Monitoring Blood Sugar and Urine Sugar levels is essential to maintaining good health for those living with conditions like diabetes.
Two of the primary methods used to assess glucose levels in our bodies are through blood and urine measurements understanding how these methods differ will allow for effective health management.
We’ll dive deeper into their significance for overall well-being and explain more fully their significance versus significance differences between blood and urine measurements.
What is Blood Sugar?
Blood sugar (also referred to as blood glucose) refers to the concentration of glucose (a type of sugar) present in one’s bloodstream.
Glucose serves as an energy source for cells throughout the body and its levels are carefully managed in order to ensure that proper bodily functions occur.
Blood sugar levels may fluctuate throughout the day depending on factors like diet, physical activity, and even the body’s own regulatory mechanisms.
Measurement of blood sugar levels is an integral component of managing conditions like diabetes, where the body’s ability to control its own metabolism becomes impaired.
Blood sugar levels are measured in milligrams per deciliter (mg/dL). The normal range can differ depending on the time of day or meal history – generally speaking, a fasting blood sugar level below 100 mg/dL is considered normal, while anything beyond this threshold could indicate impaired glucose tolerance or diabetes.
Monitoring blood sugar levels is critical for those living with diabetes in order to ensure that their glucose levels stay within safe limits.
High blood sugar, known as hyperglycemia, can lead to various health complications over time including damage to blood vessels, nerves, and organs, low blood sugar (hypoglycemia) can result in symptoms like dizziness, confusion, or even loss of consciousness if left unattended.
At home and healthcare facilities alike, different methods exist for determining blood sugar levels traditional fingerstick tests with glucose meters, continuous glucose monitoring devices (CGM), and laboratory blood tests are all options available to individuals and healthcare providers for taking measurements that,
provide insight into managing and preventing complications related to blood sugar. These measures assist individuals as well as healthcare professionals make more informed decisions when managing and treating this chronic disease.

What is Urine Sugar?
Urine sugar refers to the presence of glucose (sugar) in urine. Urine sugar testing was once widely used as a diagnostic tool for diabetes and other conditions that affect blood sugar levels.
Modern medical practices have generally moved away from urine sugar testing in favor of more accurate methods for measuring blood sugar directly through the bloodstream.
When blood sugar levels are elevated, kidneys may not be able to absorb all of the glucose filtered from the blood, as a result, some glucose may end up in urine causing it to contain sugar.
Urine sugar testing involves collecting urine samples and using chemical reagents to detect its presence – this could provide some indication as to the individual’s blood sugar levels, although only with limited accuracy.
Key Points about Urine Sugar:
Urine Sugar Testing Has Limited Accuracy: Urine sugar testing may not provide real-time information about blood sugar levels instead, its presence reflects past levels. Urine sugar testing might not give an accurate representation of the current state.
Diagnostic Significance: Urine sugar testing was once an important way of diagnosing diabetes elevated urine sugar levels could signal high blood sugar and indicate diabetes, its diagnostic value has become far less specific compared to more precise blood tests.
Urine Sugar Testing Is Less Frequent: With advancements in medical technology such as blood glucose meters and continuous glucose monitoring devices, urine sugar testing has become less prevalent. Modern methods directly measure blood sugar levels for more accurate and immediate data.
Urine Sugar Testing Is Not Advisable: Urine sugar testing should not be used as an accurate means to monitor blood sugar levels regularly, particularly for people living with diabetes. Current devices offer more accurate ways to keep tabs on one’s blood sugar.
Urine sugar testing was once used as an accurate and reliable means to assess blood sugar levels, More accurate and reliable methods such as blood glucose meters and continuous glucose monitoring have largely replaced it as more accurate methods to directly measure and provide insights for managing conditions like diabetes.

Comparison Table of Blood Sugar and Urine Sugar
Certainly, here’s a comparison table outlining the differences between blood sugar and urine sugar:
| Aspect | Blood Sugar | Urine Sugar |
|---|---|---|
| Measurement | Direct measurement of glucose in the bloodstream. | Indirect measurement of glucose in the urine. |
| Real-time Information | Provides real-time information about glucose levels. | Reflects past glucose levels and is not immediate. |
| Accuracy | Highly accurate and reliable for current levels. | Less accurate and influenced by multiple factors. |
| Diagnostic Significance | Crucial for diabetes diagnosis and management. | Historically used for diabetes diagnosis, now less common. |
| Monitoring | Essential for managing diabetes and health. | Not recommended for regular monitoring due to limitations. |
| Method | Uses blood glucose meters, CGMs, and lab tests. | Involves urine samples and chemical reagents. |
| Health Implications | Helps prevent complications of hyperglycemia. | Limited role in health management due to its limitations. |
| Immediate Feedback | Provides immediate feedback on glucose levels. | Delayed feedback due to the need for urine collection. |
It’s important to note that while blood sugar testing is the primary method for accurately assessing glucose levels in the body, urine sugar testing has historically been used for diagnostic purposes, but its accuracy and relevance have diminished with advancements in medical technology.
Diabetes and Blood Sugar Management
Diabetes is a long-term medical condition characterized by elevated levels of blood sugar (glucose). Insulin, produced by the pancreas, helps regulate glucose levels in the bloodstream, proper management of blood sugar for people living with diabetes is critical to avoid complications and maintain overall health.
Below is an overview of diabetes and blood sugar management:
Types of Diabetes:
Type 1 Diabetes: This form results from an immune response attacking and destroying insulin-producing cells in the pancreas, leaving people living with it dependent upon injections or an insulin pump to manage their blood sugar.
Type 2 Diabetes: This form is the most prevalent, often related to lifestyle factors like obesity and physical inactivity. Although the body still produces insulin, cells often become resistant to its effects, treatment includes lifestyle adjustments, oral medications, and sometimes insulin treatments.
Blood Sugar Management:
Proper blood sugar management is critical in order to avoid short and long-term complications associated with diabetes. The goal should be to keep blood sugar levels within an acceptable target range to minimize hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar).
Here’s how blood sugar is managed:
Monitoring: Regular blood glucose meters or continuous glucose monitoring (CGM) devices provide invaluable data for making necessary medication, diet, and activity adjustments.
Medication for diabetes may include insulin injections, oral medications to increase insulin sensitivity or decrease glucose production, as well as other drugs which affect blood sugar levels.
Diet: Eating healthily by controlling carb intake is key. Carbs play an integral role in blood sugar regulation managing portion sizes and selecting complex carbohydrates can help stabilize glucose levels and help maintain stable glucose levels.
Physical Activity: Exercise can increase insulin sensitivity and help control blood sugar, but adjustments may be needed in order to avoid hypoglycemia during or post-exercise.
Insulin Therapy: Individuals living with either Type 1 or Type 2 diabetes may require insulin therapy, typically through injections or an insulin pump.
Stress Management: High-stress levels can have an adverse impact on blood sugar levels. Meditation, relaxation techniques, and adequate rest all play an essential part in maintaining better control.
Education and Support: Diabetes education enables individuals to understand their condition, make informed decisions, and effectively manage blood sugar. Support from healthcare providers and diabetes communities can also be invaluable.
Long-Term Complications: Uncontrolled blood sugar levels over time can lead to complications that affect various organs, including the eyes, kidneys, nerves, and the cardiovascular system. Regular management helps reduce the risk of these complications.
Effective diabetes management entails closely monitoring blood sugar levels, adhering to medication and treatment plans, adopting a balanced diet, engaging in physical activity regularly, and making lifestyle adjustments to optimize blood sugar control.
Consulting healthcare providers for guidance is also critical to long-term management success.
Measuring blood sugar levels yourself
Measuring blood sugar levels on your own is an integral component of diabetes management, particularly for individuals who must monitor their glucose levels regularly. Doing this enables you to make informed decisions regarding medication, diet, and lifestyle options to maintain healthy levels.
Here’s how you can measure blood sugar yourself:
1. Gather Your Supplies:
A reliable blood glucose meter is recommended by your healthcare provider. Test strips for use with that particular meter. Lancing device – this device helps prick your finger for taking blood samples.
Lancets: Small, sterile needles for use with the lancing device.
2. Prepare for Testing: Wash your hands thoroughly with warm water before testing to increase blood circulation and remove any residue that might interfere with readings. Insert a new lancet into your lancing device before commencing testing.
3. Retrieve Blood Sample:
Use a lancing device to puncture the side of your fingertip, alternative sites may also be recommended by healthcare providers. Squeeze gently for at least 5 seconds in order to extract blood samples for testing.
4. Test Your Blood: Insert a test strip into your glucose meter as directed.
5. Test Strip To Blood Drop:
Touching one end of a test strip directly against a drop of blood causes it to be analyzed by your meter, which then displays your blood sugar level on the screen.
5 Record Your Readings:
Document all blood sugar readings along with their date and time in either a logbook or a diabetes management app for safe keeping.
6. Interpret the Results:
To properly interpret your blood sugar results, compare them against the target range suggested by a healthcare provider. This allows you to understand whether your levels fall within or outside that desired range.
Before performing blood testing, ensure your hands are clean to reduce contamination. Also make sure your meter is in working condition and calibrated appropriately, using new lancets for painless blood samples and adhering to any instructions from its manufacturer.
Additional option for monitoring glucose levels
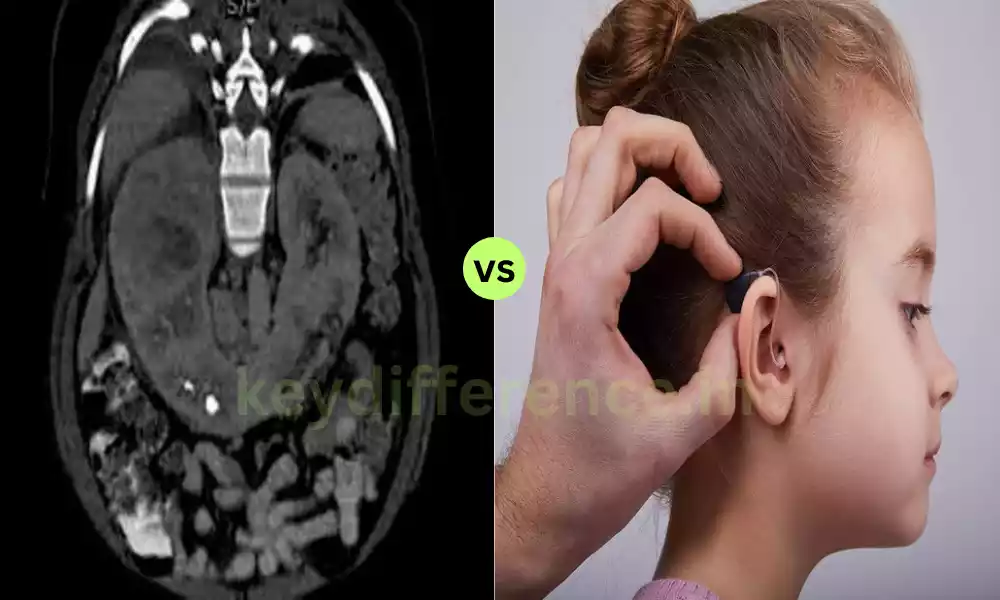
Continuous Glucose Monitoring (CGM) systems offer another advanced option for tracking glucose levels: real-time insights into your blood sugar levels that allow you to better manage diabetes.
Here is an overview of CGMs as a more advanced option in glucose monitoring:
Continuous Glucose Monitoring (CGM):
How It Works: A CGM system comprises three primary components.
Sensor: For glucose monitoring, a small, flexible sensor must be implanted just beneath the skin – often on an abdomen or arm – in order to measure levels in interstitial fluid (liquid between cells) throughout both day and night.
Transmitter: Once data from the sensor reaches a wireless transmitter, this information can then be relayed onward to receivers such as smartphones and compatible devices.
Receiver/Device: A receiver displays real-time glucose readings, trends, and alerts in real-time. Some systems connect wirelessly with smartphones or smartwatches for convenient monitoring on the go.
Advantages of CGMs:
Real-Time Monitoring: CGMs provide real-time glucose data, showing how levels change throughout the day, providing real-time insight, and helping identify patterns or trends that would go undetected with traditional fingerstick tests.
Trend Information: CGMs provide trend information, showing whether your glucose levels are rising, falling, or staying stable over time. This allows you to anticipate and manage highs and lows as they arise.
Alerts and Alarms: CGMs can be set to provide alerts for both high and low glucose levels, making them especially helpful in avoiding serious hypoglycemia or hyperglycemia episodes.
Reports with Insightful Visualizations: Many CGM systems offer reports and visualizations that offer useful insights into your glucose management over time.
Reduced Fingersticks: While CGMs require calibration with fingerstick tests, their usage results in significantly fewer manual tests compared with traditional monitoring systems.
Considerations: CGM systems need proper insertion and calibration for accurate readings. Sensor accuracy varies, making calibration necessary to provide reliable data.
CGM systems include sensors and transmitters which may increase costs over traditional meters. They require regular calibration or sensor replacement every 7-14 days depending on the system used. Some CGMs require professional guidance for use, and to start, in addition to prescription.
Popular CGM Brands:
Whilst many different CGM brands exist on the market today – such as:
Dexcom and Medtronic
Abbott’s FreeStyle Libre CGMs can be an invaluable aid for people living with diabetes who wish to gain a more detailed insight into their glucose levels and trends.
If this option interests you, talk with your healthcare provider first in order to assess if it fits with your situation as well as to find guidance in selecting and using an ideal system for you.
Reference Books
Certainly, here are some reference books that you might find helpful for learning more about monitoring glucose levels and managing diabetes:
- “Think Like a Pancreas: A Practical Guide to Managing Diabetes with Insulin” by Gary Scheiner
- This book offers practical advice on managing diabetes and insulin therapy. It covers topics such as blood sugar monitoring, carbohydrate counting, and insulin adjustments.
- “Using Insulin: Everything You Need for Success with Insulin” by John Walsh, P.A., C.D.E., and Ruth Roberts, M.A.
- A comprehensive guide to using insulin effectively, including information on blood sugar monitoring, insulin types, dosing strategies, and troubleshooting.
- “The First Year: Type 2 Diabetes: An Essential Guide for the Newly Diagnosed” by Gretchen Becker
- Geared toward those newly diagnosed with Type 2 diabetes, this book provides practical advice on blood sugar monitoring, lifestyle changes, and managing the condition.
- “Pumping Insulin: Everything You Need for Success on a Smart Insulin Pump” by John Walsh, P.A., C.D.E., and Ruth Roberts, M.A.
- If you’re considering insulin pump therapy, this book offers detailed information on pump usage, blood sugar management, and optimizing insulin delivery.
- “Bright Spots & Landmines: The Diabetes Guide I Wish Someone Had Handed Me” by Adam Brown
- This book provides actionable advice for managing diabetes effectively, including tips on blood sugar monitoring, meal planning, and everyday challenges.
Summary
Monitoring glucose levels is an integral component of managing diabetes. Blood sugar, or glucose, levels can be measured using traditional blood glucose meters or advanced Continuous Glucose Monitoring (CGM) systems.
With traditional meters, you prick a finger to obtain blood samples which are then tested with strips and meters, CGMs measure continuously through sensors placed under the skin, giving real-time data, trends, and alerts that provide deeper insight into managing blood sugar.
Diabetes management involves an integrated approach. This should include appropriate medication, a balanced diet that takes into account carbohydrate intake, regular physical activity, and stress management techniques as well as blood sugar monitoring to maintain healthy levels.