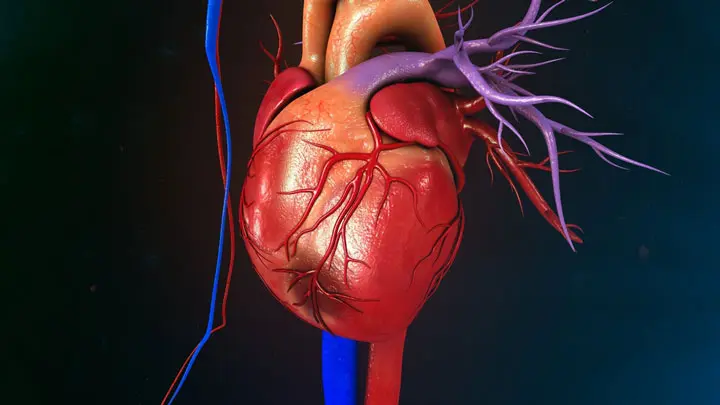
In the field of cardiovascular disease, knowing the differences between various ailments can save lives. Angina Pectoris and Myocardial Infarction are two of the diseases that can be confused because of their common symptoms of chest pain.
But they’re fundamentally different in terms of the cause as well as severity and treatment. This article will clarify the crucial differences and equip people with the necessary knowledge to recognize early signs and prompt medical treatment.
Explanation of Angina Pectoris
Angina Pectoris is an illness that causes chest discomfort or pain. It occurs because the heart muscle does not get sufficient oxygen-rich blood. The word “angina” is derived from the Latin word meaning “tightness” or “strangling,” which is a perfect description of the feeling that sufferers frequently feel.
Angina is usually provoked by physical or emotional stress. It typically is only for a brief period typically not more than 5 minutes.
There are a variety of angina:
- Stable Angina: predictable and can occur in the event of physical stress or exertion. The most common method of relief is relaxation or medications such as Nitroglycerin.
- Unstable Angina: Unstable Angina: More dangerous and unpredictable, it can occur even in a relaxed state and can last for longer. It’s a sign of the risk of a heart attack and requires prompt medical attention.
- Alternate Angina (Prinzmetal’s Angina): It is rare and can occur irregularly, most often late at night. It is caused by spasms of the coronary blood vessels.
Angina pectoris is typically thought of as an indication of an underlying heart problem, like coronary arterial disease (CAD) instead of an individual disease.
It is an alert that indicates that the heart isn’t receiving enough oxygen. It can be a sign of more severe cardiac problems so the early detection and treatment of an issue is crucial.

Explanation of Myocardial Infarction
Myocardial Infarction, also known by the name of a heart attack is an emergency medical condition that is defined by the sudden, complete obstruction of the flow of blood to a particular part of the cardiac muscle that causes irreparable damage to the tissue or even death of muscles of the heart.
In contrast to angina pectoris, in which blood flow is limited to a certain extent, myocardial infarction causes a complete blockage typically because of a blood clot that has formed within coronary arteries.
There are various types of myocardial ischemia:
- STEMI (ST-segment Elevation Myocardial infarction): This is an acute heart attack triggered by the complete blockage of the coronary artery. It is identified through the recognizable changes in ECG.
- NSTEMI (Non-ST-segment Ischemic Myocardial Infarction): This type is caused by a partial blockage, and causes significant injury to heart muscles. However, it might not display the typical ECG changes that are seen in STEMI.
- Silent Myocardial infarction: It’s an attack on the heart that happens without typical signs or with only mild symptoms, and often goes without being noticed.
Myocardial Infarction’s symptoms begin to manifest. It usually occurs quickly and is often followed by severe symptoms, such as extreme chest pain that extends into the jaw, arm, or back, breathing problems, nausea, and vomiting. Medical intervention is crucial to improve blood flow and reduce damage to the heart muscle.
The treatment is often a combination of the use of emergency procedures such as angioplasty or the placement of stents or thrombolytic therapies to break up the clot followed by medication and lifestyle modifications to control the risk factors.
The inability to quickly deal with myocardial infarction may result in serious complications, such as arrhythmias heart failure, or even cardiac arrest. So, identifying it from angina pectoris has less risk of life, and is vital to ensure proper medical treatment.
Comparison Table of Angina Pectoris and Myocardial Infarction
| Feature | Angina Pectoris | Myocardial Infarction |
|---|---|---|
| Definition | Chest pain due to reduced blood flow to the heart but no permanent damage. | Heart attack due to complete blockage of blood flow, leading to tissue death. |
| Types | Stable, Unstable, Variant Angina | STEMI, NSTEMI, Silent Myocardial Infarction |
| Symptoms | Chest pain – Shortness of breath – Fatigue | Intense chest pain – Radiating pain to arms or jaw – Nausea and vomiting – Shortness of breath |
| Causes | Partial obstruction – Emotional stress | Complete obstruction – Blood clots |
| Risk Factors | High blood pressure – High cholesterol – Smoking | Family history – Obesity – Diabetes – High cholesterol |
| Pathophysiology | Reduced blood flow causes ischemia but no tissue death. | Complete blockage leads to prolonged ischemia and tissue death. |
| Duration of Symptoms | Usually less than 5 minutes | Symptoms often last longer and intensify |
| Diagnostic Tests | ECG – Stress test | ECG – Cardiac enzymes – Imaging studies |
| Immediate Treatment | Nitroglycerin – Rest | Angioplasty and stent placement – Thrombolytic therapy |
| Long-term Management | Medications like nitrates – Lifestyle changes | Medications like beta-blockers, ACE inhibitors – Lifestyle changes – Cardiac rehabilitation |
| Complications if untreated | Can progress to myocardial infarction | Heart failure – Arrhythmias – Cardiac arrest |
| Prognosis | Generally manageable with medications and lifestyle changes | Depends on the extent of heart muscle damage and subsequent care |
Note: This table is intended for informational purposes and should not be used as a substitute for professional medical advice, diagnosis, or treatment.
Always seek the advice of your healthcare provider for any questions you may have regarding your medical condition.
Importance of distinguishing between Angina Pectoris and Myocardial Infarction
The distinction between Angina Pectoris, as well as Myocardial Infarction, is vital for a variety of reasons.
Timely Medical Intervention
- Angina Pectoris: The condition usually requires immediate evaluation and may require adjustments to medications or additional cardiac tests.
- Myocardial Infarction: requires immediate emergency intervention, such as reperfusion therapy in order to restore blood flow and reduce tissue loss.
Severity and Urgency
- Angina Pectoris: It is generally less severe and is not life-threatening immediately however, it should not be overlooked as it could be a warning signal for potential cardiac problems in the future.
- Myocardial Infarction: is a life-threatening medical emergency that demands urgent medical attention to limit the potential for fatal complications.
Treatment Strategies
- Angina Pectoris: Treatments aim to relieve symptoms and prevent further episodes, usually through medications and lifestyle modifications.
- Myocardial Infarction: The treatment is more intense, and involves surgeries, medications as well as extended hospital care.
Prognosis
- Angina Pectoris: Long-term prospects for this condition are positive if you manage it properly.
- Myocardial Infarction: The prognosis is contingent on a variety of aspects, such as the severity of tissue damage the overall health of the patient, and the speed at which the treatment process is initiated.
Prevention
- Angina Pectoris: It can be used as a wake-up alarm to initiate lifestyle changes and adjustments to medications to prevent the occurrence of a myocardial infarction.
- Myocardial Infarction: The immediate treatment of the condition is essential, however, a subsequent concentration on preventing an incident is vital and often requires more severe steps.
Long-term Health Risks
- Angina Pectoris: When not treated, the condition can progress to myocardial infarction.
- Myocardial Infarction: If it is treated increases the chance of future heart attacks, cardiac failure, and other heart complications.
Psychological Impact
- Angina Pectoris: Stress and anxiety are often felt since it could be a prelude to more serious cardiac events.
- Myocardial Infarction: is often accompanied by severe psychological trauma that requires mental and emotional health care as well as physical rehabilitation.
Knowing the distinctions between these two conditions allows for more efficient and targeted treatment, which helps lower mortality and improve the living conditions of patients affected.
Incorrect diagnosis or delay in diagnosis can result in serious negative consequences, making it crucial for health professionals and patients alike to know the difference from the other.
Reduced blood flow leads to ischemia, but no tissue death
The expression “reduced blood flow leading to ischemia, but no tissue death” is frequently related to Angina Pectoris.
What does each of these components mean:
Reduced Blood Flow
In the case of Angina Pectoris reduced blood flow is experienced because coronary vessels, that provide cardiac muscle with blood that is oxygenated are narrowed or blocked. It could be due to various factors, including atherosclerosis, blood clots, or spasms in the arteries.
Leading to Ischemia
Ischemia is the term used to describe an insufficient supply of blood to any area of the body due to constriction or obstruction in blood vessels. In the instance of Angina Pectoris, ischemia is a symptom that occurs within the heart muscle cells (myocytes). These cells are deficient in their oxygen as well as the nutrients that they require to function, triggering symptoms such as chest pain and discomfort.
But No Tissue Death
This is the primary difference between Angina Pectoris and Myocardial Infarction. With Angina Pectoris, the reduction in blood flow is generally short-term and not significant enough to result in permanent injury to heart muscles.
When blood flow is restored – either naturally or via medical intervention, the symptoms tend to ease but the muscle remains active.
However myocardial infarctions are characterized by an extended period of ischemia, which leads to irreparable tissue death. The longer that the cardiac muscle remains stripped of oxygen, the greater the amount of tissue death which can cause permanent damage.
Knowing this distinction is crucial in the diagnosis, treatment, and long-term management of the health of your cardiovascular system.
This also emphasizes the importance of seeking prompt medical attention, especially for signs that may indicate the presence of Angina Pectoris or Myocardial Infarction to stop the progress to more serious conditions.
Permanent damage to the heart muscle due to prolonged ischemia
The expression “permanent damage to heart muscle due to prolonged ischemia” is often related to Myocardial infarction which is also known as a heart attack.
Here’s an overview of what it means:
Permanent Damage to Heart Muscle
In the case of a myocardial heart attack, “permanent damage” refers to the loss of cardiac muscle cells (myocytes) which occurs when blood flow is shut off for a prolonged period.
Contrary to other cells of the body that are able to regenerate, after cardiac muscle cells cease to function and are replaced, they develop scar tissue that affects the heart’s capacity to function properly. This could lead to permanent consequences like a decrease in the heart’s output and failure or arrhythmias.
Due to Prolonged Ischemia
Ischemia refers to the insufficient flow of nutrients and oxygen to tissues because of a restricted blood flow. In the case of myocardial ischemia Ischemia is “prolonged,” meaning that the blood flow is stopped sufficiently long to cause irreparable damage.
This can be due to an entire blockage of the coronary arteries in one of them usually caused by the formation of a blood clot in the ruptured plaque of atherosclerosis.
The longer ischemia remains with no treatment greater the heart area that is affected, which could cause greater injuries and complications. This is why immediate medical intervention, usually as a reperfusion therapy such as angioplasty, a stent, or a thrombolytic drug vital for limiting injury and enhancing long-term outcomes.
Recognizing the signs of myocardial ischemia and seeking medical attention immediately is vital to prevent or limit any permanent injury to heart muscles.
Treatment generally involves both urgent procedures to repair blood flow as well as longer-term lifestyle changes and medications designed to control the risk factors that are underlying and prevent further episodes.
Long-term management: Medications, lifestyle changes
Long-term treatment of heart conditions The long-term management of cardiovascular conditions, such as Angina Pectoris and Myocardial Infarction is often a combination of lifestyle modifications and medications. This is a brief overview of each one:
Medications:
- Antiplatelet Drugs: Drugs such as aspirin and clopidogrel can prevent blood clots and lower the risk of blockages that could cause further damage to coronary arteries.
- Beta-blockers: These drugs slow the heart rate as well as reduce blood pressure, decreasing the workload of the heart and assisting in preventing angina episodes.
- Nitroglycerin: often employed for both angina and post-heart attack treatment It helps to expand blood vessels, enhancing the flow of blood and easing chest pain.
- Statins: The medications lower cholesterol levels, decreasing the possibility of plaque buildup in arteries, and subsequently heart-related issues.
- ARBs, also known as ACE Inhibitors: These medicines aid in lowering blood pressure and ease stress on the heart, particularly following a heart attack.
- Antiarrhythmics: If irregular heart rhythms occur These medications can help keep an even heartbeat.
Lifestyle Changes:
- Diet: Adopting a healthy diet that is rich in vegetables, fruits whole grains, and proteins that are lean and healthy fats will help reduce blood pressure, cholesterol levels, and inflammation.
- Exercise: Regular physical exercise enhances cardiovascular fitness, assists in maintaining a healthy weight, and helps strengthen the heart.
- Quitting Smoking: Stopping smoking cigarettes is among the most effective methods to lower the chance of developing heart-related problems.
- The Management of Stress: Techniques such as deep breathing, meditation, yoga, and meditation can help you manage stress and minimize its effects on the heart.
- The Management of Weight: Maintaining and achieving an ideal weight will reduce the strain on your heart and reduce the risk of developing various heart diseases.
- Med Adherence: Following prescription medications in a consistent manner as instructed by a physician is vital to managing symptoms and preventing complications in the future.
- Regular check-ups: Regular visits to your healthcare professional aid in monitoring progress, adjusting medications as needed, and detecting any possible problems early.
Combining lifestyle and medication modifications can dramatically enhance the long-term outlook of people suffering from cardiovascular diseases. It is important to keep in mind that treatment plans must be individualized to each person’s specific health condition as well as risk factors and medical background.
Consultation with a medical professional is vital to devise an efficient and customized management plan.
Reference Books
Certainly, here are some reference books that provide comprehensive information about cardiovascular diseases, including Angina Pectoris and Myocardial Infarction. Please note that medical literature can evolve, so it’s a good practice to check for the most recent editions or updated sources:
- “Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine” by Douglas P. Zipes, Peter Libby, Robert O. Bonow, and Eugene Braunwald
- This renowned textbook provides an in-depth understanding of cardiovascular diseases, including detailed coverage of various conditions, their pathophysiology, diagnosis, and management.
- “Cardiology Secrets” by Glenn N. Levine
- This book offers concise and practical information about a wide range of cardiology topics, making it accessible for medical students, healthcare professionals, and anyone interested in learning about heart conditions.
- “The Washington Manual of Cardiology Subspecialty Consult” by Phillip S. Cuculich and Emily C. O’Brien
- This manual offers a practical guide to diagnosing and managing cardiovascular conditions, providing insights into different aspects of cardiology subspecialties.
- “Cardiovascular Physiology” by David Mohrman and Lois Heller
- Understanding the underlying physiology of the cardiovascular system is essential to grasp the mechanisms behind conditions like Angina Pectoris and Myocardial Infarction. This book offers a comprehensive overview of cardiovascular physiology.
- “The ESC Textbook of Cardiovascular Medicine” by A. John Camm, Thomas F. Lüscher, and Gerald Maurer
- Published by the European Society of Cardiology, this textbook covers a wide spectrum of cardiovascular diseases, making it a valuable resource for up-to-date information.
Conclusion
The distinction difference between Angina Pectoris and Myocardial Infarction is vital for prompt and appropriate medical attention. Angina Pectoris is caused by chest pain because of decreased blood flow and can be an indicator of the possibility of heart problems.
On the other hand, Myocardial Infarction, or heart attack, is the permanent injury to the heart muscle from an indefinite obstruction in blood circulation. Understanding the different signs and causes, as well as urgency and treatment options is essential to ensuring the highest possible results.
If it’s about managing symptoms using medication and lifestyle changes or dealing with emergency situations swiftly knowing these conditions allows individuals to control their heart health and seek medical attention whenever needed.