Pelvic floor issues can drastically impact the quality of life for people however understanding the difference between different conditions is essential to ensure proper diagnostics and treatments. We will examine the distinctions between two of the most common problems of the pelvic floor: rectocele as well as rectal prolapse.
Rectocele and Rectal Prolapse could share risks and symptoms however, they differ in features in terms of causes, diagnosis methods, and treatments. In examining these subtleties we hope to provide those with the right information to make informed choices about their health and wellbeing.
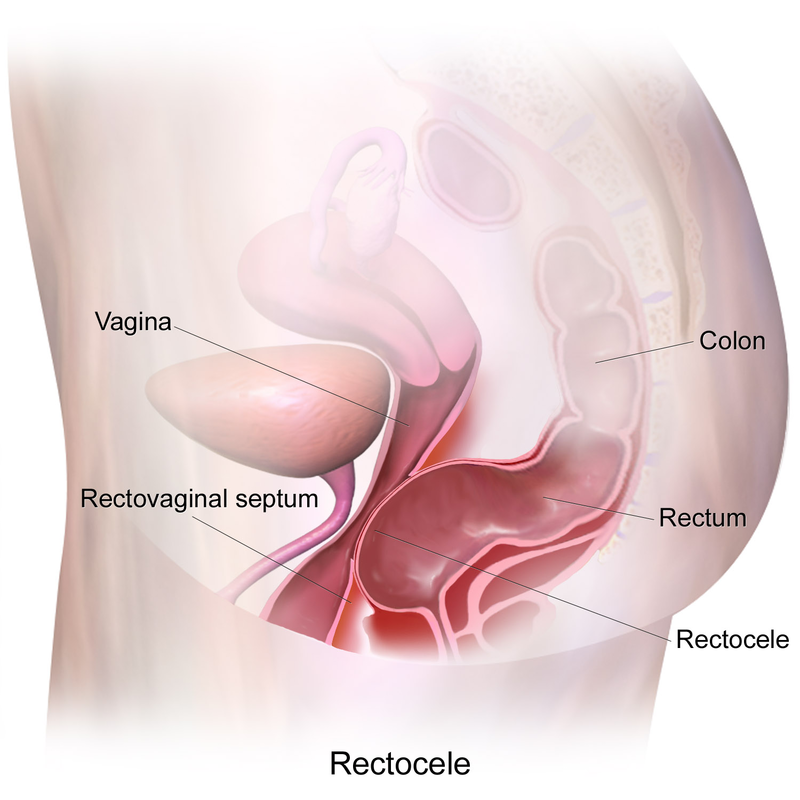
Definition of Rectocele
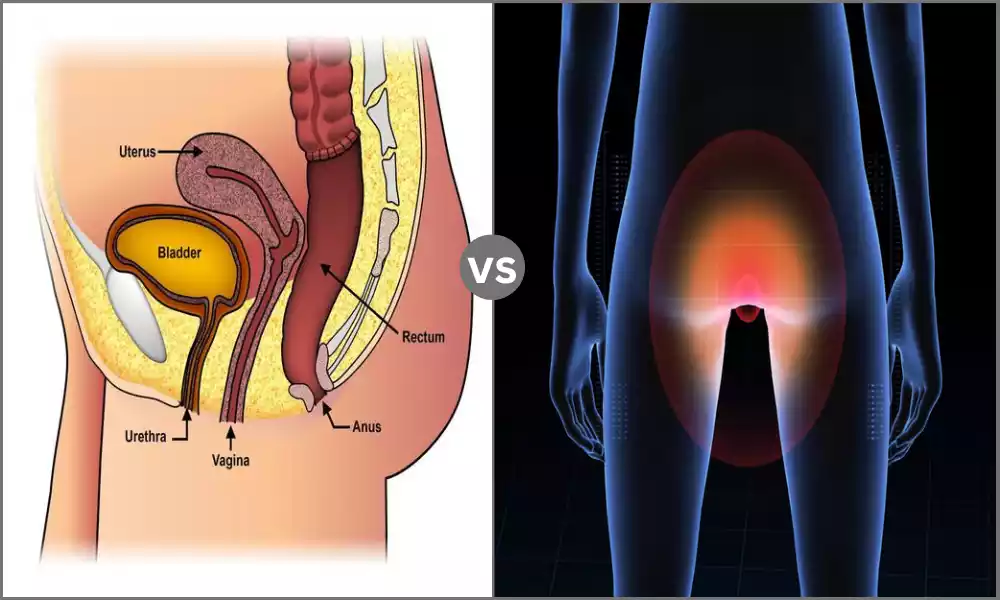
Rectocele is a medical disorder that manifests when the front of the rectum protrudes towards the back of the vagina. The condition usually develops as the muscles and tissues that support the rectum deteriorate or are damaged, resulting in an increase in the size or rupture of the septum of the rectovaginal.
Rectocele can cause various symptoms, including difficulties in the bowel, constipation, feeling of insufficient evacuation, and pelvic discomfort. It’s usually associated with pelvic floor dysfunction. It is more common among women, specifically those who gave birth vaginally or suffered pelvic trauma.
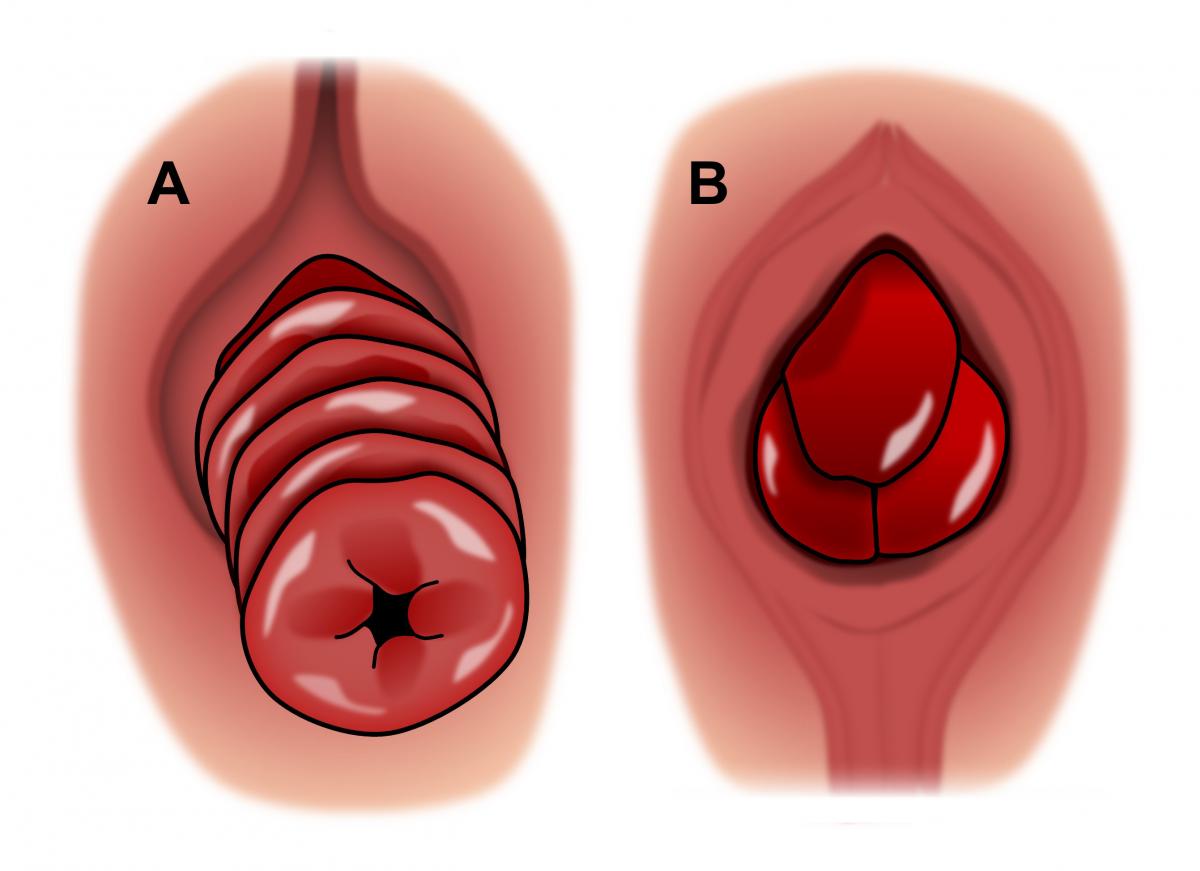
Definition of Rectal Prolapse
Prolapse of the rectal is a condition in medicine that is characterized by the protrusion or telescoping of the rectum via the anus. In this case, the rectum flips inside out and then extends beyond the body via an opening in the.
Rectal prolapse is a variable intensity, with some cases that only have a small protrusion, while other cases lead to the total externalization of the tissue. This type of condition is often caused by symptoms like blood clots in the rectal area, incontinence constipation, and pain in the area of anal.
Rectal prolapse could be a result of weak abdominal muscles that support the pelvic floor, constant strain during bowel movements, or other causes that impact the support of the anal and rectal structures. This is more frequent among older people who may frequently need medical treatment, like surgery to treat.
Comparison Table of Rectocele and Rectal Prolapse
Here’s a comparison table outlining the key differences between Rectocele and Rectal Prolapse:
| Characteristic | Rectocele | Rectal Prolapse |
|---|---|---|
| Definition | Protrusion of rectum into the vagina | Protrusion of rectum through anus |
| Location | Between the rectum and vaginal wall | Extending outside the anal opening |
| Causes | Weakened pelvic floor muscles, childbirth, straining during bowel movements, aging | Weakened pelvic floor muscles, Chronic straining during bowel movements, aging |
| Gender Predominance | Predominantly in women | Equally affects men and women |
| Common Symptoms | – Difficulty with bowel movements – Constipation |
– Rectal bleeding – Fecal incontinence – Constipation – Anal discomfort |
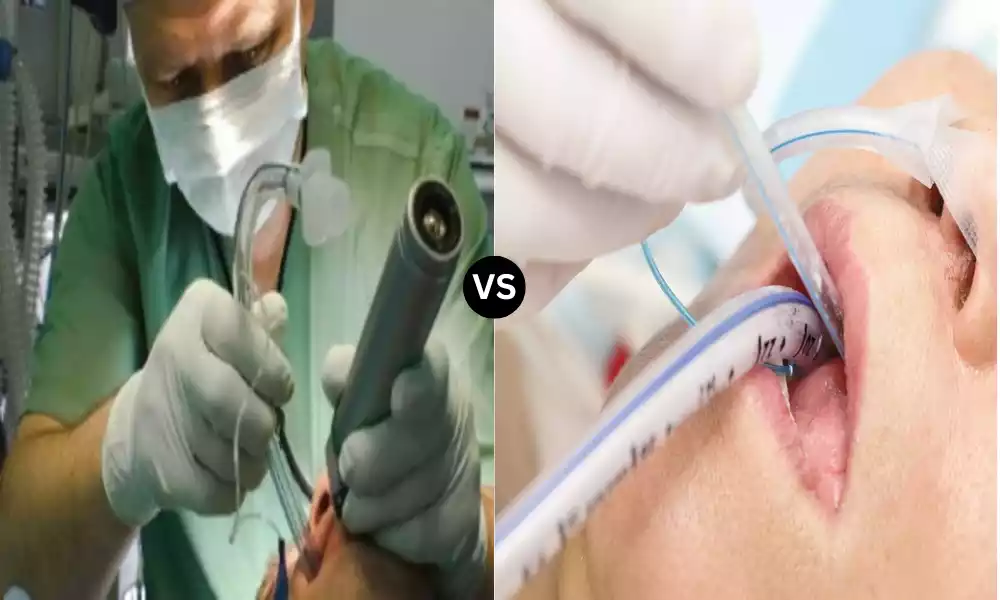
| Diagnostic Methods | – Pelvic examination – Imaging studies (e.g., MRI, defecography) | – Physical examination – Imaging studies (e.g., MRI, defecography) |
| Treatment Options | – Lifestyle and dietary changes – Pelvic floor exercises – Surgical repair if necessary | – Conservative management – Surgical interventions |
| Potential Complications | – Impact on quality of life and sexual function – Recurrence after surgery | – Rectal bleeding – Fecal incontinence- Prolapse worsening |
Please note that while this table highlights the main differences between rectocele and rectal prolapse, it’s essential to consult a healthcare professional for a thorough evaluation and accurate diagnosis if you suspect you may be experiencing symptoms related to either condition. Treatment options and outcomes can vary based on individual circumstances.
Importance of distinguishing between rectocele and rectal prolapse
The distinction between rectocele and prolapse is vital for a variety of crucial reasons:
- Accurate Diagnosis: Identifying the exact pelvic floor problem is crucial to developing a suitable treatment strategy. Rectocele-related symptoms and rectal prolapse could overlap, however, their treatment options differ greatly. A misdiagnosis could lead to ineffective or even harmful treatment.
- Tailored Treatment: Rectocele as well as rectal prolapse needs different strategies for treatment and management. Rectocele might respond well to conventional measures, whereas rectal prolapse typically requires surgical intervention. If the condition is not treated properly, it can result in unneeded medical procedures or ineffective treatment options.
- Preventing Complications: If left untreated or poorly managed the two conditions could cause complications and reduced level of living. An accurate diagnosis permits timely intervention to avoid complications like rectal bleeding or fecal incontinence. chronic discomfort.
- Information for Patients: Understanding the specific conditions can help patients. If they know that they suffer from a rectocele or rectal prolapse, they are able to make informed decisions regarding their medical care, lifestyle modifications as well and treatment options. They can also manage their expectations of the potential outcome.
- resource allocation: Resources for healthcare, like diagnostic tests, medical appointments, and surgical procedures are useful and limited. An accurate diagnosis can ensure that the resources are allocated to those who require them the most and maximize the system’s effectiveness.
- research and Data Collection: A precise diagnosis and the reporting of cases are essential to research in the field of medicine and efforts to collect data. This is in turn helping improve the understanding and treatment of diseases as well as improve the treatment methods and improve the outcomes for patients who will be treated in the future.
- Psychological Well-being: The psychological and emotional effects of pelvic floor problems shouldn’t be undervalued. Knowing the exact condition can ease stress and anxiety caused by uncertainty about the health of one’s. It can also help to develop an awareness of the control that is available in the course of one’s health.
In the end, recognizing rectocele and prolapse is essential to ensure that patients receive the appropriate and efficient treatment, avoid complications, and improve their overall health. Additionally, it benefits healthcare systems and helps to advance in the area that concerns pelvic health.
Function of the pelvic floor in maintaining bowel and urinary control
The pelvic floor performs an important role in ensuring urinary and bowel control by its many functional and anatomical components.
The pelvic floor is involved in these roles:
- Help: The pelvic floor muscles function as a hammock-like structure that lies at the pelvis’s bottom and assists in supporting the bladder and pelvis, uterus (in females), and rectum. This helps prevent these organs from falling downwards and ensures that they are in the correct position.
- Sphincteric function: The floor of the pelvis is home to two important sphincters, the urinary sphincter as well as the anal sphincter. These sphincters play a role in maintaining continence through the regulation of the release of stool and urine. If they are contracted, they block the involuntary flow of feces and urine.
- The Muscle Tone: Adequate muscle tone in the pelvic floor is vital to maintain continence. The muscles of the pelvic floor contract and relax in order to regulate an opening or closing in the urethra as well as the anus. When needed they tighten to prevent leakage and relax to allow urination as well as the movement of bowels.
- coordination: The pelvic floor muscles function in conjunction with the other muscles in the process of urination as well as defecation. For instance, when you urinate the pelvic floor relaxes so that the bladder can empty. During stool movements, it gives the support and control needed for the elimination of stool.
- Pressure Regulator: The pelvic floor assists in regulating the pressure inside the abdomen. It is a barrier to the downward pressure exerted by abdominal organs, particularly when physical activities like coughing, lifting, or sneezing raise the pressure in the abdomen. This helps prevent the leakage of feces and urine in these activities.
- Sensory Feedback: The floor of the pelvis is home to a large system of sensory nerves. The nerves transmit feedback to the brain regarding the condition of the organs of the pelvis, which includes rectal and bladder fullness. This information allows people to detect the need for urination and the need for bowel movements.
- The Posture as well as the Alignment: Correct position of pelvic muscles vital for efficient bowel and urinary control. Maintaining a healthy posture and aligning of the pelvis can help optimize the performance of the muscles.
In the end the pelvic floor functions as a crucial part of the digestive and urinary systems, which ensures the proper release of stool and urine as well as providing support to those organs of the pelvic.
A weakness or deficiency within the pelvic floor could result in urinary and urinary incontinence, as in other pelvic floor issues which highlights the importance of keeping it healthy and functioning.
Similarities Between Rectocele and Rectal Prolapse
While rectocele and prolapse, are two distinct pelvic floor conditions with distinct causes symptoms, and treatments there are some commonalities between the two:
- Pelvic Floor Dysfunction: Rectocele as well as rectal prolapse are regarded as the causes of pelvic floor dysfunction. They are caused by weakening or injury to the connective tissues and muscles that support the organs of the pelvis.
- Impact on Bowel Function: Both conditions can impact the function of the bowel. They can cause symptoms like constipation, difficulty in stool movements, or the sensation of a lack of elimination.
- Risk Factors: Certain risk factors for rectocele as well as prolapse of the rectal area overlap. This could include factors such as the aging process, chronic straining in bowel movements, as well as pelvic trauma.
- Pelvic discomfort: Individuals with both rectocele and prolapse in the rectal area may feel pelvic discomfort or a sensation of discomfort in the pelvic region.
- Potential for conservative management: In milder cases of rectocele as well as rectal prolapse, conservative strategies for management could be suggested at first. This could include diet and lifestyle changes Pilates exercises for pelvic floors (Kegel exercises) and the use of devices that support such as pessaries.
- The impact on quality of life: Both of these conditions can have a major impact on a person’s well-being, impacting the daily routine and leading to emotional distress.
It is important to remember that despite these similarities the rectocele as well as rectal prolapse remain two distinct diseases with their own distinct features and treatment strategies.
An accurate diagnosis by a medical expert is vital in determining the best treatment for each situation because they might require different approaches to deal with their specific functional and anatomical issues.
Dietary and lifestyle changes for symptom management
Lifestyle and diet changes are key factors in reducing symptoms of pelvic floor issues such as rectocele and rectal prolapse. These changes can alleviate discomfort improve the function of the bowel and help improve overall pelvic health.
Here are some diet and lifestyle suggestions to manage symptoms:
Dietary Changes:
- Fiber-rich diet: Include high-fiber foods in your diet, to help soften stool and encourage regular elimination. The best sources of fiber are whole grains as well as fruits legumes, vegetables, and nuts.
- Efficient water intake: Get plenty of water to avoid constipation and to maintain stool consistency. Hydration is crucial for a proper bowel function.
- Limit processed foods: Reduce your intake of refined and processed foods that can lead to constipation and discomfort in the digestive tract.
- Avoid foods that trigger symptoms: Identify foods that could cause symptoms to worsen like spicy foods as well as caffeine or dairy items. Eliminate or limit these foods when they cause a worsening of your condition.
- Regular meals: Maintain a regular eating plan to establish a pattern for bowel movements. Eating the same meals every day can help you to regulate the digestive tract.
Lifestyle Changes:
- Pelvic Floor exercises: Learn and perform pelvic floor exercises often referred to as Kegel exercises, to build the muscles supporting the organs of the pelvis. These exercises will help improve the control of bladder and bowel.
- Avoid straining: Avoid excessive straining in bowel movements as it may aggravate symptoms. Utilize proper methods, such as relaxing and breathing with control when sitting on the toilet.
- Maintain a healthy weight: Excess weight can cause more pressure on the pelvic floor and cause symptoms. Try to maintain an appropriate weight with healthy eating and regular physical exercise.
- Regular exercise: Engage in regular physical activity to boost overall well-being and improve the regularity of your bowel. Things like swimming, walking, and yoga are beneficial.
- Position: Maintain good posture while sitting in the toilet. Make use of a stool or footrest to lift your feet slightly to help in adjusting the rectum to facilitate elimination.
- Avoid heavy lifting: Minimize heavy lifting since it could strain your pelvic muscles. In lifting items, make sure to use the correct lifting techniques and work the core muscles.
- Scheduled Bathroom Time: Set a regular routine for your toileting. It is best to go to the bathroom every day in order to promote regularity.
- Stress Management: Chronic stress can cause pelvic floor problems. Try stress-reducing techniques like meditation, deep breathing, or mindfulness.
- Proper Toilet Practices: Take your time in the bathroom and do not rush through the process of bowel elimination. Be sure to empty your bowels as insufficient emptying could be an indication of pelvic floor problems.
- Contact a specialist: If you suspect that you may have an issue with your pelvic floor, such as rectocele, or rectal prolapse seek out a medical professional or specialist in pelvic floor. They can offer individualized advice and treatment options based on your specific condition.
It’s crucial to note that the results of diet and lifestyle adjustments can vary depending on the individual. If you experience persistent symptoms or get worse despite these changes, consult a physician to conduct a thorough assessment and treatments.
Reference Books
Certainly, here are some reference books that cover topics related to pelvic floor disorders, rectocele, rectal prolapse, and related medical conditions.
These books can provide in-depth information, guidance, and insights into these topics:
- “Pelvic Organ Prolapse: The Silent Epidemic” by Sherrie J. Palm
- This book offers a comprehensive overview of pelvic organ prolapse, including rectocele and rectal prolapse. It discusses causes, symptoms, treatment options, and personal stories from individuals who have experienced these conditions.
- “Pelvic Floor Dysfunction and Pelvic Surgery in the Elderly: An Integrated Approach” by Roger Dmochowski and David A. Ginsberg
- This reference book explores various pelvic floor disorders, including rectocele and rectal prolapse, in the context of aging and geriatric care. It provides insights into treatment strategies and considerations for older adults.
- “Pelvic Floor Disorders: Surgical Approach” by Philippe Zimmern and Eric S. Rovner
- Focusing on surgical approaches to pelvic floor disorders, this book is a valuable resource for healthcare professionals. It covers surgical techniques, outcomes, and management strategies for rectocele, rectal prolapse, and other conditions.
- “Pelvic Floor Dysfunction: A Multidisciplinary Approach” edited by Jacqueline Pretorius and Christopher Norton
- This multidisciplinary book addresses various aspects of pelvic floor dysfunction, including anatomy, assessment, and management. It provides a holistic view of conditions affecting the pelvic floor.
Conclusion
Understanding the distinction between rectocele and prolapse is crucial for accurate diagnosis and efficient treatment. The pelvic floor disorders could have some commonalities in their symptoms however they require different methods of treatment.
Changes in lifestyle and diet are beneficial for the management of symptoms in both disorders, however individualized care and guidance from a professional are essential.
If you suspect that you may have an issue with your pelvic floor consult a doctor to conduct a thorough examination and a customized treatment plan to improve your overall quality of life and health of your pelvis.