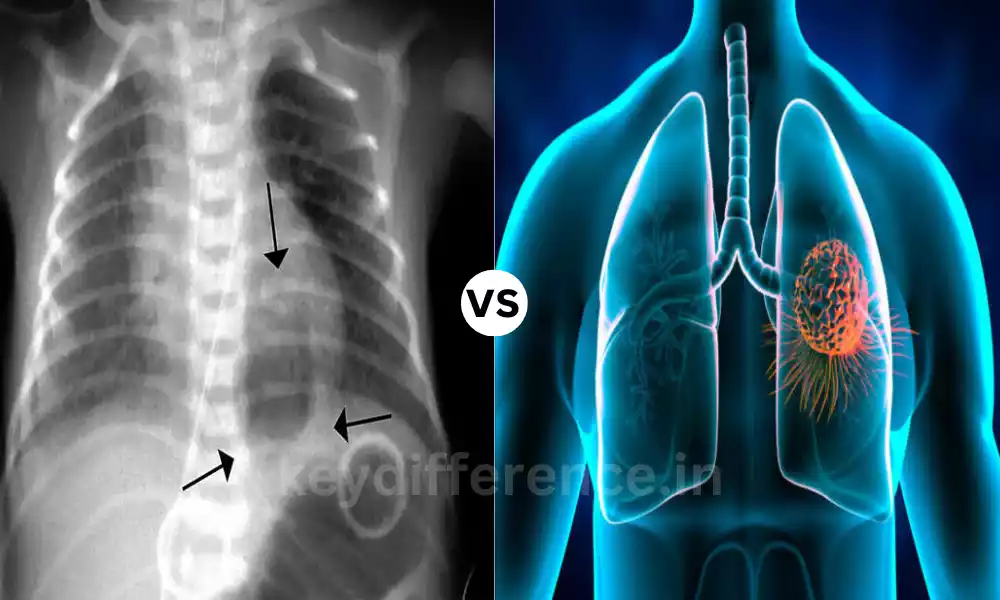
Ischemic Heart Disease and Myocardial Infarction are two closely related cardiovascular conditions affecting the heart. Though similar, these two diseases differ greatly in nature, symptoms, diagnosis, treatment approaches, and management strategies.
Understanding these distinctions is vital in order to promote heart health and avoid life-threatening complications we’ll look at them here in more depth along with definitions, risk factors, symptoms diagnosis management strategies.
Definition of Ischemic Heart Disease
Ischemic Heart Disease (IHD) also known in the form of Coronary Artery Disease (CAD) or Coronary Heart Disease (CHD) is a heart condition that is characterized by a diminished flow of blood to heart muscles as a result of the blockage or narrowing of coronary arteries.
The decreased blood flow is often triggered by the accumulation of plaque and fat deposits within coronary arteries causing the heart to lose the vitality and nutrition it requires to function effectively.
As a chronic illness, IHD can cause a variety of symptoms like angina (chest discomfort or pain) as well as breathlessness and may increase the chance of grave events such as myocardial infarction (heart attack) in cases where the flow of blood into the cardiac muscle becomes affected.
The long-term treatment of IHD usually involves lifestyle changes or medications, as well as medical procedures to ease symptoms and lower the risk of complications.

Definition of Myocardial Infarction
Myocardial Infarction (MI), more commonly referred to as a cardiac attack or heart attack, is a sudden, serious medical condition that develops in the event of a blocked or decreased circulation to a particular part of the muscle that causes the death of the heart muscle cells because of a lack of oxygen supply.
The most common cause is the total occlusion of a coronary artery usually because of break-up of the atherosclerotic artery or the formation of blood clots (thrombus) inside the coronary artery.
In the event of a myocardial heart attack, is when the affected portion of the muscle in your heart is depleted of oxygen, and in the event that blood flow is not quickly restored, it may cause irreparable damage or even death of the heart tissue.
The primary sign of an attack of the heart is severe chest pain that lasts for a long time or discomfort, which can be felt in the left jaw, neck, arm, or back. Other symptoms include breathlessness as well as nausea, sweating, and lightheadedness.
The need for immediate medical attention is vital for a myocardial heart attack to bring back blood flow into the muscle of your heart and reduce the harm.
This is usually accomplished through treatments like thrombolytic therapy (clot-dissolving drugs) or percutaneous coronary intervention (PCI) using angioplasty, the placement of stents, and, in some instances coronary artery bypass surgery (CABG).
A well-planned treatment and lifestyle changes after a heart attack are crucial to avoid the recurrence of cardiac events and help speed the recovery.
Comparison Table of Ischemic Heart Disease and Myocardial Infarction
Here’s a comparison table highlighting the key differences between Ischemic Heart Disease (IHD) and Myocardial Infarction (MI):
| Characteristic | Ischemic Heart Disease (IHD) | Myocardial Infarction (MI) |
|---|---|---|
| Definition | Chronic condition due to reduced blood flow to the heart muscle, often caused by coronary artery narrowing or blockage. | An acute condition resulting from the sudden blockage of a coronary artery, leading to heart muscle cell death. Also known as a heart attack. |
| Nature | Chronic and ongoing, typically with intermittent symptoms. | Sudden and acute, characterized by severe symptoms. |
| Risk Factors | Atherosclerosis, hypertension, hyperlipidemia, smoking, diabetes, family history, obesity, sedentary lifestyle, etc. | Similar risk factors as IHD, but may include additional stress-related factors. |
| Symptoms | Angina (chest pain or discomfort), shortness of breath, fatigue, and palpitations, may vary in severity and duration. | Severe and prolonged chest pain or discomfort, often radiating to the left arm, neck, jaw, or back, accompanied by sweating, nausea, and lightheadedness. |
| Diagnosis | Electrocardiogram (ECG), stress tests, coronary angiography, and imaging (e.g., echocardiography). | ECG changes (ST-segment elevation or depression), elevated blood markers (troponins), and imaging (e.g., echocardiography). |
| Treatment and Management | Lifestyle modifications (diet, exercise, smoking cessation), medications (statins, antiplatelets, beta-blockers), angioplasty, stenting, coronary artery bypass grafting (CABG). | Immediate medical attention (call 911), thrombolytics (clot-dissolving drugs), antiplatelets, beta-blockers, coronary angioplasty, stenting, and cardiac rehabilitation. |
| Long-Term Outlook | Focuses on prevention, long-term management, and symptom control. | Immediate intervention to restore blood flow, followed by long-term management and risk factor control. |
| Complications and Prognosis | Can lead to MI, heart failure, arrhythmias, and other cardiac issues if not managed effectively. The prognosis depends on the severity and extent of coronary artery disease. | Potential complications include heart failure, arrhythmias, cardiogenic shock, and death if not treated promptly. The prognosis varies based on the extent of damage and timely intervention. |
Please note that while this table highlights the primary differences between IHD and MI, these conditions are closely related, and individuals with IHD are at risk of experiencing a myocardial infarction if their coronary arteries become severely blocked or narrowed.
Timely medical attention and proper management are essential for both conditions to minimize risks and promote heart health.
Importance of understanding Ischemic Heart Disease (IHD) and Myocardial Infarction (MI)
Knowing the difference between Ischemic Heart Disease (IHD) and Myocardial Infarction (MI) is essential for a variety of reasons:
- Health awareness: Knowledge of these ailments helps people identify the symptoms and signs, which allows them to seek medical attention if required. It could be the difference between life and life in cases of MI.
- Prevention Measures: Knowing the risk factors that contribute to IHD can help individuals adopt healthy lifestyle changes. This can include adopting a heart-healthy diet, regularly engaging in exercise, quitting smoking, and taking care of conditions like diabetes and hypertension.
- Quick Intervention: Knowing the differences between IHD and acute MI is essential. MI requires medical intervention immediately while IHD requires long-term treatment. Being aware of the time to seek urgent treatment could save lives.
- Treatment compliance: Patients diagnosed with IHD or MI are more likely to follow prescribed medication, lifestyle changes as well and follow-up appointments once they are aware that these actions are crucial to managing their conditions and reducing the likelihood of developing cardiac issues in the future.
- Health Promotion: Awareness and knowledge regarding IHD and MI can improve results for public health. This information can help reduce the incidence rate as well as reduce healthcare costs and better overall cardiovascular health for the general population.
- Medical professionals: Healthcare providers need a thorough knowledge regarding IHD as well as MI to correctly diagnose the condition, and treat and educate patients. Medical professionals play an essential role in the prevention and management of these illnesses.
- Research and development: A better understanding of these conditions is the basis for medical research and development. It is the basis for the development of new diagnostic tools, treatments, and preventive strategies that ultimately improve outcomes for patients.
- Qualities of life: For individuals living with IHD Knowing about the condition helps them manage their symptoms and enjoy an improved standard of living. Knowing about MI can assist patients in making important lifestyle changes to prevent repeating situations.
- Reducing stigma: Understanding IHD and MI can help reduce the stigma that surrounds heart disease. It promotes discussions about heart health and makes it easier for people to seek support and help.
- Community Assistance: Community and support groups for those who are affected by IHD as well as MI benefit from having knowledgeable members who are able to share their experiences, offer emotional support, and encourage positive lifestyle modifications.
Knowing Ischemic Heart Disease and Myocardial Infarction is crucial for the individual and society as a whole. It allows individuals to manage their health and heart condition, get urgent medical treatment, and make lifestyle adjustments to lower the risk of heart-related issues.
It also helps improve public health outcomes as well as advances in the field of cardiovascular medicine.
Reduced blood flow to the heart muscle
The flow of blood into the muscle of the heart often referred to as myocardial Ischemia occurs when the coronary arterial arteries that supply high-oxygen blood supply to heart muscles get narrowed or blocked.
The decreased blood flow could result in a variety of important consequences regarding heart health:
- Reduced Oxygen Supply: When the flow of blood into the cardiac muscle is reduced it indicates that less nutrients and oxygen reach those heart cells (myocardium). This could result in the depletion of oxygen, which could hinder the heart’s ability to perform its duties.
- Chest pain (Angina): One of the most frequent signs of decreased circulation of blood into the heart can be chest discomfort or pain called angina. Angina is a condition that can be severe and can be caused by physical stress or emotional stress when the heart muscle’s requirement for oxygen is greater than the supply.
- Effect of heart Attack: Prolonged or drastic diminution in the flow of blood to the heart may result in myocardial infarction (heart attack). Heart attacks occur in the event of a total blockage to an artery that is coronary, which causes the muscles of your heart to die because of the lack of oxygen.
- Chronic Condition: Reduced blood flow to the heart is a characteristic of diseases such as Ischemic Heart Disease (IHD) or Coronary Artery Disease (CAD). These are chronic diseases that result in atherosclerosis (buildup of plaque within the arteries) gradually narrows the coronary arteries as time goes by.
- Risk Factors: Numerous risk factors, including elevated blood pressure elevated cholesterol, smoking obesity, diabetes and a lack of exercise may result in decreased circulation of blood to your heart.
- Therapy: The management of diminished heart blood flow typically involves lifestyle changes as well as medication (such as statins and antiplatelets) and medical procedures such as angioplasty and stenting to improve blood flow. In the most severe instances, coronary artery bypass grafting (CABG) might be necessary.
Understanding the significance of a reduced supply of oxygen to the muscles in your heart is vital for healthcare professionals and people.
Early diagnosis and management of risk factors and the appropriate treatment could aid in preventing heart attacks as well as improve overall heart health.
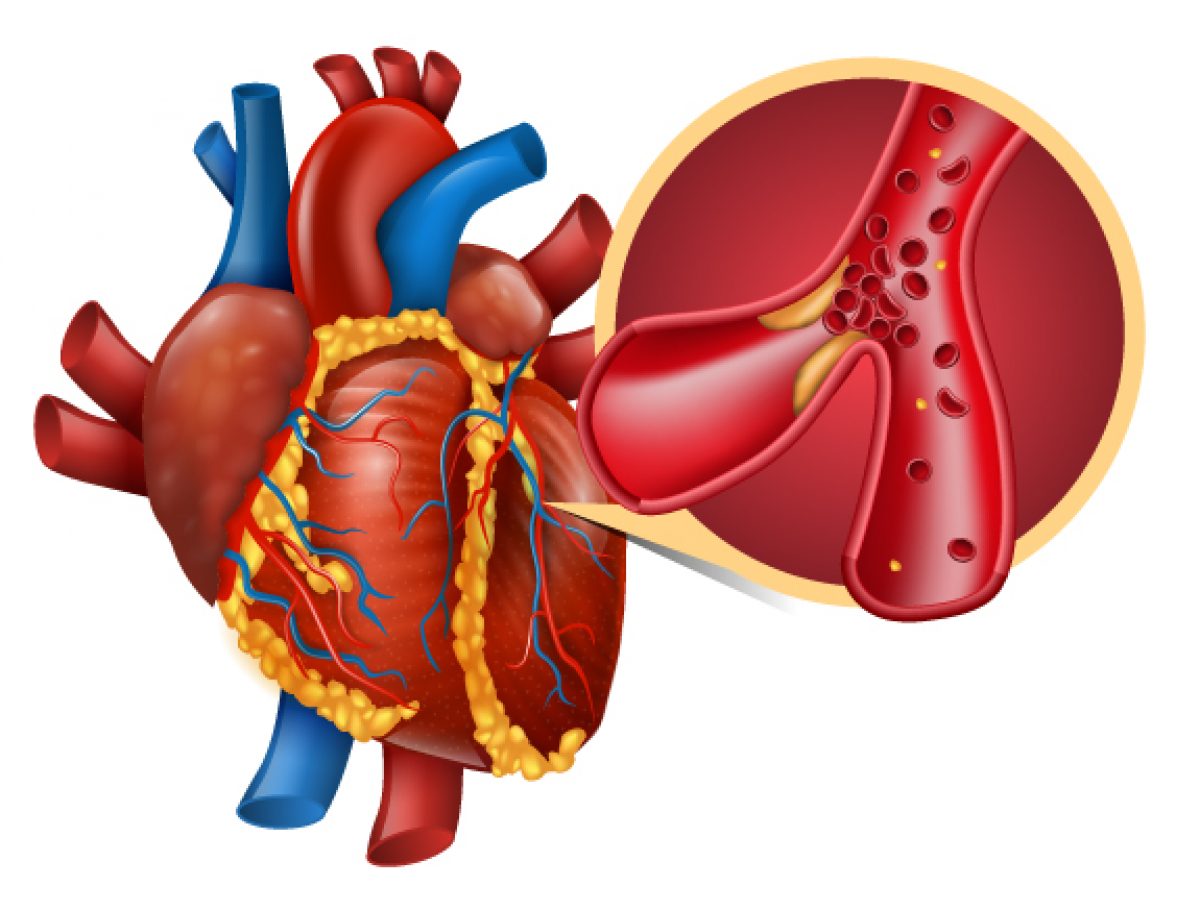
Sudden blockage of a coronary artery
An abrupt blockage in a coronary artery can be an important event that could cause a myocardial injury (MI) often referred to as an attack on the heart. It happens whenever one coronary artery that supplies an oxygen-rich bloodstream to the muscle of your heart is completely blocked.
This is a summary of the procedure:
- Coronary artery blockage: The blockage can be caused by a break of the atherosclerotic plaque. It can also be caused by the formation of a blood clot (thrombus) in the coronary artery. Atherosclerosis is an illness characterized by the accumulation of cholesterol, fatty deposits, and inflammation cells in the walls of the artery as time passes.
- Oxygen Deprivation: If the coronary artery gets blocked, the flow of blood to a particular region in the muscle of your heart suddenly stops. The heart muscles in that region are deficient in oxygen and nutrients.
- Myocardial infarction (Heart attack): The lack of oxygen-rich blood causes muscles of the heart (myocardium) to die in a matter of minutes. The condition is known as myocardial ischemia (MI) also known as heart attack. The degree and severity of heart attacks is dependent upon the severity and position of the artery that is blocked.
- The symptoms: The hallmark symptom of a heart attack is frequently prolonged and severe chest discomfort or pain. The pain could be felt in the left arm and neck, jaw, or even back. Other signs include breathlessness as well as nausea, sweating, and lightheadedness.
- Immediate medical attention: Recognizing the symptoms of an attack on the heart and seeking urgent medical attention is crucial. A quick intervention can help restore the flow of blood to the blockage arterial vein, reduce the damage to the heart muscle, and increase the odds of surviving.
- Treatment: Medical treatments for heart attacks may include thrombolytic treatment (clot-dissolving drugs) antiplatelet drugs beta-blockers, and treatments aimed at restoring blood flow, for instance, the percutaneous coronary interventions (PCI) using angioplasty as well as the placement of stents.
- Long-Term Management: After an event like a heart attack it is crucial to manage the long-term effects to prevent recurrence of incidents. This could include lifestyle changes (e.g. diet, eating habits, and exercises) or medications, as well as heart rehabilitation programs.
An abrupt blockage in a coronary artery is an important circumstance that could lead to an attack on the heart (myocardial infarction). Knowing the causes, signs and the need for immediate medical attention in the event of an attack of the heart is vital in preventing deaths and minimizing the damage to the heart muscle.
Similar risk factors for both conditions
Ischemic Heart Disease (IHD) and Myocardial Infarction (MI) share many risk factors that are common to both because both diseases are closely linked and often interconnected.
Risk factors shared by both conditions include:
- Atherosclerosis: The development of Atherosclerosis can be an important risk factor as well as IHD or MI. It causes the formation of fat deposits (atherosclerotic plaques) within the coronary arteries. This leads to a narrowing and possibly obstruction of the arteries.
- Hypertension (High Blood Pressure): High blood pressure causes stress on the blood vessels and heart and contributes to the development of atherosclerosis, thereby increasing the risk of IHD as well as MI.
- Hyperlipidemia (High Cholesterol Levels): High amounts of cholesterol levels, especially lower-density lipoprotein (LDL) cholesterol, may result in the accumulation of plaque within coronary blood vessels, increasing the risk of developing atherosclerosis, and the subsequent IHD or MI.
- Smoking: Smoking cigarettes is an important threat factor to both. Smoking not only harms blood vessels and increases the risk of atherosclerosis, it can also increase the risk of forming blood clots, which could lead to MI when the coronary artery is blocked.
- Diabetes: Individuals with diabetes have a greater chance of developing atherosclerosis and related complications because of high glucose levels in the blood. The condition can also cause endothelial dysfunction, which can increase the chance of developing both IHD as well as MI.
- Obesity: Obesity or being overweight is linked to the possibility of developing risks such as hypertension, hyperlipidemia, or diabetes. All of these increase the likelihood of having the two conditions: IHD or MI.
- Physical inactivity: A sedentary lifestyle could lead to overweight, high blood pressure, and irregular blood lipid profiles, increasing the risk of developing cardiovascular diseases which include IHD as well as MI.
- Family history: Family history that has a family connection to IHD or MI could be a sign of a genetic predisposition to these diseases, which could increase a person’s risk.
- Age: Ageing is an underlying risk factor for both IHD as well as MI The risk gets higher as we age.
- Genre: Men tend to be more at risk for IHD and MI. IHD and MI, however, the risk increases for women following menopause.
- Stress: Continuous stress may cause high blood pressure and encourage unhealthy coping strategies such as eating too much or smoking, which can increase the likelihood of both.
Understanding and managing these common risk factors is essential for the prevention of the development of both Ischemic Heart Disease and Myocardial Infarction. Changes in lifestyle regular medical check-ups and the right medical intervention can reduce the risk and improve heart health.
IHD symptoms are chronic and may be intermittent
One of the main characteristics that is characteristic of Ischemic Heart Disease (IHD) is that its signs are usually chronic, and could be intermittent. IHD is a chronic illness that is caused by a decrease in blood flow into the muscle of the heart because of the blockage or narrowing of coronary arteries.
This is why the symptoms of IHD are often intermittent and persistent:
- The progressive character of IHD: generally develops gradually over time as a result of atherosclerosis, which is the gradual accumulation of deposits of fatty substances (atherosclerotic plaques) within coronary arteries. The gradual progress may lead to a long-term decrease in the flow of blood into the heart.
- Intermittent symptoms: The severity of IHD symptoms, including angina (chest discomfort or pain) may vary depending on the severity of coronary arterial blockage. In certain cases, if the blockage isn’t too extreme, patients who suffer from IHD might experience symptoms that occur and disappear. The symptoms could be caused by factors such as physical exertion or emotional stress and extreme temperatures.
- Stable angina: The majority of patients with IHD suffer from stable angina which is defined by consistent and predictable symptoms of chest discomfort or pain when performing certain activities, such as going uphill or climbing stairs. This kind of angina tends to ease with relaxation or medications.
- Silent Ischemia: Certain patients with IHD may suffer from silent ischemia. This is when they suffer from a decrease in blood flow to the heart but without any noticeable symptoms. This condition is detected via diagnostic tests, such as ECGs (ECGs) as well as stress tests.
- Unstable Angina: On the contrary unstable angina is the most severe kind of IHD which is characterized by symptoms that fluctuate and can occur even at any time, and could suggest an increased risk of having a heart attack (MI). This isn’t a recurring issue and requires medical attention immediately.
It is crucial for people with IHD to recognize the patterns and extent of their symptoms and collaborate closely with healthcare professionals in order to take care of the illness efficiently.
Lifestyle changes, medication as well and cardiac rehabilitation may aid in reducing symptoms, preventing the progression of the disease, and lowering the risk of complications such as myocardial infarction (heart attack). Regular follow-up with your health professional is crucial to check and modify the treatment plan when required.
IHD management is typically long-term and focuses on prevention
Absolutely, the treatment for Ischemic Heart Disease (IHD) is usually long-term and focuses on prevention. IHD can be a long-lasting illness that is characterized by a decrease in oxygen flow in the muscle of the heart because of coronary artery narrowing or blockage.
This is why long-term treatment and prevention is crucial:
- Chronic Nature: IHD is considered to be a long-lasting illness, meaning that it continues to be present for an extended time. The root cause of the disease, atherosclerosis (plaque accumulation in the arteries) tends to advance slowly as time passes. So controlling IHD is a continual process.
- Avoid Complications: The principal objective of long-term treatment is to avoid complications such as myocardial artery infarction (heart attack) heart failure and arrhythmias. By reducing risk factors, and slowing the progression of atherosclerosis issues are often prevented.
- Lifestyle modifications: Changes in lifestyle play an integral aspect when it comes to IHD management. This could include adopting an eating plan that is heart-healthy as well as getting active regularly as well as quitting smoking and keeping an ideal weight. These practices not only relieve symptoms but also address the fundamental causes behind IHD.
- Medicines: The majority of patients with IHD require ongoing medication management to manage blood pressure, reduce the levels of cholesterol, control diabetes, and lower the chance of developing blood clots. The use of antiplatelets, beta-blockers, statins, along with ACE inhibitors are often utilized in IHD treatment.
- Regular Check-ups: Ongoing monitoring through regular visits to a health professional is crucial. This permits the evaluation of the risk factors, medication adjustments, and early detection of any changes to the health.
- Risk Factor Management: The management and control of risk factors, like hypertension, hyperlipidemia, and diabetes, is a crucial element in IHD prevention. Through effective management of these risk factors and preventing the progression of atherosclerosis, it is possible that it is slowed or stopped.
- Cardiac Rehabilitation: Rehabilitation programs for cardiac health are frequently recommended for those suffering from IHD. They provide exercise that is supervised education on healthy living and emotional support for individuals to get back and keep the health of their heart.
- Psychological well-being: Controlling stress and dealing with issues with mental health are crucial components in IHD management. Techniques for reducing stress and aiding emotional well-being can help improve the health of the heart.
- Self-Care and Education: Patients and their families are frequently educated about the symptoms, and conditions as well as how important it is to take care of themselves. Ensuring that people are educated can help them play an active part in their personal health.
long-term treatment and strategies to prevent IHD are essential for enhancing living quality for people suffering from IHD, lessening the risk of complications, and healthier heart health for those suffering from this condition.
Reference Books
Certainly, here are some reference books on various topics that you might find valuable depending on your interests and needs:
- Medicine and Health:
- “Harrison’s Principles of Internal Medicine” by Dennis L. Kasper et al.
- “Robbins and Cotran Pathologic Basis of Disease” by Vinay Kumar et al.
- “The Emperor of All Maladies: A Biography of Cancer” by Siddhartha Mukherjee.
- Science:
- “Cosmos” by Carl Sagan.
- “A Brief History of Time” by Stephen Hawking.
- “Sapiens: A Brief History of Humankind” by Yuval Noah Harari.
- History:
- “A People’s History of the United States” by Howard Zinn.
- “Guns, Germs, and Steel: The Fates of Human Societies” by Jared Diamond.
- “The Second World War” by Sir Winston S. Churchill.
- Psychology and Self-Help:
- “Thinking, Fast and Slow” by Daniel Kahneman.
- “The Power of Habit: Why We Do What We Do in Life and Business” by Charles Duhigg.
- “Man’s Search for Meaning” by Viktor E. Frankl.
- Fiction and Literature:
- “To Kill a Mockingbird” by Harper Lee.
- “1984” by George Orwell.
- “The Great Gatsby” by F. Scott Fitzgerald.
Conclusion
Reference books are useful sources that cover a variety of subjects, ranging from science and medicine to psychology, history, and more. They offer in-depth information about the subject, as well as insights and perspectives that are vital for learning, research, and personal growth.
If you’re looking to broaden your knowledge of a topic or just want an enjoyable read the reference books provide an abundance of information and ideas.