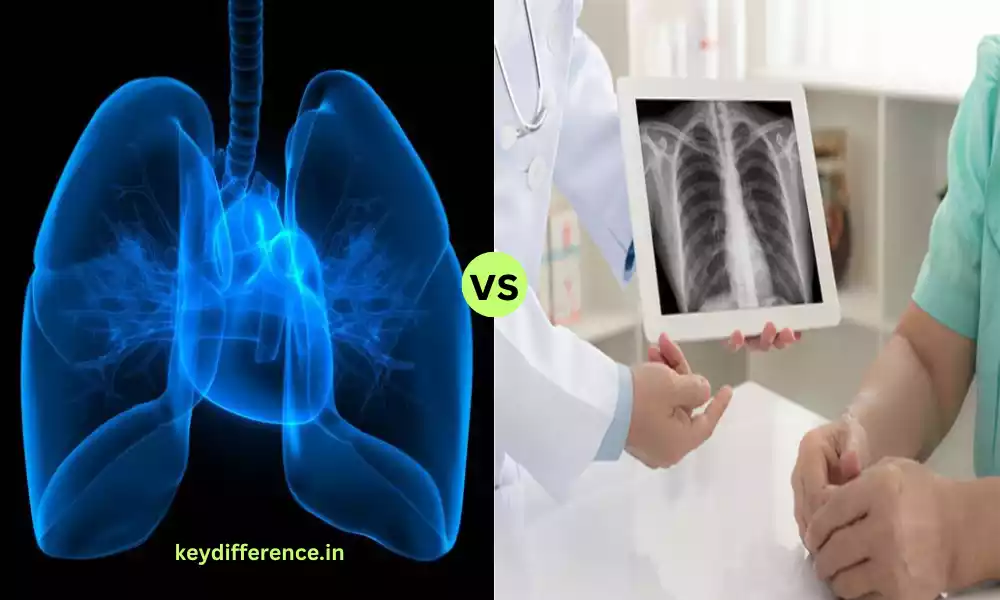
Atelectasis and Pneumonia are respiratory illnesses that can affect the lungs. However, they have distinct distinctions in their pathophysiology, causes, and clinical manifestations. We will look at the differences and similarities between the two conditions, highlighting the importance of an accurate diagnosis and the proper treatment for the best patient care.
Definition of Atelectasis
Atelectasis is a term that refers to the condition wherein a portion or the entire lung is unable to breathe or becomes airless which results in the loss of lung function. It happens when the air sacs of the lung, referred to as alveoli, shrink or do not expand completely and prevent the exchange of carbon dioxide and oxygen.
Atelectasis may be caused by many causes, such as blockages of the airway pressure external to the lung, and insufficient production of surfactants, vital to keep the alveoli afloat. Atelectasis symptoms can include chest pain or decreased oxygen levels in blood.

Definition of Pneumonia
Pneumonia is an inflammatory lung disease that is characterized by inflammation and infection in the air sacs (alveoli) in either or both of the lungs. It is usually caused by viruses, bacteria, or other microorganisms in addition to non-infectious elements such as chemical irritants or the aspiration of foreign substances.
Pneumonia can result in the build-up of pus and other fluids within the affected parts of the lungs. This can affect their ability to oxygenate blood efficiently. The typical symptoms of pneumonia are cough, fever, and breathing difficulties as well as chest pain. the production of sputum or mucus.
The severity of the condition can vary from mild instances that are manageable at home, to more severe cases that require hospitalization or intensive medical treatment. The early diagnosis and the appropriate treatment are essential to avoid complications and aid in healing.

Importance of Distinguishing Between Atelectasis and Pneumonia
The distinction between atelectasis and pneumonia is crucial in the field of clinical practice due to a number of reasons:
- Appropriate treatment: Atelectasis and pneumonia require different treatment strategies. In the majority of cases, atelectasis requires intervention to re-inflate the lung tissue while pneumonia generally needs antibiotics in order to manage the root infection. A precise diagnosis will ensure all patients are treated with the appropriate treatment, increasing their odds of healing.
- Preventing Overuse of Antibiotics: Incorrectly diagnosing atelectasis with pneumonia could result in unnecessary antibiotics being prescribed, resulting in resistance to antibiotics and exposing patients to possible adverse reactions to these drugs. A precise differentiation can help avoid the unnecessary use of antibiotics.
- Cutting down on Healthcare Costs: Inadequate hospitalizations, tests, or treatments resulting from misdiagnoses could cause increased healthcare costs for patients and healthcare providers. A precise diagnosis can help allocate funds more effectively.
- Beware of complications: Failure to distinguish between these two conditions could cause delays in dealing with the root cause. For instance, if an atelectasis diagnosis is misinterpreted as pneumonia, the actual cause of the collapse of the lung may remain untreated, which could lead to complications.
- Patient Well-being: An accurate and prompt diagnosis can lead to better outcomes and better health. A well-managed treatment for each disease can help relieve symptoms, avoid complications, and accelerate the recovery process.
- Clinical Decision-Making: Healthcare professionals depend on accurate diagnosis to make informed choices about the treatment of patients. The distinction between pneumonia and atelectasis is the basis for deciding on treatments and diagnostic tests.
- Research and Data Collection: A precise diagnosis is crucial in studies of epidemiology as well as clinical trials and the collection of data in healthcare. It is essential to ensure that the correct information is collected for each illness and, in turn, helps inform healthcare policies and practices.
Recognizing pneumonia and atelectasis is essential to provide patients with the most efficient and appropriate treatment as well as avoiding costly healthcare expenses and avoiding the excessive use of antibiotics. An accurate diagnosis is the key to better outcomes for patients and more efficient healthcare systems.
Anatomy and Physiology of the Respiratory System
The respiratory system comprises a complicated structure and organs which are responsible for exchanging gases specifically carbon dioxide (O2) along with carbon dioxide (CO2) in the external. Understanding the anatomy and physiology is vital to understanding the mechanism that involves breathing as well as gas exchange.
Anatomy of the Respiratory System:
- Nose as well as Nasal Cavity: The respiratory system starts with the nose. There, air is drawn into nasal passages. Nasal cavities are lined by mucous membranes as well as tiny hair-like structures, called cilia that help in filtration, humidification, and warm inhaled air.
- Pharynx (Throat): The Pharynx is an open passageway that can be used for food and air. It connects the mouth and nasal cavity to the larynx and esophagus.
- The larynx (Voice Box): The larynx has vocal cords, and is responsible for the production of voice. It also acts as a safeguard mechanism that prevents liquids and food from getting into the respiratory tract lower.
- Trachea (Windpipe): The Trachea is a tube comprised of a cartilage ring. It carries air from the larynx to the bronchi. The trachea’s walls are lined by mucus-producing cells and cilia to aid in the removal of foreign particles.
- Bronchi as well as Bronchioles: The trachea divides into two major bronchi that enter each lung. The bronchi then split into smaller bronchioles. They are used as passageways for air to get to the alveoli.
- The lungs: The lungs are the main respiratory organs comprised of the left and right lungs which are enclosed by the pleura which is a membrane that is double-layered. Each lung has lobes (the right lung contains three and the left has 2) as well as millions of air sacs, also known as alveoli.
- Alveoli: Alveoli are the sites where gas exchange happens. They are enclosed by a tangle of tiny blood vessels (capillaries). Air vapors from breathing diffuse into the bloodstream, whereas carbon dioxide in the bloodstream is absorbed by the alveoli for exhalation.
Physiology of the Respiratory System:
- Ventilation: The process of ventilation refers to the procedure of moving air inside the lung. It has two phases exhalation (inspiration) as well as exhalation (expiration). The intercostal muscles and the diaphragm play an important role in causing changes to the thoracic volume, which facilitates these processes.
- Gas Exchange: Gas exchange happens in the alveoli. Air vapor from inhalation is absorbed by hemoglobin in red blood cells. It is then transferred to tissues of the body to aid in cell respiration. Carbon dioxide, which is an end product of cell metabolism, is transported to the alveoli, where it is exhaled.
- Respiratory Control: The regulation of breathing is controlled via the breathing control centers within the brainstem, particularly the pons and medulla oblongata. These areas respond to changes in blood levels of carbon dioxide, oxygen, and pH, allowing them to adjust the intensity and rate of breathing.
- Respiratory Muscles: The diaphragm and intercostal muscles and the other muscles that are associated with them are essential to breathing’s mechanics. The contraction and relaxation of these muscles cause changes in the volume of the thoracic cavity and facilitate air movement.
- Gas Transport: The oxygen is carried through the bloodstream, mostly linked to hemoglobin within hemoglobin-containing red blood cells. Carbon dioxide is transported in the bloodstream in three different forms: dissolving in plasma and hemoglobin as bicarbonate Ions.
Knowing the anatomy and physiology of the respiratory system is crucial to understanding the way that our body uses oxygen for energy production. It also eliminates carbon dioxide, which is a metabolic waste product. It helps to understand respiratory diseases and the treatment they require.
Comparison Table of Atelectasis and Pneumonia
Here’s a comparison table outlining the key differences between atelectasis and pneumonia:
| Characteristic | Atelectasis | Pneumonia |
|---|---|---|
| Definition | Lung collapse or incomplete expansion of lung tissue. | Infection and inflammation of lung tissue, particularly the alveoli. |
| Etiology | Various causes, including obstruction, compression, resorption, or adhesion of lung tissue. | Typically caused by bacteria, viruses, or other microorganisms, but can also result from chemical irritants or aspiration. |
| Primary Mechanism | Reduction in lung volume due to the collapse of alveoli. | Infection and inflammation lead to the filling of alveoli with pus and other fluids. |
| Symptoms | Shortness of breath – Rapid breathing – Chest discomfort or pain – Decreased breath sounds on the affected side | Fever – Cough with mucus production – Difficulty breathing – Chest pain – Fatigue and weakness |
| Radiological Findings | Lung collapse or consolidation – Shift of mediastinum (if severe) | Infiltrates or opacities on chest X-ray or CT scan – Consolidation of lung tissue – Air bronchograms (visible airway shadows) |
| Diagnosis | Physical examination – Chest X-ray or CT scan – Bronchoscopy (in some cases) | – Physical examination – Chest X-ray or CT scan – Blood tests – Sputum culture (to identify the causative organism) |
| Treatment and Management | Address the underlying cause (e.g., remove airway obstruction) – Breathing exercises – Chest physiotherapy – Oxygen therapy | Antibiotics (if bacterial) – Antiviral medications (if viral) – Supportive care (rest, fluids, and fever reducers) – Oxygen therapy – Mechanical ventilation (in severe cases) |
| Prognosis | Generally good when the underlying cause is treated promptly. | Prognosis varies depending on the type of pneumonia, the patient’s overall health, and the speed of diagnosis and treatment. |
It’s important to note that while this table highlights the primary differences between atelectasis and pneumonia, both conditions can present with respiratory symptoms, and accurate diagnosis by a healthcare professional is essential for appropriate management. Additionally, some symptoms and radiological findings may overlap in certain cases, making a comprehensive evaluation crucial.
Treatment and Management of Atelectasis
The treatment and management of atelectasis are primarily based on the cause of the condition as well as the seriousness of the problem. The objective of managing atelectasis is to rebuild the lung tissue that has collapsed and improve lung function.
These are some common strategies for treating and managing atelectasis:
- Address Underlying Causes:
- Airway Clearance: In the case of mucus or obstruction by foreign bodies Clearing the airway is crucial. This can be accomplished through methods like the practice of deep breathing, coughing, and physiotherapy of the chest.
- Elimination of Blockages: In certain situations medical procedures like bronchoscopy are required to eliminate obstructions.
- The Treatment for Infections: If the cause of atelectasis can be traced to the presence of an infection antiviral or antibiotic medications are recommended to treat the underlying infection.
- Breathing Exercises and Chest Physiotherapy:
- Deep breathing exercises, incentives for diaphragmatic breaths, and spirometry techniques can improve lung capacity and stop further collapse.
- Chest physiotherapy, which is performed by a respiratory therapist could include techniques like the use of percussion or postural drainage to assist in mobilizing secretions and assist in lung expansion.
- Oxygen Therapy: When atelectasis causes a decrease in blood oxygen levels supplemental oxygen can be provided to ensure adequate oxygenation.
- Incentive Spirometry: Patients are urged to utilize an incentive spirometer. It is a device that can help improve lung function by encouraging deep breathing and long-term lung expansion.
- positioning: Changing a patient’s posture by turning or sitting up can assist in facilitating lung expansion by spreading air in the lung.
- Suctioning: Sometimes suctioning is necessary to eliminate excess mucus or secretions that block the airways.
- surgery: In rare cases when atelectasis results from structural problems (e.g. tumors compressing the airways) surgery may be required to treat the root cause.
It’s crucial to understand that prevention is usually the best approach to managing the treatment of atelectasis. This means early mobilization and walking (especially following surgery) as well as coughing and breathing exercises that are deep, as well as managing risk factors like smoking and quitting.
The precise treatment plan for atelectasis needs to be formulated by a physician according to the individual conditions, including the underlying reason and general health of the individual. The need for prompt intervention is vital to avoid complications and aid in the recovery of lung function.
Similarities Between Atelectasis and Pneumonia
Although atelectasis and pneumonia can be distinguished as respiratory diseases with different origins and pathophysiologies are some commonalities between them, specifically regarding their clinical presentation as well as their impact on the respiratory tract. Here are a few commonalities:
- Respiratory symptoms: Both atelectasis and pneumonia can be accompanied by respiratory symptoms, including:
- Breathlessness (dyspnea)
- Breathing that is shallow or rapid
- The chest may be painful or uncomfortable.
- Coughing
- Trouble breathing (especially when you are working)
- The sound of breath is less frequent during physical examination
- Imaging Findings: Imaging studies of the chest, like the X-rays and CT scans, could reveal abnormalities for both of the following conditions:
- Atelectasis may manifest as a swollen or consolidated part of the lungs.
- Pneumonia is often accompanied by anatomical evidence of lung infiltrates, consolidation, or the presence of opacities.
- Complications: Both conditions can cause complications, but they are different in nature. problems may be different:
- In atelectasis, the complications could consist of the development of pneumonia (secondary infection) as well as a decrease in oxygen saturation and respiratory distress, If not treated promptly.
- Pneumonia can cause severe respiratory distress, sepsis, abscess development, or pleural effusion If not treated properly.
- Reduced Lung Function: Both of these conditions can cause a decrease in lung function, as well as impairment of gas exchange because of impaired alveolar function. This may result in decreased oxygen levels in the blood and an increase in carbon dioxide levels.
- Diagnostic Overlap: The clinical evaluation for patients suffering from respiratory symptoms typically requires identical diagnostic procedures for the two conditions like physical examination, chest imaging, or blood tests. The process of distinguishing between them usually involves a thorough examination and analysis of the patient’s medical history, risk factors, and any additional diagnostic findings.
- Importance of timely diagnosis and Treatment: A timely diagnosis and the appropriate treatment are essential for both atelectasis as well as pneumonia to prevent complications, maximize the outcomes of treatment, and improve lung function.
Despite these commonalities, it’s crucial to note that atelectasis as well as pneumonia have different mechanisms, causes, and treatment methods. A precise differentiation of medical professionals is crucial in order to provide appropriate treatment and enhance the patient’s outcomes.
The Role of Healthcare Professionals in Differentiating Atelectasis and Pneumonia
The work of health professionals, especially doctors and respiratory therapists is vital in correctly discerning between the two conditions of atelectasis and pneumonia. The distinction between the two respiratory diseases involves a combination of clinical assessment, diagnostic tests, and medical knowledge.
Here’s a brief outline of the role that health experts play during this distinction process:
- Clinical Assessment:
- The nurses and physicians collect an extensive medical history that includes information on the patient’s health issues including recent surgeries, any underlying health issues, and potential risk factors for respiratory illnesses.
- Physical Examination:
- Healthcare specialists perform a thorough physical examination taking note of breathing indicators like breathing sounds, chest movements, and other signs of discomfort.
- Diagnostic Tests:
- Chest X-rays: These are usually the first imaging studies that are conducted. Radiologists and physicians analyze images to determine the most characteristic features related to atelectasis, or pneumonia. For example, atelectasis can be seen as an isolated lung collapse or as a rounded opacity while pneumonia can show areas of infiltrates or consolidation.
- Computed Tomography (CT) Scans: In more complex instances or when X-rays aren’t conclusive, CT scans provide more precise images. Physicians and radiologists review the scans to determine the lung’s anatomy as well as bronchial anatomy and possible signs of infection.
- Blood tests: Laboratory professionals may test blood samples to look for indications of inflammation, infection, and alterations in blood gas levels. This will help distinguish between ailments.
- Sputum Culture: In the event of a suspicion that pneumonia has occurred, health professionals can obtain sputum samples for a culture to determine the microorganism that caused the problem.
- Respiratory Therapists:
- Respiratory therapy professionals play a crucial role in evaluating lung function by using techniques such as spirometry arterial blood gas (ABG) analysis and pulse oximetry to assess the degree of impaired oxygenation and impairment to ventilation.
- Consultation and Collaboration:
- Healthcare professionals frequently collaborate with specialists, for example, infectious disease specialists or pulmonologists in cases that require specific expertise or treatments.
- Treatment Planning:
- Based on the diagnosis, health experts, specifically physicians, design a treatment plan based on the particular situation. For atelectasis, this might be as simple as addressing the causes and using methods to expand the lung tissue that has collapsed. For pneumonia, treatment usually includes antibiotics or antiviral medicines, along with supportive treatment.
- Monitoring and Follow-up:
- Healthcare professionals continuously track the progress of patients, altering the treatment plan as needed and making sure that the selected treatment options are successful. The follow-up appointment and imaging tests could be scheduled to determine the patient’s recovery.
- Patient Education:
- Healthcare professionals instruct patients and their family members about the causes of their condition the importance of compliance with treatment and the best strategies to prevent the occurrence of respiratory problems in the future.
A precise distinction between atelectasis as well as pneumonia is vital to provide those suffering from pneumonia with effective and efficient treatment. The efforts of health professionals collecting clinical information, conducting diagnostic tests, and applying their expertise in medicine are essential to achieving this goal and ensuring the best patient outcomes.
Conclusion
It is crucial to differentiate between pneumonia and atelectasis. is crucial for healthcare professionals to offer prompt and appropriate care to patients suffering from respiratory symptoms. Although these two conditions might have some commonalities they are distinct in their reasons, diagnosis findings, and treatment methods.
The dedication of healthcare professionals involved in the field of clinical evaluation, diagnostic testing along treatment plans is crucial to ensure precise differentiation and, ultimately improve the patient’s outcomes and overall well-being.