key for improving outcomes in colon cancer cases.
Definition of rectal cancer
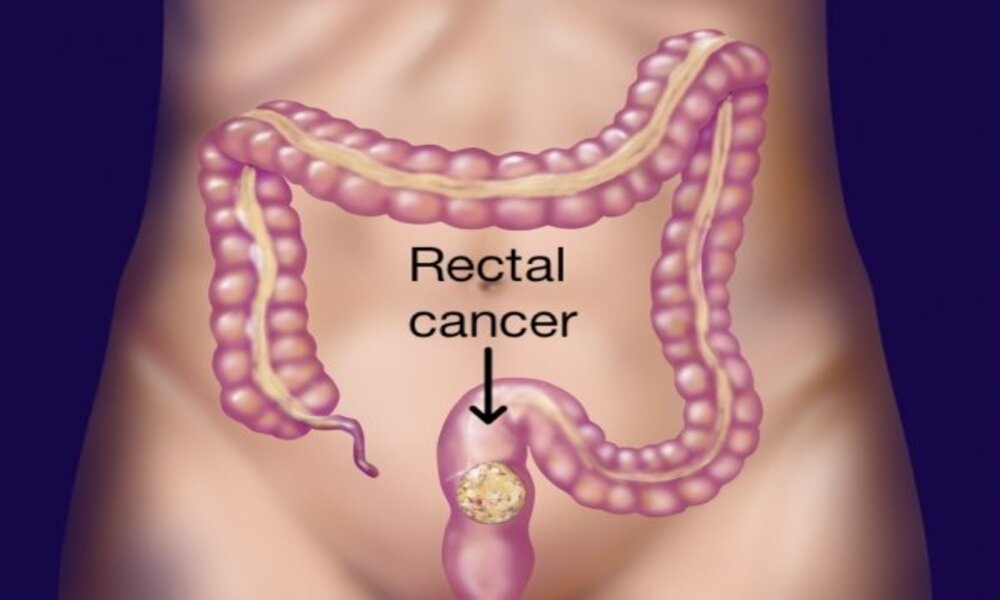
Rectal cancer refers to Malignant tumors found in the rectum, the last Segment of large intestine Located just above the anus. Like colon cancer, rectal cancer typically begins as Precancerous polyps that form on its inner lining Before Progressing into Cancerous cells that invade Nearby tissues and spread.
If not detected and treated early enough, rectal cancer can spread to nearby lymph nodes and organs leading to advanced stages. Thus early diagnosis and appropriate therapy are key elements for improved outcomes in rectal cancer cases as is colon cancer cases.
Difference Between Colon and Rectal Cancer
Sure! Here’s a comparison table highlighting the key differences between colon and rectal cancer:
| Aspect | Colon Cancer | Rectal Cancer |
|---|---|---|
| Location | Begins in the colon, the large intestine’s first segment after the small intestine | Begins in the rectum, the last section of the large intestine just above the anus |
| Risk Factors | Similar risk factors as rectal cancer, including age, family history, inflammatory bowel disease, and lifestyle factors | Similar risk factors as colon cancer, including age, family history, inflammatory bowel disease,and lifestyle factors |
| Symptoms | Abdominal pain or discomfort, changes in bowel habits, rectal bleeding, fatigue, unexplained weight loss, anemia | Changes in bowel habits, rectal bleeding,persistent urge to have a bowel movement,abdominal pain or discomfort |
| Diagnostic Tests | Colonoscopy, flexible sigmoidoscopy, stool tests,imaging tests (CT scan, MRI, etc.) | Colonoscopy, flexible sigmoidoscopy, digital rectal exam, imaging tests (CT scan, MRI, etc.) |
| Treatment Options | Surgery (colectomy), chemotherapy, radiation therapy, targeted therapy |
Surgery (low anterior resection, abdominoperineal resection), chemotherapy, radiation therapy, |
| Prognosis | Prognosis varies based on stage and other factors | Prognosis varies based on stage and other factors |
| Prevention | Healthy lifestyle, regular screening (colonoscopy),polyp removal, aspirin use (in certain cases) | Healthy lifestyle, regular screening (colonoscopy), polyp removal, aspirin use (in certain cases) |
Please note that this is a simplified overview, and each case of colon or rectal cancer may vary in terms of its specific characteristics and treatment approach.
It’s important to consult with a healthcare professional for a comprehensive evaluation and personalized care.
Importance of understanding the differences between the Colon and Rectal Cancer
Understanding the differences between colon and rectal cancer is of great significance for several reasons, such as:
Accurate Diagnosis: Healthcare professionals benefit greatly from knowing the differences between colon and rectal cancer to accurately diagnose and stage it. Tumor location has an effect on diagnostic tests and imaging techniques used, providing targeted evaluations to confirm which form of cancer exists.
Treatment Planning: Colon and rectal cancer may require different approaches due to variations in their locations and anatomical structures, enabling healthcare providers to create personalized plans tailored specifically for each type of cancer, ultimately leading to improved results and patient care.
Prognosis and Survival Rates: Colon and rectal cancer have different prognoses and survival rates. Recognizing these disparities allows patients and their loved ones to develop a realistic understanding of potential outcomes, make informed choices regarding treatment options available, and prepare themselves for potential obstacles associated with each form of cancer.
Prevention and Screening: Being informed on the differences between colon and rectal cancer helps individuals form targeted prevention strategies and screening recommendations. By understanding each type’s individual risk factors, individuals can make necessary lifestyle modifications, undergo recommended screening tests, and take precautionary steps against developing either cancer type.
Patient Education and Support: Being informed about the differences between colon and rectal cancer helps patients better comprehend their diagnosis and actively take part in their care journey. Healthcare providers can then tailor education, resources and support specifically tailored to that patient’s diagnosis – leading to informed decision-making and emotional well-being for all concerned parties.
Understanding the differences between colon and rectal cancer helps improve diagnostic accuracy, enable personalized treatment planning, provide realistic expectations about prognosis and prophylaxis, support prevention efforts and empower patients to actively participate in their healthcare journey.
Similarities in location between colon and rectal cancer
Colon and rectal cancer share similar geographic origins within the large intestine. Both forms of cancer manifest themselves within the digestive tract, specifically impacting colon and rectal tissues.
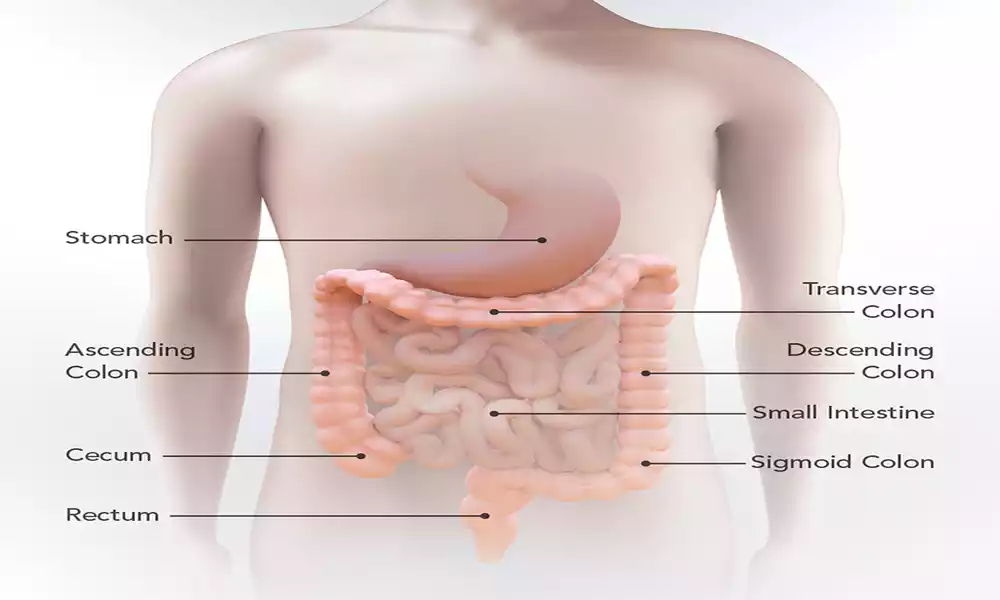
The colon is a long, hollow tube that makes up most of the large intestine. It starts at the cecum (first portion of large intestine) and extends all the way to the rectum; with its final segment just above anus being known as the rectum.
Colon cancer affects not only the colon itself, but all four sections – ascending, transverse, descending and sigmoid. Rectal cancer typically originates in the rectum but may spread into lower parts of sigmoid colon.
Due to their proximity, colon and rectal cancer share similarities in terms of organs and structures affected. There may also be distinct variations regarding where within the large intestine they are found, which may influence diagnostic approaches, treatment options and potential complications.
Common risk factors for both colon and rectal cancer
Both colon and rectal Cancer share some shared risk Factors, such as:
Age: The risk of colon and rectal cancer Increases with age, with most cases being seen among Individuals aged 50 years or over; however, they may also occur among younger Individuals.
Family History and Genetics: Colon or rectal cancer runs in families, especially first-degree relatives (parents, siblings and children), which increases your risk. Certain hereditary conditions such as Lynch syndrome and Familial Adenomatous Polyposis (FAP) further increase this risk.
Personal History of Polyps or Inflammatory Bowel Disease (IBD): Individuals who have had precancerous polyps (adenomas) in either the colon or rectal regions have an increased risk of cancer development, as do individuals suffering from ulcerative colitis and Crohn’s disease which also increase this risk.
Lifestyle Factors: Unhealthy lifestyle choices increase the risk of colon and rectal cancer, such as eating too many red and processed meats, low fiber intake, sedentary living styles, obesity, smoking excessive alcohol consumption or a lack of physical activity.
Race and Ethnicity: African Americans and Ashkenazi Jews tend to have higher incidence of colon and rectal cancer compared to other populations.
Diabetes: People living with type 2 diabetes face an increased risk of colon and rectal cancer.
Previous History of Cancer: Individuals who have Previously Experienced colon, rectal, or other Cancers may be at an Increased risk for developing Secondary primary colon or Rectal cancers.
Note that these risk factors increase the likelihood of colon and rectal cancer, they do not guarantee it. Even individuals without these risk factors can still develop colon or rectal cancer; regular screenings, early detection, and leading a healthy lifestyle can all help lower this risk and improve outcomes.
Additional risk factors specific to colon cancer
As well as sharing Common risk factors with rectal cancer, colon cancer poses its own Unique set of risk factors that must be taken into Consideration. These include:
Polyp Characteristics: Certain polyps in the colon, such as large or multiple adenomatous polyps, increase your risk for colon cancer. Adenomas are precancerous growths with potential to become cancerous over time.
Inherited Colon Cancer Syndromes: Rare genetic Conditions like hereditary Nonpolyposis colorectal cancer (HNPCC), more Commonly referred to as Lynch syndrome, and familial Adenomatous polyposis (FAP), significantly raise your risk for colon cancer. These syndromes are marked by gene mutations that predispose individuals towards multiple polyps and/or colorectal cancer development in individuals who carry them.
Personal History of Colon Cancer or Precancerous Polyps: Individuals who have had colon cancer in the past or certain Precancerous polyps are at an Increased risk for colon cancer Recurrence in future years.
Inflammatory Bowel Disease (IBD): IBD increases your risk for both colon and Rectal cancer; however, its risk is highest with colon cancer. Individuals living with Longstanding ulcerative colitis or Crohn’s Disease affecting the colon have an Increased chance of Becoming colon cancer Patients.
Radiation Therapy: People who have received radiation therapy to treat abdominal or pelvic cancers in the past may be at an increased risk of colon cancer later on.
Certain Inherited Gene Mutations: Beyond hereditary cancer syndromes, other genetic mutations like those found in the MUTYH gene can increase risk for colon cancer development.
Importantly, additional risk factors do not guarantee colon cancer development and individuals without these risk factors may still develop it. Screening, early detection and lifestyle modifications are key ways of lowering risks and improving outcomes related to colon cancer.
Additional risk factors specific to rectal cancer
Additionally, rectal Cancer has its own set of risk Factors which differ from those shared with colon Cancer, including:
Location: Due to its close Anatomical relationship and unique Position within the pelvis, rectal cancer risk Factors include the Proximity between its rectum and anus and its Unique position within it. Furthermore, rectal cancer located lower on its site could affect its management and treatment options.
Sex: Men have a Slightly increased risk of rectal cancer Compared to women, Although the Difference in risk isn’t as Noticeable.
Rectal Polyps: Certain kinds of rectal polyps, known as adenomatous polyps, can significantly increase your risk for rectal cancer. Adenomas are precancerous growths with potential to turn cancerous over time.
Inflammatory Bowel Disease (IBD): While IBD increases your risk for both colon and Rectal cancers, its effect on Rectal cancer risk is Particularly pronounced. Individuals Suffering from long-Standing ulcerative colitis Affecting the rectum have an Increased chance of rectal cancer Developing over time.
Previous Anal Cancer History: Individuals who have had anal cancer, which shares Similar risk factors and location to rectal cancer, may have an Increased chance of rectal cancer Developing.
Human Papillomavirus (HPV) Infection: Certain strains of HPV, Specifically types 16 and 18, have been Associated with Increased risk of anal cancer; there may also be some Overlap in HPV-related risk factors Between anal and rectal cancers.
Radiation Therapy: Individuals who have had radiation therapy for prior cancers in their pelvis area may be at a higher risk for rectal cancer.
Note that these risk factors do not guarantee rectal cancer; individuals without these additional factors can still develop it. Screenings, early detection and lifestyle modifications are critical components in lowering risks and improving outcomes associated with rectal cancer.
Symptoms more commonly associated with colon cancer
Though symptoms of colon and rectal cancers may overlap, there are certain indicators more often associated with colon cancer.
These may include:
Changes in Bowel Habits: Colon cancer symptoms that manifest themselves with persistent changes to one’s bowel habits include changes to frequency, consistency and caliber of bowel movements; such as diarrhea, constipation or more narrow stool than usual.
Blood in Stool: Blood can be an indicator of colon cancer. Blood may appear either visibly in the stool or cause it to appear dark and tarry in appearance.
Persistent Abdominal Discomfort: Constant abdominal discomfort such as cramps, pain or an increased feeling of fullness may be an early indicator of colon cancer. This discomfort could be localized in one part or more generalized throughout your lower abdomen area.
Unintentional Weight Loss: Unexpected and unexplained weight loss without clear cause such as diet or physical activity changes could be a symptom of colon cancer. Such weight loss could coincide with loss of appetite.
Fatigue and Weakness: Colon cancer may result in fatigue and weakness that could be related to anemia or your body’s response to cancer itself.
Iron Deficiency Anemia: Colon cancer’s ongoing or recurrent bleeding can result in iron deficiency anemia, marked by low red blood cell count and reduced iron levels, with symptoms including fatigue, weakness and shortness of breath.
Important to remember is that these symptoms could also be indicative of other conditions and do not necessarily indicate colon cancer.
However, if any persist or are accompanied by other suspicious signs it’s essential to consult a healthcare professional and undergo appropriate testing immediately – early detection and timely treatment have proven to dramatically improve outcomes in colon cancer cases.
Symptoms more commonly associated with rectal cancer
Though symptoms of colon and rectal cancer may overlap, rectal cancer symptoms tend to be more prominent. They include:
Changes in Bowel Habits: Rectal cancer has long been linked with persistent changes to one’s bowel habits, including increases or decreases in frequency, consistency or caliber of bowel movements – such as diarrhea, constipation or feeling of incomplete emptying after each visit to the restroom.
Rectal Bleeding: One of the hallmark symptoms of rectal cancer is rectal bleeding. This may manifest itself in bright red blood in your stool, on toilet paper, or after having a bowel movement; occasionally blood may mix with your stool to darken its color or make it appear.
Persistent Urgency to Have a Bowel Movement: Feeling an urgent urge to urinate often after recently emptying the bowels is one of many symptoms associated with rectal cancer, though its origin may not necessarily be tied to changes in diet or hydration status.
Abdominal Discomfort and Pain: Individuals diagnosed with rectal cancer may experience chronic abdominal discomfort or pain, typically concentrated in their lower abdomen or around their rectum area. The discomfort could range from cramp-like sensations to an ongoing dull ache.
Sensation of Incomplete Emptying: Rectal cancer may cause you to feel that the rectum has not been completely emptied after each bowel movement, which may cause discomfort and strain during subsequent movements. This symptom could contribute to strain or difficulty with passing stool altogether.
Narrowing of Stools: Rectal cancer may result in narrowing or thinning of the stools, often described as pencil-thin stools. This narrowing occurs due to obstruction caused by tumors which hinder stool passage through your system.
Notably, these symptoms may also be related to other conditions, including hemorrhoids or inflammatory bowel disease. But if any of them persist or appear along with other worrying symptoms, it’s a good idea to consult a healthcare professional for further assessment and testing – early detection can significantly increase chances of successful rectal cancer cases.
Screening tests for colon and rectal cancer
Screening tests are essential in early detection and prevention of both colon and rectal cancer. Here are some commonly utilized screening tests for colon and rectal cancer:
Colonoscopy: Colonoscopy is widely considered the gold standard screening test for both colon and rectal cancer. A flexible tube (colonoscope) equipped with a camera is inserted into the rectum and advanced through the colon, enabling doctors to observe both areas and identify any abnormalities before potentially extracting precancerous polyps or performing biopsies if necessary.
Fecal Occult Blood Test (FOBT): FOBT is a noninvasive stool screening test to detect hidden blood in stool samples collected at home and submitted for laboratory analysis. FOBT can detect even minute amounts of blood that might otherwise not be visible, which could indicate colon or rectal cancer as well as other digestive conditions.
Fecal Immunochemical Test (FIT): Fecal Immunochemical Tests are stool-based tests used to detect blood in stool. Like FOBT, however, they use antibodies specific for human blood that reduce false-positive results due to diet. As a result, FIT offers more sensitive and specific testing compared to traditional FOBT.
Flexible Sigmoidoscopy: Flexible sigmoidoscopy involves inserting a flexible tube with a camera (sigmoidoscope) into the rectum and lower portion of the colon, providing visibility of these areas – commonly associated with rectal cancer. While not as comprehensive as colonoscopy, flexible sigmoidoscopy can still detect abnormalities within this part of the digestive tract.
Virtual Colonoscopy (CT Colonography): Virtual colonoscopy is a noninvasive imaging test using computed tomography (CT) scans to create detailed images of the colon and rectosigmoid area, including detection of polyps or tumors in three dimensions. If abnormalities are discovered, further evaluation or removal may be required via follow-up colonoscopy.
Stool DNA Test: Stool DNA testing with Cologuard detects genetic changes that could indicate colon or rectal cancer, in an easy and noninvasive process that is performed at home with collection of stool sample. Results will be analysed at laboratory.
Selecting the most appropriate screening test depends on various factors, including age, personal and family medical history and personal preferences. Consultation with healthcare providers will help identify the most suitable approach based on individual circumstances.
Diagnostic procedures for confirming the presence of cancer
When screening tests or symptoms indicate the possibility of colon or rectal cancer, additional diagnostic procedures may be conducted in order to confirm it. Here are some of the more Frequently utilized Diagnostic tools:
Colonoscopy: Colonoscopy serves both as a Screening test and direct Visualization of the colon and rectum, Providing direct access to its inner Workings. A thin flexible tube equipped with a camera (colonoscope) is inserted into the rectum before being advanced through to colon. During this procedure, doctors can visually examine colon lining for abnormalities as well as take biopsies or remove polyps for further investigation and testing.
Biopsy: To conduct a biopsy requires taking a tissue sample from an area identified during colonoscopy or imaging tests that is suspicious for cancer cells and sending it off for laboratory analysis by a pathologist; biopsy results provide definitive diagnoses of colon or rectal cancer.
Imaging Tests: Imaging tests may assist in assessing the extent and spread of cancer, including potential metastasis. Such exams could include:
Computed Tomography (CT) Scan: CT scans use X-rays and computer technology to generate detailed cross-sectional images of the colon, rectum and nearby structures that help assess tumor size and location as well as detect any spread to nearby lymph nodes or organs.
Magnetic Resonance Imaging (MRI): An MRI employs magnetic fields and radio waves to generate detailed images of the colon, rectum, and surrounding tissues. An MRI provides information regarding tumor size, extent, invasion into nearby structures, metastasis formation, as well as presence.
Positron Emission Tomography (PET) Scan: A PET scan involves injecting a radioactive tracer into your body. Cancerous cells tend to absorb more of it than usual, which can then be detected using special camera technology. This test helps determine whether cancer has spread to distant organs or lymph nodes.
Blood Tests: Blood tests may be conducted to assess certain markers associated with colon or rectal cancer, such as carcinoembryonic antigen (CEA). An elevated level of CEA could indicate either cancerous growth or monitor its response to treatment.
Diagnostic procedures provide crucial data to confirm the presence of colon or rectal cancer, evaluate its stage, and help guide treatment decisions. When making this decision it’s wise to consult a healthcare professional regarding what approach would best meet individual circumstances.
Conclusion
Understanding the differences between colon and rectal cancer is critical for accurate diagnosis, effective treatment planning, and improved patient outcomes. While both forms affect the large intestine, their specific locations often dictate diagnostic approaches and treatment approaches.
Recognizing both shared risk factors of colon and rectal cancer as well as any additional ones unique to each type allows for targeted prevention strategies and screening recommendations. Early detection through regular colonoscopies or stool-based tests can significantly improve prognosis and survival rates.